Research Article - Biomedical Research (2017) Volume 28, Issue 21
Vitamin D levels and vitamin D receptor expression in children with primary nephrotic syndrome
Xingxing Zhang1, Xiaochuan Wu1*, Fujuan Wang1,2, Zhuwen Yi1 and Yan Cao1
1Department of Pediatrics, the Second Xiangya Hospital, Central South University, Changsha, Hunan 410011, PR China
2Department of Pediatrics, Shanghai Jiao Tong University Affiliated Sixth People’s Hospital, PR China
- *Corresponding Author:
- Xiaochuan Wu
Department of Pediatrics
The Second Xiangya Hospital
Central South University
Changsha, Hunan 410011, PR China
E-mail: xiaochuanwu@mail.csu.edu.cn
Accepted date: September 20, 2017
Abstract
Objective: To explore the significance of vitamin D and vitamin D receptor expression in the occurrence and outcome of primary nephrotic syndrome.
Methods: Serum 25-hydroxy vitamin D3 levels were determined in 90 children with primary nephrotic syndrome. Renal vitamin D receptor expression was detected in 36 children with primary nephrotic syndrome.
Results: Serum 25-hydroxy vitamin D3 levels in the 90 children with primary nephrotic syndrome were significantly lower compared with the control group (P<0.05). Serum 25-hydroxy vitamin D3 levels were lower in the initial onset and non-remission groups than in the remission group (P<0.05). Vitamin D receptor expression in kidney tissue in primary nephrotic syndrome children was significantly lower than that in the control group (P<0.05), significantly lower in the focal segmental glomerulosclerosis group than that in the mesangial proliferative glomerulonephritis and minimal change disease groups (P<0.05), and lower in the mesangial proliferative glomerulonephritis group than that in the minimal change disease group (P<0.05).
Conclusions: Decreased 25 (OH) D3 levels and altered vitamin D receptor expression in primary nephrotic syndrome children may be associated with the occurrence and outcome of primary nephrotic syndrome.
Keywords
Calcitriol, Cholecalciferol, Nephrotic syndrome, Vitamin D3 receptors
Introduction
Primary Nephrotic Syndrome (PNS) is a common pediatric disease. The annual incidence is estimated at 2-4 cases per 100,000 children in the UK. The majority of the patients are younger than 6 years of age (80%) and there is a male predisposition. There is a clear geographical variety with children from Southeast Asia more affected [1]. The occurrence of PNS is correlated with T-cell immune disorders and abnormal glomerular podocyte proteins; however, the exact etiology and pathogenesis of PNS remain poorly understood.
Vitamin D has been shown to exert immunomodulatory effects [2-4]. The immune cell phenotype can be influenced by multiple natural and chemical compounds. One of these molecules is vitamin D3 and its active hormonal metabolite 1, 25-dihydroxyvitamin D3 (1, 25 (OH)2 D3) [5]. The multiple immunomodulatory and anti-inflammatory effects of vitamin D may have particular relevance in the Chronic Kidney Disease (CKD) population, given that the uremic state in humans results in a perturbed biochemical state characterized by inflammatory and oxidative stress as well as vitamin D deficiency [6]. In addition, Angiotensin converting enzyme inhibitor combined with vitamin D receptor activator lessens proteinuria, slows the process of glomerular sclerosis, and delays the progression of renal disease in uremic rats [7].
Nevertheless, it remains unclear whether vitamin D and its receptor are associated with the occurrence and outcome of nephrotic syndrome in children. The current study detected serum 25-hydroxyvitamin D3 (25 (OH) D3) levels and vitamin D receptor expression in the kidney of PNS children of different pathological types, and investigated the significance of vitamin D and its receptor in the occurrence and outcome of PNS.
Methods
Subjects for vitamin D level detection
We enrolled a total of 90 PNS children who were patients in the Department of Pediatrics, the Second Xiangya Hospital, Central South University, China, from July 2010 to February 2013. The study was approved by the Ethics Committee of the Second Xiangya Hospital and performed in accordance with the declaration of Helsinki. Informed consent was obtained from all participants included in the study. Participants were equally divided into an initial onset group, a remission group, and a non-remission group according to the disease course. Patients in the initial onset group experienced their first clinical episode with a mean duration of 14 d and received no treatment. The age in this group ranged from 0.75 to 13 y. Patients in the remission group received prednisone (2 mg/kg/d) for 4 w, with negative urine protein at the end of therapy, suggesting complete remission. Clinical episodes in this group lasted at least 30 d and the age ranged from 1.1 to 14 y. Patients in the non-remission group received prednisone (2 mg/kg/d) for 4 w, and urine protein was not negative at the end of therapy suggesting incomplete remission. The age range in this group was 2-14 y. Controls consisted of 90 healthy children, aged 1-12 y, who received health examination in the Child Health Clinic, the Second Xiangya Hospital, Central South University, China, from January to December 2012. This was a case-control study (Table 1).
