- Biomedical Research (2012) Volume 23, Issue 4
Vascular Thoracic Outlet Syndrome
Mohammed Al-Omran*The Peripheral Vascular Disease Research Chair and Division of Vascular Surgery, Department of Surgery, College of Medicine, King Saud University, Riyadh, Saudi Arabia
- *Corresponding Author:
- Mohammed Al-Omran
King Khalid University Hospital
Department of Surgery
P.O. Box 7805(37)
Riyadh 11472, Saudi Arabia
Accepted date: June 09 2012
Abstract
Thoracic outlet syndrome (TOS) is a collection of upper extremity symptoms that result from compression of the neurovascular bundle by various structures in the area just above the first rib and behind the clavicle. Although vascular TOS (venous and arterial) account for only 5% of all TOS cases, leaving the majority for neurogenic cases, it is associated with the most serious complications, including limb ischemia. The main pathophysiology is based on a mechanism of chronic compression over the subclavian artery or vein and then stenosis, which results in further intimal injury with fibrosis, thickening, and arterial luminal narrowing or complete or partial venous occlusion and thrombosis. Arm swelling, cyanosis, and other symptoms of primary venous thromboses represent the clinical picture of venous TOS. With arterial TOS, an ischemic hand in various pictures represents an advance stage, whereas asymptomatic cases are the majority. Various invasive and non-invasive examination tests can help in diagnosing and distinguishing among the etiologies of TOS; however, conventional arteriography and venography remains the gold standard for vascular investigation testing. Of note, this method has gradually been replaced by advanced CT angiography/venography. In terms of vascular TOS treatment, the role of conservative management is limited and the main target of treatment, which includes relieving the compression over the neurovascular structures, is mainly achieved by surgical option with superior results with early intervention.
Keywords
Thoracic outlet syndrome, subclavian artery, subclavian vein
Introduction
Thoracic outlet syndrome (TOS) involves compression resulting in injury or irritation of neurovascular structures as they course through the narrow passageway from the base of the neck into the arm via the axilla, or in a broader definition, is upper extremity symptoms due to compression of the neurovascular bundle by various structures in the area just above the first rib and behind the clavicle. This region is constrained by the anterior middle scalene muscles, clavicle, and first and second ribs. Within this area, the brachial plexus exits the cervical spine and passes between the anterior and middle scalene musculature, and under the clavicle and pectoralis minor muscle, along with the main upper limp vasculature, subclavian artery and vein. The most important narrow passageway in this area anatomically is the scalene triangle, which bounded by the anterior and middle scalene muscles with the 1st rib forming the base. These muscles can be further hypertrophied after repetitive motion and create more compression. Although the narrowing of this area can be further constricted by other structures such as congenital cervical ribs, which have an incidence rate of 1% [1], fibrous bands and anomalous muscles may be a more common cause of narrowing.
Historically, Galen was the first one who described the cervical rib in human dissections around 150 AD [2] and until 1927 the cervical rib was commonly thought to be the cause of symptoms of TOS [3] while thoracic outlet syndrome, as a medical term, was first introduced in 1956 by Peet et al [4]. TOS is classified into three distinct subtypes based on the involved structure: neurogenic, venous, and arterial; symptoms of each subtype are produced relative to which of the neurovascular structures is compressed in the thoracic outlet.
Epidemiology
With lack of confirmatory testing for TOS, the true incidence is not known, but the reported incidences range from 3 to 80 cases per 1000. It is more commonly observed in women with a peak of onset in the 4th decade of life [5,6]. Vascular TOS, which has given more interest in this review, account for only 5% of all TOS cases [1].The venous type is the more common of the two vascular TOS, and is seen in approximately 3-4% of cases, whereas arterial TOS is seen in only 1% of cases but associated with the most serious complications, including limb ischemia [3,7,8].
