Review Paper - Current Pediatric Research (2018) Volume 22, Issue 3
Whats going on pediatric obesity: Report from Italy.
Luca Pecoraro1, Angelo Pietrobelli1,2, Marco Zaffanello1, Giulia Paiola1, Pasquale Comberiati1, Giorgio Piacentini11Pediatrics, Department of Surgical Sciences, Dentistry, Gynecology and Pediatrics, University of Verona, Verona, Italy.
2Pennington Biomedical Research Center, Baton Rouge, LA, USA.
- Corresponding Author:
- Marco Zaffanello
Department of Surgical Sciences
Dentistry, Gynecology and Pediatrics, University of Verona
Verona, P.le Stefani, 1, Verona, 37126, Italy
Tel: +39 045 8127121
E-mail: marco.zaffanello@univr.it
Accepted date: July 27, 2018
Abstract
Objective: It is a report of childhood obesity in Italy. Italian Statistic Data Center (ISTAT), reports that 24% of the subjects between 6 to 17 yrs of age are overweight, with higher percentage in the South of Italy. The same report underlines that one million of subjects between 6 to 11 yrs of age are overweight or obese. Consequently, among European countries, Italy is at the top level in term of pediatric obesity incidence and frequency. Methods: A systematic literature search was conducted. All quantitative and qualitative studies of Italian pediatric samples reporting results on childhood obesity were included. 7 articles were found. These studies are focused on the prevalence of overweight and obesity, adolescent lifestyle, the correlation between education attainment, eating patterns, physical activity, socioeconomic status, individual Body Mass Index (BMI) and early-life risk factors. Results: Articles analysed showed higher prevalence of overweight and obesity in the south of Italy; overweight and obese adolescents have wrong lifestyles: they skip breakfast, drink soft and sweet beverages and energy drinks; we found also a strong relationship between education of adolescents and parents, eating patterns, and physical activity and individual BMI. Early risk factors of cardiovascular diseases are related to childhood obesity, too. Conclusion: Concerted public health efforts need to achieve the healthy objectives for obesity and nutrition and to fight the childhood obesity epidemic. These efforts are definitely focused both on obese children and children at highly risk of being obese.
Keywords
Obesity; Children; Prevention; Italy; Nutrition; Physical activity.
Introduction
Italy, among European countries, is at the top level in term of pediatric obesity incidence and frequency. Italian Statistic Data Center (ISTAT), reports that 24% of the subjects between 6 to 17 yrs of age are overweight, with higher percentage in the South of Italy. The same report underlines that one million of subjects between 6 to 11 yrs of age are overweight or obese. It is well known that 30% to 60% of overweight or obese children will be overweight or obese in adult age [1]. Although, it is important to underline that since 2008, the number of children between 8 and 9 yrs of age that are overweight or obese decreased slightly. Specifically, if we consider overweight and obese children aged 8-9 yrs old, in 2012 22.1% were overweight compared to 23.2% in 2008-09 (1.1%), and 10.2% were obese, while in 2008-09 the amount was 12% (1.8%) [1].
The role of this report is to describe incidence of prevalence of overweight and childhood obesity in Italy and understand the reasons for the high rates of these statistical data (Table 1).
| 2008 | 2012 | Percentage Difference | |
|---|---|---|---|
| Overweight | 23.2% | 22.1% | 1.1% |
| Obesity | 12% | 10.2% | 1.8% |
Table 1: Percentage prevalence trends about overweight and obesity in Italy
Methods
Authors performed a systematic literature search through the Cochrane Library and Medline/PubMed databases. All quantitative and qualitative studies of Italian pediatric samples reporting results on childhood obesity since 2010 were included. 7 articles were found. Five parameters were considered: the prevalence of overgrowth and obesity in north, central and south of Italy, wrong lifestyles of Italian adolescent, the correlation between education attainment, eating patterns, physical activity, socioeconomic state and individual Body Mass Index (BMI), education of the parents, early life risk factors.
Studies were excluded made before 2010 and regarding other countries pediatric samples.
Results
Prevalence of overgrowth and obesity in north, central and south of Italy
There is a major prevalence of overweight and obesity in the south of Italy with percentages 3-6% higher rather the national average for overweight and 2-3 higher rather this average for obesity.