| Group | Gender (male:female) | Age (y) | 25 (OH) D3 (nmol/l) |
|---|---|---|---|
| Control | 63:27 | 6.4 ± 2.5 | 70.2 (16.3) |
| Initial onset | 24:06 | 5.9 ± 3.4 | 26.8 (15.3)*† |
| Remission | 23:07 | 6.7 ±3.8 | 39.5 (19.2)* |
| Non-remission | 22:08 | 7.6 ± 3.4 | 23.5 (9.3)*‡ |
Table 1. Comparison of gender, age, and serum 25 (OH) D3 levels between the PNS groups and control group (mean ± s.d).
Subjects for vitamin D receptor expression detection
We enrolled 36 patients with PNS who underwent previous renal biopsy. The group included 28 males and 8 females, aged 1-16 y (mean, 7.57 y; standard deviation, 3.91 y). Indications for patients undergoing renal biopsy included little or no response to corticosteroid treatment and more than three relapses within 1 year. In accordance with the pathological type, these patients were equally assigned to a Focal Segmental Glomerulosclerosis (FSGS) group, Mesangial Proliferative Glomerulonephritis (MsPGN) group, and Minimal Change Disease (MCD) group. Three samples of kidney tissue served as controls and were obtained from patients whose kidneys had to be resected because of trauma, in the Department of Urinary Surgery, the Second Xiangya Hospital, Central South University, China. These kidney tissues showed no gross or microscopic pathological changes (Table 2).
| Item | FSGS group | MsPGN group | MCD group |
|---|---|---|---|
| Case number (n) | 12 | 12 | 12 |
| Age (y) | 7.2 (4.6) | 7.7 (3.0) | 7.6 (4.4) |
| Gender (male:female) | 10:02 | 08:04 | 10:02 |
| Blood urea nitrogen (mmol/l) | 3.9 (1.4) | 4.0 (1.4) | 4.1 (2.1) |
| Creatinine (µmol/l) | 30.3 (6.6) | 33.8 (13.8) | 34.6 (10.8) |
Table 2. Clinical data of the PNS patients undergoing renal biopsy (mean (s.d)).
Exclusion criteria
Exclusion criteria included: (1) Previous history of antiepileptic drug administration or the use of vitamin D preparations in the children during therapy; and (2) liver and kidney dysfunction; endocrine disease; calcium or phosphorus metabolism disorders.
Determination of serum 25 (OH) D3 levels and urine protein/urine creatinine ratio
Enzyme-linked immunosorbent assay was used to measure serum 25 (OH) D3 levels with using ELISA kits EuroImmun (cat. No. EQ 6411-9601) [8]. A mid-stream urine sample was collected in the morning for the detection of urine protein and urine creatinine. Urinary total protein (benzethonium chloride turbidimetric method) and urine creatinine (Jaffe colorimetric method) on Roche cobas c701 (Roche Diagnostics, Indianapolis, IN, USA) [9].
Detection of vitamin D receptor expression in kidney tissue
Briefly, kidney tissue embedded in wax was sliced into 4 μmthick paraffin sections. The sections were dried in an oven at 60°C for 4 h to make slices closely adherent. The sections were heated at 60°C for 1 h, dewaxed twice in xylene for 5 min each time, hydrated, then followed by antigen retrieval. Sections were then incubated with an appropriate amount of endogenous peroxidase (approximately three drops) at room temperature for 10 min, washed with phosphate-buffered saline, blocked with normal goat serum at room temperature for 10 min following air-dried. Sections were then treated with primary antibody working solution (vitamin D receptor antibody 1:100, ab8756, Abcam) at room temperature for 90 min, washed with phosphate-buffered saline, and incubated with biotinylated secondary antibody (1:800, ab175714, Abcam) working solution at room temperature for 10 min, then washed with phosphate-buffered saline. The sections were then treated with horseradish peroxidase-labeled streptavidin-biotin at room temperature for 10 min, washed with phosphate-buffered saline, visualized with 3, 3'-diaminobenzidine, and then mounted.