Pathophysiology
For arterial TOS, the essential mechanism is chronic compression over the subclavian artery, and then stenosis. Furthermore, this chronic compression can result in intimal injury with fibrosis, thickening of the wall, and, eventually, luminal narrowing. Poststenotic dilation may also develop distal to the site of narrowing secondary to compression over the subclavian artery and it might progress to aneurismal changes with time. Basically, compression over the subclavian artery and stretching of the arterial wall (poststenotic), resulting in disruption of the natural integrity of the intima. This disruption precipitates platelet deposition and initiates formation of a thrombus after activation of collagen and tissue factor that play an important role in thrombus formation by activation and accumulation of platelets and generation of thrombin [9]. Distal thromboembolism is one of the complications that may result either due to mural thrombus originating from within the area of poststenotic dilation, or from an intimal lesion at the site of compression with resultant formation of platelet aggregates.
These platelet aggregates may microembolize distal to the small vessels of the hands and fingers, resulting in ischemia with eventual tissue necrosis. Mural thrombi typically result in the occlusion of more proximal arteries with larger collateral supplies; therefore, mural thrombi are less likely to produce severe ischemic changes than other types. Rarely, complete occlusion of the subclavian artery may occur. Bony abnormality represents the most frequent cause of arterial compression in the thoracic outlet. Among arterial TOS patients, 88% presented an osseous abnormality [10], most of which were cervical ribs, up to 63% in some of the large series[10-12]. Upper extremities overuse is considered a significant but not essential cause of arterial TOS[12-14]. The result is soft tissue hypertrophy and cramping in the space of the bony outlet, or can lead to direct arterial injury through repetitive motion.
On the other hand, occlusion of the subclavian vein, completely or partially, is the primary mechanism of venous TOS. This venous occlusion, also known as Paget- Schroetter syndrome, primary subclavian vein thrombosis or effort thrombosis, accounts for approximately 2% to 4% of all DVT cases [15]. Venous TOS occurs in related to multifactorial etiology including extrinsic compression at the costoclavicular space, or trauma with a congenitally narrow thoracic inlet. As in arterial TOS, chronic extrinsic compression may be caused by one of the anatomical structures mentioned earlier, and this compression can be exaggerated with certain positions or activity of upper extremity like swimming, weight lifting, throwing a baseball (athletes) or working with elevated arms [16,17]. Chronic compression and irritation of the vessel walls can predispose or cause stasis, mainly by impairing the clearance of activated coagulation factors; intimal damage, through exposure of tissue factor to the blood coagulation system; and/or hypercoagulability (Virchow triad), resulting in formation of an intraluminal thrombus, which causes the lumen to become narrowed or entirely occluded, and end with primary venous thrombosis[18]. Chronic compression and trauma eventually produce external inflammation as well, which leads to fibrosis, relative fixation to the surrounding anatomic structures beside the intimal hypertrophy. This chronic inflammation can be explained by the replacement of loose connective tissue that normally surrounds the vein by dense collagen scarring, which further reduces the vein mobility and poses increased risk for further injury.
Clinical presentation
At the early stages of arterial cases, most of patients are asymptomatic due to lacking of atherosclerotic occlusive disease clinical markers. Then, patients present with varying degrees of ischemia in the affected arm or hand, range between chronic ischemia at the beginning with signs and symptoms including weakness, paresthesias, claudication, pallor, and diminished pulses distally, especially with activity or positional changes, acute ischemia with sudden onset of severe hand pain mainly secondary to distal embolization and gradual critical ischemia in the form of pain of the hand at rest (rest pain) and digital gangrene or ulceration after microembolization of small arteries [5,19].
Arm swelling, cyanosis and moderate pain are the main clinical presentations of venous TOS or primary venous thrombosis that commonly occurs suddenly and begins within the first 24 hours. All of these signs and symptoms result from venous hypertension and may improve gradually secondary to collateral formation and recanalization of the vein in many patients [20].