This event can be related the lesser ability of southern doctors to advise to an overweight or obese patient to lose weight. The evidence is that doctors of south of Italy have less consideration of this problem [2].
Lifestyle factors
There is a relationship between childhood overweight/ obesity and several lifestyle factors in a sample of Italian adolescents. The main findings of this study are that adolescents that skip breakfast, drink soft and sweet beverages and energy drinks have higher odds of being overweight or obese [3]. This consideration accords with the knowledge that in European children and adolescents, having breakfast is associated with a lower BMI and with a reduced risk of becoming overweight or obese [4]. Specifically, both childhood and adulthood had a larger waist circumference and higher fasting insulin, total cholesterol and LDL cholesterol concentrations than those who had breakfast regularly [5].
The role of education attainment on individual body mass index (BMI), eating patterns, and physical activity
There is a peculiar pronounced negative correlation between body weight and socioeconomic conditions: poorly educated Italian women are 3 times more likely to be overweight than better-educated women, and poorly educated men are 1.3 times more likely to be overweight than bettereducated men. Moreover, a recent expansion of unhealthy lifestyles, especially for poor socioeconomic groups, has resulted in a sharp increase in body weight of Italian children, who show the highest prevalence of being overweight among all European countries [6].
Education has an impact on individual BMI, Eating patterns, physical activity have an impact on education.. Specifically, completion of lower secondary education, especially in the presence of strong socioeconomic inequalities, has a significant positive impact on its reduction, containment of calorie consumption, and promotion of physical activity [7].
The role of parent’s education level
There is a correlation between parental education level and proper estimation of the child weight status, too. Either a low or medium (p<0.005) education level of parents has been reported to strongly correlate with an inadequate evaluation of the child weight status not only for mothers but also for fathers [8].
Early‑ life risk factors
A significant linear regression was found between birth weight and the child Waist Circumference (WC) and Waistto- Height ratio (W/H), determinants of child central obesity [8]. Remarkably, the child WC and W/H significantly correlate with birth weight even after adjusting data for age and gender, suggesting a link between high birth weight and subsequent unfavorable adiposity distribution during childhood and adolescence, a possible consequence of a predominantly genetic origin.
An important role is played by breastfeeding as a protective factor. Among overweight/obese children, the prevalence of breastfeeding was lower compared to thin/ normal children [9].
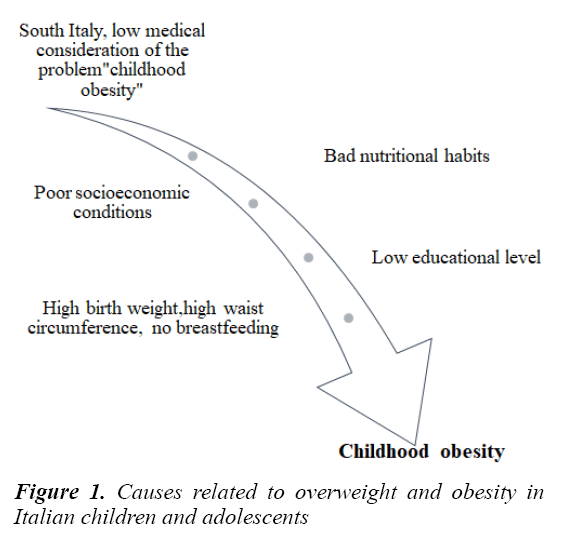
Summary of the causes related to overweight and obesity in Italian children and adolescents is showed in Figure 1.
Discussion
The importance to put the attention both on obese children and children at highly risk of being obese
The improvement of lifestyle factors and adolescent and parents' educational level are tasks of Italian Minister of Health and Instruction and refer to overweight or obese children and adolescents present in Italy. This is a good strategy, but the limited success of preventive programs adopted until this moment imposes to put the attention both on obese children and children at highly risk of being obese. So, across the discovery of the importance of understanding risk factors for pediatric obesity, it is mandatory to identify children at highly risk of being obese and to predispose early intervention strategies. They were realized by the Mediterranean Nutrition Group (MeNu Group), a working group of researchers from the Mediterranean region willing to contribute through their research or medical activities to the prevention of pediatric obesity. This group elaborated a proposal of 10 good practices to help prevent obesity in the first 1,000 days [10].