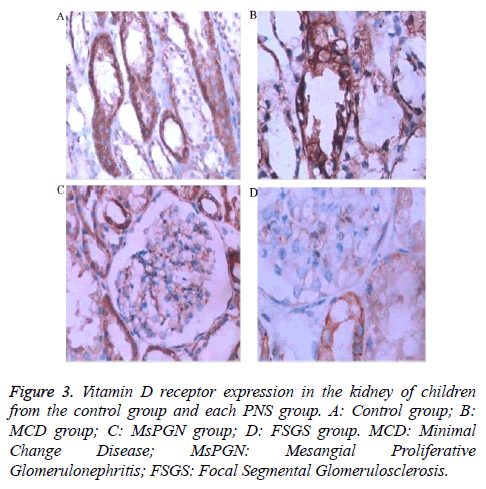
Analysis of immunohistochemical images
The staining intensity of positive cells was observed under light microscopy (X400) with vitamin D receptor expression appearing as brown particles in positive cells. Images were analysed using Image Pro Plus 6.0 software (Media Cybernetics, Atlanta, GA, USA). Integrated optical density represents the strength of vitamin D receptor expression and it is directly proportional to the positive rate of vitamin D receptor expression. Optical density values were calculated in three fields in each section under light microscopy at X400 magnification. In each field, approximately 80% of the cells were arranged in roughly equal density. The mean value refers to the strength of vitamin D receptor expression in the kidney tissue for each case [10].
Statistical analysis
The data were analysed using SPSS 17.0 software (SPSS Inc., Chicago, IL, USA). Measurement data that obeyed normal distribution were expressed as means (sd). Two samples using a group design were compared by t-test and multiple sample mean using a group design was compared by analysis of variance. Paired comparisons among multiple sample means were done using the Newman-Keuls method. Numeration data were compared using the line × list chi-square test and correlation analysis was done using Pearson’s linear correlation analysis. A P-value less than 0.05 was considered statistically significant.
Results
Serum 25 (OH) D3 levels in PNS children
Serum 25 (OH) D3 levels were significantly lower in the 90 PNS patients (4.05-90.20 nmol/l, mean 29.21 nmol/l) than levels in the control group (P<0.05). Significant differences in serum 25 (OH) D3 levels were detected between the PNS groups and the control group (P<0.01). Serum 25 (OH) D3 levels were lower in the initial onset group and non-remission group than that in the remission group (P<0.05, and P<0.01, respectively). No significant differences in serum 25 (OH) D3 levels were detectable between the initial onset group and the non-remission group (P>0.05, Table 1).
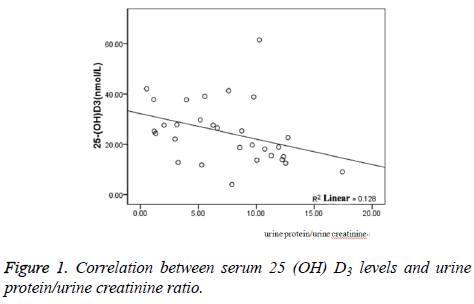
Correlation of serum 25 (OH) D3 levels and urine protein/urine creatinine ratio
Univariate correlation analysis demonstrated that serum 25 (OH) D3 levels were negatively correlated with urine protein/ urine creatinine ratios in the exacerbation and non-remission stages in PNS children (r=-0.331, P=0.01, Figure 1).
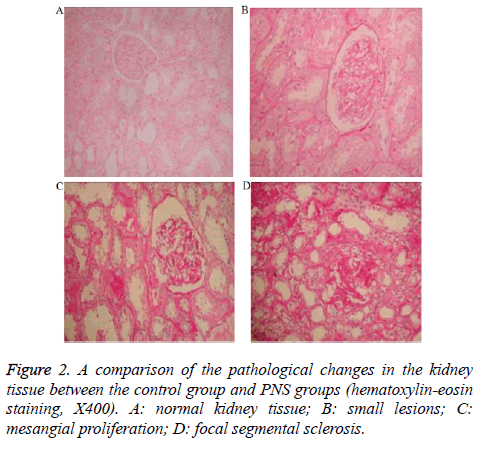
Vitamin D receptor expression in kidney tissue
Pathological changes in the kidney tissue in the control group and each PNS group are shown in Figure 2. Vitamin D receptor expression in the kidney tissue in the control group and PNS groups is shown in Figure 3. Vitamin D receptor expression (integrated optical density) was significantly lower in each PNS group than that in the normal kidney tissue (P<0.05). Significant differences in vitamin D receptor expression were observed between the FSGS, MsPGN and MCD groups using paired comparison (P<0.05). Vitamin D receptor expression in the kidney tissue was significantly lower in the FSGS group than that in the MCD and MsPGN groups (P<0.05) and also lower in the MsPGN group than that in the MCD group (P<0.05). With worsening severity of kidney tissue lesions, vitamin D receptor expression gradually declined. Also, vitamin D receptor expression was weakest in the kidneys affected by glomerular sclerosis (Table 3).