Diagnosis
Various examination maneuvers can help in the diagnosis and distinguishing among the etiologies of TOS, but positive results of these tests can occur under normal conditions in some cases, hence they are not sufficient for diagnosis. The Adson test, abolition or reduction of patient’s radial pulse with externally rotated, extended and slightly abducted arm and while patient is looking towards the side being examined and taking in a deep breath; and the Roos test, developing of hand paresthesias or pain after external rotation and abduction of the arm more than 90 degrees, are examples of these compression maneuvers, but none of them is pathognomonic [21,22].
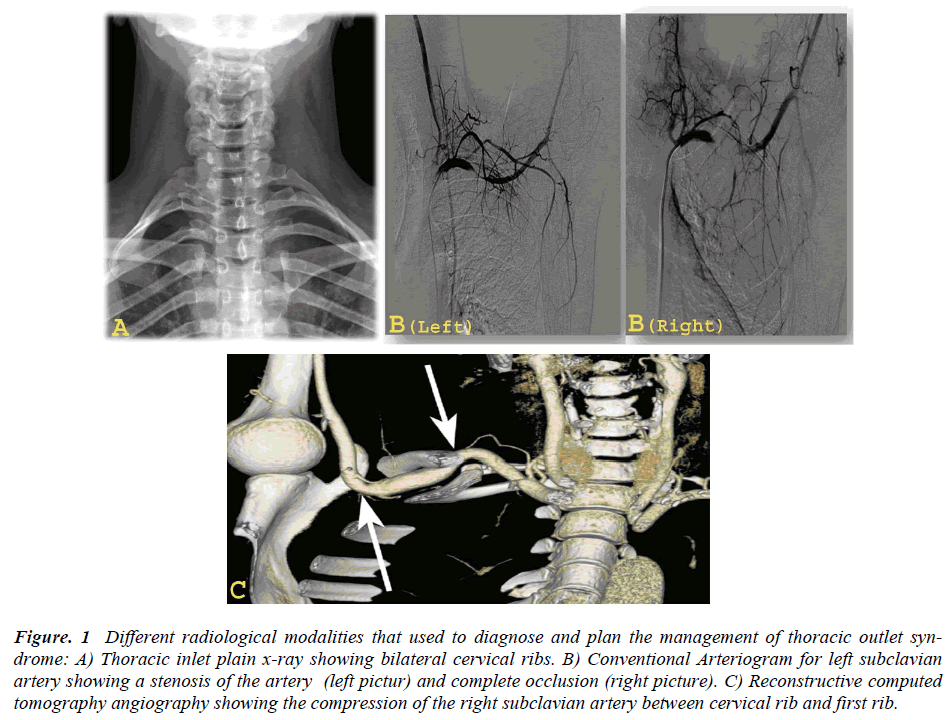
A plain radiograph of the neck and chest with cervical spine view or thoracic inlet view is one of the initial noninvasive and simple procedures that can assist in the diagnosis of vascular TOS[23](Figure.1A). Although this kind of imaging is not essential in the diagnosis, it is helpful and important to demonstrate the presence of any osseous abnormality including cervical ribs, prominent or elongated C7 transverse processes, abnormal or elevated 1st rib caused by tight anterior or middle scalene muscles, large clavicle fractures, callus, or any other bony pathology.
Figure. 1 Different radiological modalities that used to diagnose and plan the management of thoracic outlet syndrome: A) Thoracic inlet plain x-ray showing bilateral cervical ribs. B) Conventional Arteriogram for left subclavian artery showing a stenosis of the artery (left pictur) and complete occlusion (right picture). C) Reconstructive computed tomography angiography showing the compression of the right subclavian artery between cervical rib and first rib.
Doppler ultrasound or duplex is very useful and helpful in the diagnosis for both types of vascular TOS. A near cutoff of flow during the stress (hyperabduction) maneuver with reproduction of symptoms is the most suggestive in this non-invasive test. Duplex also can detect poststenotic subclavian artery aneurysms as well as the thrombosis of axillary and other distal arteries. Moreover, this test is non-invasive, simple, and easily performed bilaterally in one sitting, making it an effective method and first step in confirming a suspicious clinical diagnosis of vascular TOS when compared to other conventional methods [24,25].