Both mother and father behavior matter
A balanced diet with adapted excessive fat and protein intake and favoring fruits and vegetables is recommended for both parents during conception period and pregnancy. Furthermore, overweight/obese women who plan to be pregnant should reduce weight before conception [10]. In fact, different epigenetic mechanisms are elicited by dietary factors in early critical developmental ages that are able to affect the susceptibility to several diseases in adulthood. Both maternal under- and over-nutrition may interact with genes controlling lipid and carbohydrate metabolism, thus inducing alterations in epigenetic regulations [11,12]. Specifically, several prenatal risk factors related to mother's behaviour during pregnancy are consistently associated with later childhood overweight: higher maternal prepregnancy, mother's BMI, maternal excess gestational weight gain, prenatal tobacco exposure, gestational diabetes and inappropriate bottle use [11-13].
Before and during pregnancy, at birth and during early life, body composition measurements are crucial to monitor growth
Pediatric obesity is a condition of excess body fat accumulation and a clinical diagnosis of obesity should based on an accurate direct or indirect measure of total body fat [10]. Independent of total adiposity, an upper body, central or visceral distribution of fat is believed to be a risk factor for poor health in both adults and children. Accurate measurement of total and regional body fat is fundamental in order to detect as early as possible whether a given child is deviating from normal values or trends. A lot of studies used body mass index that could be defined a surrogate measure of adiposity. Differences in body weight are only in part related to differences in body fatness. In fact it is adiposity, rather than body weight per se, that may underlie the major health comorbidities related with obesity even in childhood. So, it is important to quantify total body and regional adiposity, and map adipose tissue distribution in order to evaluate metabolic risk factors in children, using PEA POD (an Air Displacement Plethysmography used in subjects between 1 and 8 kg) and Dual X-ray absorptiometry (DXA) (infants larger than 8 kg) [14].
Exclusive breastfeeding for the best start in life
Breastfeeding may contribute to obesity prevention. Thus exclusive breastfeeding is recommended at the beginning of life until 6 mon. When breastfeeding is not possible, the use of an infant follow-on formula should be privileged as it will bring more fat of good quality and limit protein intake. In that respect, cow’s milk should be avoided at least during the first year of life [10]. A longer duration of breastfeeding is associated with a larger decrease in risk of overweight. Specifically, the duration of breastfeeding is inversely and linearly associated with the risk of overweight: the risk of overweight was reduced by 4 percent for each month of breastfeeding. This effect lasted up to duration of breastfeeding of 9 mon and was independent of the definition of overweight and age at follow-up [15]. This finding can be related to the evidence that breast milk provides a moderate amount of calories and nutrients for infant, such as sugar, water, protein and fat. Moreover, the composition of breast milk changes with time and the mother’s diet. In contrast, formula feeding provides higher levels of fat and protein than the baby’s needs. Higher protein and fat intake in early childhood have been associated with adiposity. Moreover, breast milk rather than other milk contains bioactive substances such as leptin and ghrelin, which can influence the proliferation and differentiation of the infant’s adipocytes. Thus, breast milk is rich in effective ingredient with higher nutritional value [16]. Brestfeeding influences adult life, too. In fact, it decreases the odds of type 2 diabetes and by 13% the odds of overweight/obesity. No associations were found for total cholesterol or blood pressure [17].
Begin weaning between 4 and 6 months
Complementary feeding timing and practices can have direct or later consequences on health with possible longterm effects related to obesity. 4 to 6 mon of age is the optimal window to introduce complementary feeding and build the child current and future food repertoire. Then, until 1 year of age, breast milk or follow-on formula must remain the main source of feeding and cow’s milk must be avoided [10]. The timing of the introduction of complementary foods has no clear association with childhood obesity, although very early introduction of solid foods (<4 mon of age) may result in an increase in childhood BMI [18]. An early introduction to complementary foods increases the susceptibility of individuals to an obesogenic environment. This event can be related to an increased intake of calories and protein during infancy (predictive of greater weight gain and percent body fat in childhood), the likelihood of premature termination of breastfeeding (introducing solid food before 4 mon was associated with an almost 6-fold increase in the risk of obesity among 3-year-old formula-fed infants, but not in breastfed infants), alterations in gut flora (leading to epigenetic modification of metabolism genes) [19]. High intakes of energy and protein, particularly dairy protein, in infancy could be associated with an increase in BMI and body fatness. During weaning, it is not important the type of food introduced, but the time when they are introduced; so, adherence to dietary guidelines during weaning is recommended [20].