| Group | Case number (n) | Integrated optical density |
|---|---|---|
| Control | 12 | 18294.2 (2471.6) |
| MCD | 12 | 15888.7 (3484.0)* |
| MsPGN | 12 | 10948.1 (1936.0)*† |
| FSGS | 12 | 6674.8 (2059.3)*†‡ |
Table 3. Vitamin D receptor expression in the kidney in each group (mean (s.d)).
Discussion
During PNS attacks, a large amount of middle-molecule proteinuria can be eliminated because of changes in glomerular filtration membrane permeability. Therefore, 25 (OH) D3 can easily be lost in the urine, resulting in a decrease in serum 25 (OH) D3 levels. Mittal et al. [8] verified that 25 (OH) D3 levels were reduced in nephrotic syndrome children, and that 25 (OH) D3 levels were negatively correlated with proteinuria. Previous studies have shown that vitamin D levels were inversely proportional to the degree of proteinuria [11,12]. Our results also confirmed that serum 25 (OH) D3 levels were negatively associated with urine protein/urine creatinine in PNS children, indicating that the decrease in serum 25 (OH) D3 levels was possibly correlated with urinary protein excretion or the increase in urinary protein excretion was associated with the decrease in serum 25 (OH) D3 levels. Wozniak et al. [13] demonstrated that 25 (OH) D3 levels diminished in PNS children during the remission stage. Zhang et al. [14] showed that 25 (OH) D3 levels in PNS children after more than 3 months of remission were similar to those in the normal control group, and 25 (OH) D3 levels were lowest within 3 months of recurrence. In this study, serum 25 (OH) D3 levels were significantly lower in the PNS children than for normal controls. 25 (OH) D3 levels were higher in the remission group than in the initial onset group and non-remission group, but still lower than in the control group, suggesting that serum 25 (OH) D3 levels were correlated with changes in the disease stage.
Chronic use of glucocorticoids impacts calcium and phosphorus metabolism, and negatively adjusts vitamin D metabolism. In the present study, serum 25 (OH) D3 levels were slightly higher in the PNS children in the initial onset group (without any prior treatment) than in children from the non-remission group (treatment with glucocorticoids 2 mg/kg/d for 4 w), but no significant difference was detected between the two groups. These findings indicated that short-term treatment with glucocorticoids was not the reason for decreased serum 25 (OH) D3 levels in PNS children.
Vitamin D plays a biological role by binding to vitamin D receptor on target cells in the body. Vitamin D receptor expression was selectively found in the renal proximal convoluted tubule, distal convoluted tubule, medullary collecting duct, and the ascending branch [15]. Vitamin D receptor expression was also detectable in mesangial cells and podocytes. Vitamin D receptor in the kidney regulates the renal proximal tubule absorption of calcium and phosphorus by binding to 1, 25 (OH)2 D3, promoting bone formation and mineralization, suppressing the proliferation of monocytes and macrophages by promoting their differentiation, adjusting the secretion of active T-lymphocytes into various cytokines, and exerting various immunomodulatory effects. A previous study confirmed that vitamin D receptors reduced proteinuria, lessened the degree of glomerular sclerosis, and exerted protective effects against kidney diseases by inhibiting the renin angiotensin system, and having an anti-inflammatory and anti-fibrotic effect [16]. Banerjee et al. verified that the activation of calcitriol receptors decreased the degree of fibrosis in the kidney by suppressing type I collagen, type III collagen, tumor growth factor-β1, and fibronectin mRNA expression in a rat model of unilateral ureteral obstruction [17]. These results suggest that vitamin D receptors have protective effects on the kidney in a rat model of kidney disease. Results from our study demonstrated that vitamin D receptor expression was detected mainly in the cytoplasm of renal tubular epithelial cells, and partially in the tubular epithelial cell membrane in each PNS group. Vitamin D receptor expression was also weakly observed in the mesangial cells and podocytes. Our results also showed that vitamin D receptor expression in the kidney was associated with the severity of renal pathological changes. Vitamin D receptor expression in the normal kidney was obviously higher than that in the kidney with PNS. Vitamin D receptor expression was higher in children with MCD and MsPGN than in those with FSGS, and higher in MCD children than in MsPGN children, and lowest in FSGS children. Therefore, vitamin D receptor expression could potentially be used to assess the degree of renal pathological changes. Decreased vitamin D receptor expression reduces its immunomodulatory effects (differentiation promotion, proliferation suppression) on intrinsic renal cells, and induces abnormal proliferation of mesangial cells and glomerular sclerosis.