Upper extremity conventional or catheter-based arteriography and venography is an effective vascular investigation test, but is a highly invasive procedure. It can confirm vascular compression with exact localization and highlight subclavian stenoses, aneurysms, mural thrombus or occlusion of the digital arteries as well as subclavian and axillary vein thrombosis (Figure. 1B) . In addition, arteriography permits dynamic views of the subclavian and axillary arteries with the arms in abduction and adduction and provides evaluation of the distal circulation. This procedure remains a helpful tool and the gold standard for assessment of vascular TOS and for pre-operative planning, but its role has become limited, gradually replaced by advanced CT angiography/venography.
Computed tomographic (CT) angiography/venography with positioning arm maneuvers is very useful in providing accurate information on the location and mechanism of vascular compression. Details of the relationship of bony deformity or any abnormal fibrous bands with arterial or venous compression as well as identifying all of the structures in the thoracic outlet can be easily demonstrated by CT angiography/ venography, especially threedimensional CT imaging, with the avoidance of invasive conventional arteriography/ venography complications [26,27]. The CT angiogram is an important test in the assessment of TOS, and for pre-operative planning, and even in asymptomatic or questionable TOS cases; it can improve surgical success and help for selection of operative candidates [28] (Figure. 1C).
Magnetic resonance angiography and venography (MRA/MRV) is another choice of imaging modality that can be used for diagnosis and evaluation of vascular TOS. Although an MRI scan is a promising noninvasive technique for the diagnosis of vascular causes of TOS, the required cost and time are considerable, and the specificity and sensitivity for diagnosing arterial or venous TOS seems to be low. Indeed, an MRI scan is more useful for identification and visualization of soft tissue abnormalities; or fibromuscular changes that might cause the narrowing at the thoracic inlet area rather than establishing the diagnosis of vascular TOS, and it is still the imaging method of choice for evaluating the anatomy and pathology of the brachial plexus in neurogenic TOS[29-31].
Management
Treatment of TOS in general can be either conservative or surgical. The goal of the surgical option is to relieve the compression over the neurovascular structures as well as reconstruct any involved vessel and restoration of perfusion to the distal extremity (e.g., with thromboembolectomy) in vascular cases.
Although conservative management is still recommended for neurogenic cases including modification of behaviors by avoiding provocative activities, and using physical therapy, analgesics and muscle relaxants, its role with vascular TOS is very narrow or even nonexistent, as in symptomatic arterial TOS cases [1,32]. Surgical intervention represents the core of most treatment options, and provides good and fast results in vascular TOS, and the majority of patients appear to benefit from surgery, principally arterial TOS patients.
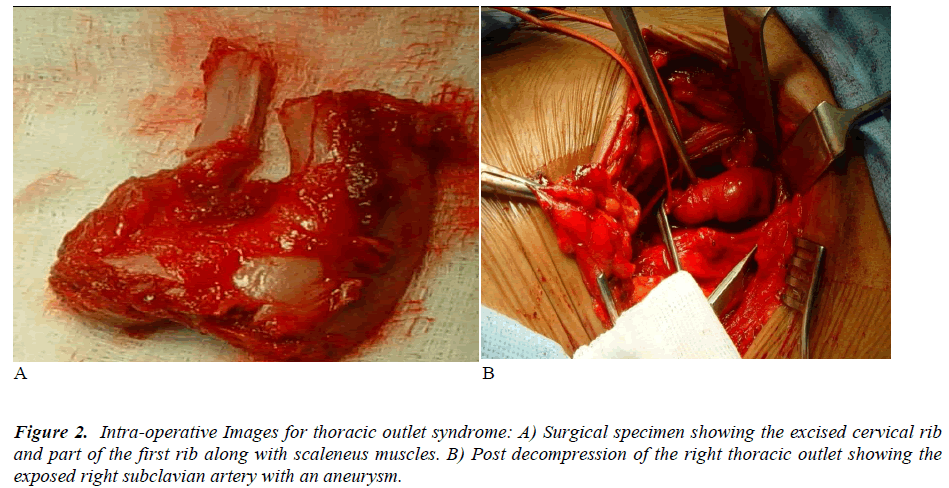