Fruits and vegetables liking begins early
Complementary diet must embrace all food categories with an emphasis on vegetables and fruits. Daily variety, diversity in a meal and repeated exposure up to 8 times are efficient strategies to increase acceptance of foods not well accepted at first. Promoting healthy foods as part of usual meals during complementary feeding is important as eating habits learned in childhood are likely to continue through life. There is no need to add sugar and salt and sugary fluids (juices, soda, infusion…) should be avoided during complementary feeding and onwards [10]. Recent evidence shows that healthy eating habits such as high fruit and vegetable intake, reduced soft drink consumption and eating breakfast regularly are the key elements to prevent chronic disease and promote health. This is a very important aspect: several studies have shown that health risk behaviours such as eating habits established in childhood and adolescence tend to be maintained into adulthood. A meta-analysis published by Levin shows that Italian 15-year-old have worse behaviour rather than European average [21,22]. A successful management of childhood obesity requires holistic interventions that not only promote healthy diets, nutritional education, physical activity promotion, community support, change of school policies to promote healthy nutrition. The age of the children may be another factor that affects the impact of the interventions. Children develop the majority of their food preferences around the ages of 2 and 3 yrs, and food introduced after the age of four is more likely to be disliked than liked. This may reflect older children’s ability to understand the nutritional advice better and are able to exercise willpower over their food choices than younger children, for example, choosing to eat foods that they do not necessary enjoy the taste of because they know they are healthy [23].
Respect the child appetite
Babies know to recognize their hunger and satiety cues but they lose this ability, probably due to external influences. Avoid coercive “clean your plate” feeding practices. Adapt portions of food and offer foods to the child in response to their feeling of hunger and not to use foods as reward for good behavior [10]. Beyond parent's behaviour, a lot of early life characteristics are associated with appetite related eating behaviors. Specifically, eating behaviors develop early in life and result from interplay between genetic predisposition, natural food responses and preferences, and environmental influences. About the familial environment, children who tend to overeat are more likely to be male, live in a single parent home, and have both parents overweight or obese. About lifestyles, more sedentary lifestyles at 4 yrs old were associated with higher appetite restraint and appetite disinhibition scores later in childhood. Accordingly, emotional and external eating has already been associated with increased screen time, which could be explained by an association between screen time and less attentive eating. A last consideration about the type of food first consumed at complementary feeding significantly predicted eating behaviors in the third infancy. The absence of repeated exposure to vegetables and unsweetened fruits early in life may even induce a low capacity to taste different flavours later in life, consequently promoting picky eating. Starting from the evidence that it is not possible to act towards genetic predisposition, it is necessary to focus the attention on parents' behaviour. They influence child weight through interactions that shape the development of child eating behaviors. It is known that poor self-regulation of eating in children increases the risk of childhood obesity. While most children appear to possess an inborn ability to self-regulate food intake in responses to the energy content of foods consumed, some children show poor patterns of self-regulation [24,25].
Control animal Protein Intake
Several findings substantiate a recommendation to limit animal protein intake in early life to reduce the risk of an early adiposity rebound, which indicates an increased obesity risk. To meet the child nutritional requirements after 12 mon, growing-up milk should be preferred to cow’s milk in order to limit protein intake and meet essential fatty acids and iron needs [10]. Starting from the evidence that that early weight gain is the best predictor of later childhood overweight, a randomized controlled trial confirms the hypothesis that higher protein intake in infancy leads to more rapid length and weight gain in the first 2 yrs of life. Limiting the protein content of infant and follow-on formula and, more generally, the dietary protein intake during infancy, might constitute a potentially important approach to reducing the risk of childhood overweight and obesity [26].