The main limitation of our study is the small sample size and further investigation with a large sample size is needed.
In summary, serum 25 (OH) D3 levels were reduced in the exacerbation and remission stages in PNS children and this reduction was correlated with urinary protein excretion. Changes in vitamin D receptor expression in the PNS kidney are likely associated with glomerular sclerosis. Therefore, decreased 25 (OH) D3 levels and altered vitamin D receptor expression in PNS children may be associated with the occurrence and outcome of PNS; therefore, serum 25 (OH) D3 levels should be measured regularly in PNS patients. Timely replenishment of vitamin D may effectively prevent the progression of PNS and reduce the occurrence of glomerular sclerosis.
References
- Zolotas E, Krishnan RG. Nephrotic syndrome. Paediatr Child Health 2016; 26: 349-352.
- Mazzaferro S, Goldsmith D, Larsson TE. Vitamin D metabolites and/or analogs: which D for which patient? Curr Vasc Pharmacol 2014; 12: 339-349.
- Hossein-nezhad A, Holick MF. Vitamin D for health: a global perspective. Mayo Clin Proc 2013; 88: 720-755.
- Lang CL, Wang MH, Chiang CK. Vitamin D and immune system from the nephrologists viewpoint. ISRN Endocrinol 2014; 2014: 105456.
- Vanherwegen AS, Gysemans C, Mathieu C. Vitamin D endocrinology on the cross-road between immunity and metabolism. Mol Cell Endocrinol 2017; 453: 52-67.
- Bucharles S, Barberato SH, Stinghen AE, Gruber B, Piekala L, Dambiski AC. Impact of cholecalciferol treatment on biomarkers of inflammation and myocardial structure in hemodialysis patients without hyperparathyroidism. J Ren Nutr 2012; 22: 284-291.
- Battault S, Whiting SJ, Peltier SL. Vitamin D metabolism, functions and needs: from science to health claims. Eur J Nutr 2013; 52: 429-441.
- Granlund L, Ramnemark A, Andersson C. Prevalence of vitamin D deficiency and its association with nutrition, travelling and clothing habits in an immigrant population in Northern Sweden. Eur J Clin Nutr 2016; 70: 373-379.
- Katayev A, Zebelman AM, Sharp TM, Flynn S, Bernstein RK. Prevalence of isolated non-albumin proteinuria in the US population tested for both, urine total protein and urine albumin: An unexpected discovery. Clin Biochem 2017; 50: 262-269.
- Eyles DW, Liu PY, Josh P. Intracellular distribution of the vitamin D receptor in the brain: Comparison with classic target tissues and redistribution with development. Neuroscience 2014; 268: 1-9.
- Prietl B, Treiber G, Pieber TR. Vitamin D and immune function. Nutrients 2013; 5: 2502-2521.
- Kunisawa J, Sugiura Y, Wake T. Mode of bioenergetics metabolism during B cell differentiation in the intestine determines and distinct requirement for vitamin B1. Cell Rep 2015; 13: 122-131.
- Wozniak LJ, Bechtold HM, Reyen LE. Vitamin D deficiency in children with intestinal failure receiving home parenteral nutrition. J Parent Enter Nutr 2015; 39: 471-475.
- Xingxing Z, Xiaochuan W, Lan X, Zhuwen Y, Qingnan H, Xiaojie H. Role of vitamin d3 in regulation of t helper cell 17 and regulatory t-cell balance in rats with immunoglobulin A nephropathy. Iran J Kidney Dis 2014; 8: 363-370.
- Finch JL, Suarez EB, Husain K, Ferder L, Cardema MC, Glenn DJ. Effect of combining an ACE inhibitor and a VDR activator on glomerulosclerosis, proteinuria, and renal oxidative stress in uremic rats. Am J Physiol Renal Physiol 2012; 302: 141-149.
- Al-Eisa AA, Haider MZ. Vitamin D receptor gene TaqI and Apal polymorphisms and steroid responsiveness in children idiopathic nephrotic syndrome. Int J Nephrol Renovasc Dis 2016; 2016: 187-192.
- Banerjee S, Basu S, Sengupta J. Vitamin D in nephrotic syndrome remission: a case-control study. Pediatr Nephrol 2013; 28: 1983-1989.