In arterial TOS, surgical decompression is recommended for most cases. Decompression of the thoracic outlet area includes resection of cervical rib or 1st rib, scalenectomy, and/or fibrous bands removal (Figure. 2A). All of these can be provided surgically through many approaches, mainly supraclavicular and transaxillary. Each procedure has some advantages but the same objectives. For example, supraclavicular scalenectomy with excision of the cervical rib and/or 1st rib resection provides good visualization of the thoracic outlet area, and excellent exposure for arterial reconstruction if needed, with excellent results in many cases[33,34]. Arterial reconstruction procedures include resection of the aneurysm of the subclavian artery with a replacement using either a vein or synthetic (e.g., Gortex) interposition graft(s), as well as distal thrombectomy through these kind of approaches (Figure. 2B). The successes of surgical decompression of the thoracic outlet area in arterial cases that have been reported in the literature are impressive, and improvement in the symptoms is quick, especially with acute and critical cases [11,12]. Percutaneous transluminal angioplasty and thrombolysis are a potential treatment option for arterial TOS that can be used in some selected cases such as those that are poor surgical candidates. However, their results are not as favorable as the gold standard, surgical decompression [35].
The principle of management for venous TOS is the same as arterial, whereas the role of non-surgical treatment is respectable. All venous TOS patients should be anticoagulated for 3 to 6 months, and followed clinically by ultrasound scans [36]. Wire passage with thrombolysis plays an important role in venous cases treatment. However, timing of thrombolysis represents the key of success for this kind of treatment, as early thrombus is soft and easily treated, whereas chronic ones become organized, adherent, and fibrotic[37,38]. Nevertheless, surgical decompression of the thoracic outlet remains the ideal option, even among venous cases, especially those patients with persistent stenosis or signs of extrinsic compression on venography after thrombolytic therapy, and most studies suggest performing decompression as early as possible after thrombolysis, in order to decrease the risk of reocclusion [39,40].
Conclusion
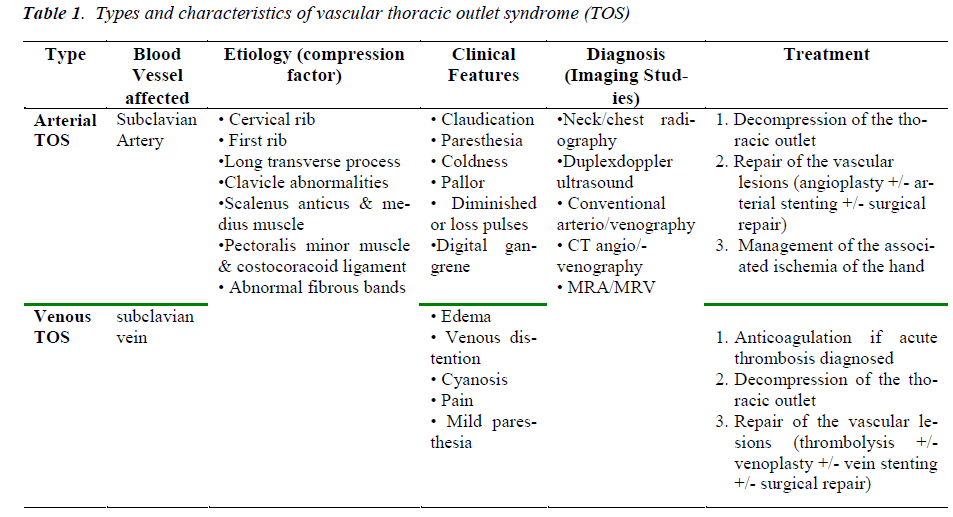
Perhaps vascular TOS represents a low percentage of thoracic outlet syndrome cases generally and is considered a rare disease, it is a serious disorder if not discovered promptly, and treated professionally. Subclavian artery intimal injury, poststenotic aneurysm, mural thrombus formation and embolization could result in significant complications; acute and critical upper extremity ischemia, and less commonly pulmonary embolism secondary to venous cases. Thoracic outlet-related vascular complications may remain underestimated with delay of obvious findings and may cause acute arterial complications. Effective treatment of vascular thoracic outlet syndrome requires early recognition of the disease by providing accurate clinical assessment together with selection of the proper type of investigative imaging. Careful surgical planning for vascular TOS patients can yield satisfactory outcomes. Table 1 summarizes the types, etiology, features, diagnosis, and management of vascular thoracic syndrome.