Assure adequate qualitative fat intake
The restriction of fat intake during early life seems to increase the susceptibility to develop overweight. Thus, the intake of adequate fat containing essential fatty acids should be promoted. low-fat products should be avoided from weaning period and onwards [10]. There is an association between early low fat intakes with adults being overweight and having high serum leptin. However, it was shown that infants that were exclusively or predominantly breast fed and consumed higher amounts of fat grew more rapidly in weight and length during the first months, but appeared to falter thereafter. There aren't deleterious consequences of high consumption of lipids during the first two years of life [27].
About Omega-3 and omega-6 fatty acids, particularly docosahexaenoic acid (DHA), they are essential fatty acids (EFAs) as they cannot be produced by the human body. They are known to play an essential role in the development of the brain and retina. Specifically, the brain is composed of large amounts of both DHA and AA. During the third trimester of pregnancy and first year of life, the brain grows rapidly and an adequate supply of both of these fatty acids is thought to be essential for optimal development. DHA is also a major component of the retina and thus affects visual acuity. There is an association between maternal omega-6 and omega-3 fatty acid status and birth weight, length and body composition of the child during early infancy. It has been hypothesized that high omega-6 to omega-3 status raises tissue AA, which increases prostacyclin production and, in turn, stimulates signaling pathways implicated in adipogenesis. As breast milk is one of the best sources of Linoleic acid (ALA) and DHA, breastfed infants are less likely to be at risk of insufficient intakes than those not breastfed. Fatty acid supplementation showed improvement in cognition or development in infants. These benefits were more pronounced in undernourished children and apparently healthy children from low socioeconomic status. The importance of providing an appropriate supply of omega-3 and omega-6 fatty acids, especially DHA and AA, is likely to be relevant in early childhood in these settings because both fatty acids continue to accumulate most rapidly in brain gray matter during the first 2 yrs of life. In older children above 2 yrs of age, no benefits of omega-3 fatty acids were observed on growth or cognition [28].
Let’s enjoy adapted meals in family
Parents have a model role in feeding. They should be an example for the child, make meals a moment of pleasure taken in family, including breakfast, while respecting the young child specific nutritional needs, with TV and all other screens turned off [10]. Dietary behaviours develop in the early years of life. Young children share their food environment with parents and siblings. This shared “family food environment” is the most important influence on children’s dietary intakes and therefore, provides an important target setting for improving diets and eating behaviours among children. The family food environment is where food behaviours are initially developed and reinforced. It incorporates a cluster of potential parental influences on children’s diets, which offer opportunity for influencing dietary intakes among young children, particularly during shared family mealtimes (breakfast, lunch, dinner and snacks). About eating location, it is considered to be an important characteristic of family meals, with eating while sitting at a table reported to be associated with younger children’s increased fruit and vegetable consumption, appropriate portion sizes, social engagement between parents and children, and reduced access to TV viewing during meals [29]. Specifically, 62% of children aged 8 to 12 yrs reported daily TV viewing, spending on average 2.21 h per day watching TV. American Academy of Pediatrics’recommendation is that parents should limit children's total media time to <2 h of programming per day, screen-time (i.e., TV viewing, computer/video/handheld game playing). TV-viewing for more than 2 h per day is associated with adverse health outcomes. For school-aged youth this include the risk of excess weight gain, poor fitness levels, adverse psychosocial outcomes, and decreased academic achievement. TV-viewing habits during childhood are also associated with obesity and poor fitness in adulthood, suggesting that interventions that aim to reduce sedentariness should start early in life. The recently released recommendations from the Community Preventive Services Task Force on Reducing Children's Recreational Sedentary Screen Time found that family based social support was the most common component of effective interventions for children aged 13 yrs or younger, drawing attention to the critical role of family and parent support to influence children's sedentary screen time behaviour [30]. Specifically, it gives some advice: not having a TV in the child’s bedroom, turning the TV off when nobody is watching, and not eating snacks in front of the TV. Empowering parents with specific strategies to reduce their child’s media consumption could help them to positively enhance their child's health and to promote healthier lifetime leisure habits [31].
Encourage physical activity and good sleep
Environmental and psycho-social factors also have a supporting role. Preventive interventions consisting in letting kids move and encouraging physical activities can contribute to the prevention of pediatric obesity and obesity later on. Furthermore, a child has to get sleep sufficiently as short sleep duration may be associated with increased risks of developing obesity in childhood and adulthood [10]. Combinations of Physical Activity (PA), Sedentary Behaviour (SB), and sleep are associated with important health indicators in children and youth aged 5–17 yrs. Children and youth with a combination of high PA/high sleep/low SB (best combination) had favourable measures of adiposity and cardio metabolic health, when compared with those with a combination of low PA/low sleep/high SB (worst combination). These findings suggest that there may be synergistic benefits to achieving optimal levels for multiple movement behaviours [32]. If it is easy to understand the link between absence of physical activity is related to childhood obesity, it is less immediate to understand the relationship between sleep deprivation and weight gain and the development of obesity. The term ‘‘lack of sleep’’ generally refers to an insufficient amount of sleep for optimal functioning. Sleep deprivation as a contributor to weight gain and obesity has emphasized the need to include sleep hygiene in health assessments and lifestyle modification interventions. Assessing general sleep hygiene (sleep duration, quality, and timing) does not need to be long and complicated and can efficiently be incorporated into any health and lifestyle assessment. Rules about bedtime in the household and making sure that gadgets are out of the child’s bedroom are important in the promotion of healthy sleep hygiene. In this contest, American Academy of Pediatrics recommends that parents remove TV sets and internetconnected electronic devices from children’s bedrooms. Sleep is not a ‘‘waste of time’’, and public health efforts should aim to better promote a good night’s sleep for overall health [33-35].
Conclusion
Italy is at the top level in term of pediatric obesity incidence and frequency. This aspect is related with wrong lifestyles of Italian adolescent, poor education attainment of the children and their parents and early life risk factors. Preventive programs adopted until this moment had limited success; they was directed mainly on the medical profession and they didn't involve the rest of society (family, school, media, institutions, commercial companies). The Italian Minister of Health recently presented a “policy maker” where is mandatory a commercial spot control, taxes on soft drinks, clear information on the labels, together with support of promotion of healthy diet and regular physical activity. So, it is mandatory to put the attention both on obese children and children at highly risk of being obese. Concerted public health efforts are needed to achieve the healthy objectives for obesity and nutrition and to fight the childhood obesity epidemic.
References
- https://www.istat.it/it/archivio/214228
- http://www.epicentro.iss.it/passi/dati/sovrappeso.asp
- Galfo M. Overweight/obesity and lifestyle factors among Italian adolescents: The ALIADO study. Minerva Ped. 2016;22.
- Szajewska H, Ruszczynski M. Systematic review demonstrating that breakfast consumption influences body weight outcomes in children and adolescents in Europe. Crit Rev Food Sci Nutr. 2010;50:113-19.
- Smith KJ. Skipping breakfast: Longitudinal associations with cardiometabolic risk factors in the Childhood Determinants of Adult Health Study. Am J Clin Nutr. 2010;92:1316-25.
- http://www.oecd.org/els/health-systems/obesity-and-the-economics-of-prevention-9789264084865-en.htm
- Staiger D, Stock J. Instrumental variables regression with weak instruments. Econometrica 1997;65: 557-86.
- Atella V. Body weight, eating patterns, and physical activity: The role of education. Demograph. 2014;51:1225-49.
- Brambilla P, Bedogni G, Heo M, et al. Waist circumference-to-height ratio predicts adiposity better than body mass index in children and adolescents. Int J Obes (Lond). 2013;37:943-46.
- Parrino C. Influence of early life and parental factors on childhood overweight and obesity. J Endocrinol Invest. 2016;39:1315-21.
- Pietrobelli A, Agosti M, Zuccotti G, The MeNu Group. Putting the barker theory into the future: Time to act on preventing pediatric obesity. Int J Environ Res Public Health. 2016;13.
- Eli K, Sorjonen K, Mokoena L, et al. Associations between maternal sense of coherence and controlling feeding practices: The importance of resilience and support in families of preschoolers. Appetite. 2016;105:134-430.
- Canani RB, Costanzo MD, Leone L, et al. Epigenetic mechanisms elicited by nutrition in early life. Nutr Res Rev. 2011;24:198-205.
- Woo-Baidal JA, Cheng ER, Blake-Lamb TL, et al. Risk factors for childhood obesity in the first 1,000 days: A systematic review. Am J Prev Med. 2016;50:761-79.
- Fields DA, Demerath EW, Pietrobelli A, et al. Body composition at 6 months of life: Comparison of air displacement plethysmography and dual-energy X-ray absorptiometry. Obesity. 2012;20:2302-06.
- Harder T. Duration of Breastfeeding and Risk of Overweight: A Meta-Analysis. Am J Epidemiol 2005;162:397-403.
- Yan J, Liu L, Zhu Y, et al. The association between breastfeeding and childhood obesity: A meta-analysis. BMC Public Health. 2014;14:1267.
- Hinkle SN, Schieve LA, Stein AD, et al. Association between maternal prepregnancy bod mass index and child neurodevelopment at 2 years of age. Int J Obes. 2012;36:1312-19.
- Horta BL, Victoria CG, World Health Organisazation. Long-term effects of breastfeeding: A systematic review. World Health Organization 2013.
- Wang J, Wu Y, Xiong G, et al. Introduction of complementary feeding before 4 months of age increases the risk of childhood overweight or obesity: A meta-analysis of prospective cohort studies. Nutr Res. 2016;36:759-70.
- Pearce J, Langly-Evans SC. The types of food and feeding style introduced during complementary feeding and risk of childhood obesity: A systematic review. Int J Obes. 2013;37:477-85.
- Pereira-da-Silva L, Rêgo C, Pietrobelli A. The diet of preschool children in the mediterranean countries of the European Union: A systematic review. Int J Environ Res Public Health. 2016;13.
- Levin KA, Kirby J, Currie C, et al. Trends in adolescent eating behaviour: A multilevel crosssectional study of 11-15 year olds in Scotland, 2002-2010. J Public Health. 2012;34:523-31.
- Bourke M, Whittaker PJ, Verma A. Are dietary interventions effective at increasing fruit and vegetable consumption among overweight children? A systematic review. J Epidemiol Community Health. 2014;68:485-90.
- Albuquerque G, Severo M, Oliveira A. Early life characteristics associated with appetite-related eating behaviours in 7-year-old children. J Pediatr. 2017;180:38-46.
- Silva GK, Power TG, Fisher JO, et al. Latina mothers' influences on child appetite regulation. Appetite. 2016;1:200-7.
- Koletzko B, von Kries R, Closa R, et al. European childhood obesity trial study group. Lower protein in infant formula is associated with lower weight up to age 2 years: A randomized clinical trial. Am J Clin Nutr. 2009;89:1836-45.
- Rolland-Cachera MF, Akrout M, Péneau S. Nutrient intakes in early life and risk of obesity. Int J Environ Res Public Health. 2016;13.
- Huffman SL, Harika RK, Eilander A, et al. Essential fats: How do they affect growth and development of infants and young children in developing countries? A literature review. Matern Child Nutr 2011;7:44-65.
- Kubik MY, Gurvich OV, Fulkerson JA. Association between parent televisionviewing practices and setting rules to limit the television-viewing time of their 8- to 12-year-old children, Minnesota, 2011–2015. PrevChronic Dis. 2017;14:160235.
- Litterbach EV, Campbell KJ, Spence AC. Family meals with young children: an online study of family mealtime characteristics, among Australian families with children aged six months to six years. BMC Public Health. 2017;17:111.
- Escobar-Chaves SL, Markham CM, Addy RC, et al. The fun families study: Intervention to reduce children’s tv viewing. Obesity. 2010;18;99-101.
- Saunders TJ, Gray CE, Poitras VJ, et al. Combinations of physical activity, sedentary behaviour and sleep: relationships with health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41:283-93.
- Chaput JP. Is sleep deprivation a contributor to obesity in children? Eat Weight Disord. 2016;21:5-11.
- Ministry of Health. Global action plan of the who For prevention and control of non-transmissible diseases 2013-2020. 2010;1-55.