References
- Fugate MW, Rotellini-Coltvet L, Freischlag JA. Current management of thoracic outlet syndrome. Curr Treat Options Cardiovasc Med 2009; 11(2): 176-183.
- Atasoy E. History of thoracic outlet syndrome. Hand Clin 2004; 20(1): 15-16.
- Urschel HC, Kourlis H. Thoracic outlet syndrome: a 50- year experience at Baylor University Medical Center. Proc (Bayl Univ Med Cent) 2007; 20(2): 125-135.
- PEET RM, HENRIKSEN JD, ANDERSON TP, MARTIN GM. Thoracic-outlet syndrome: evaluation of a therapeutic exercise program. Proc Staff Meet Mayo Clin 1956; 31(9): 281-287.
- Huang JH, Zager EL. Thoracic outlet syndrome. Neurosurgery 2004; 55(4): 897-902.
- Podlaha J. Thoracic outlet syndrome--24 years of experience. Bratisl Lek Listy 2007; 108(10-11): 429-432.
- Sanders RJ, Hammond SL, Rao NM. Diagnosis of thoracic outlet syndrome. J Vasc Surg 2007; 46(3): 601- 604.
- Makhoul RG, Machleder HI. Developmental anomalies at the thoracic outlet: an analysis of 200 consecutive cases. J Vasc Surg 1992; 16(4): 534-542.
- Furie B, Furie BC. Mechanisms of thrombus formation. N Engl J Med 2008; 359(9): 938-949.
- Sanders RJ, Haug C. Review of arterial thoracic outlet syndrome with a report of five new instances. Surg Gynecol Obstet 1991; 173(5): 415-425.
- Cormier JM, Amrane M, Ward A, Laurian C, Gigou F. Arterial complications of the thoracic outlet syndrome: fifty-five operative cases. J Vasc Surg 1989; 9(6): 778- 787.
- Durham JR, Yao JS, Pearce WH, Nuber GM, McCarthy WJ, III. Arterial injuries in the thoracic outlet syndrome. J Vasc Surg 1995; 21(1): 57-69.
- Short DW. The subclavian artery in 16 patients with complete cervical ribs. J Cardiovasc Surg (Torino) 1975; 16(2): 135-141.
- Pairolero PC, Walls JT, Payne WS, Hollier LH, Fairbairn JF. Subclavian-axillary artery aneurysms. Surgery 1981; 90(4): 757-763.
- Malhotra S, Punia VP. Upper extremity deep vein thrombosis. J Assoc Physicians India 2004; 52: 237- 241.
- Kommareddy A, Zaroukian MH, Hassouna HI. Upper extremity deep venous thrombosis. Semin Thromb Hemost 2002; 28(1): 89-99.
- Adelman MA, Stone DH, Riles TS, Lamparello PJ, Giangola G, Rosen RJ. A multidisciplinary approach to the treatment of Paget-Schroetter syndrome. Ann Vasc Surg 1997; 11(2): 149-154.
- Bagot CN, Arya R. Virchow and his triad: a question of attribution. Br J Haematol 2008; 143(2): 180-190.
- Sanders RJ, Hammond SL, Rao NM. Thoracic outlet syndrome: a review. Neurologist 2008; 14(6): 365-373.
- Illig KA, Doyle AJ. A comprehensive review of Paget- Schroetter syndrome. J Vasc Surg 2010; 51(6): 1538- 1547.
- ADSON AW. Surgical treatment for symptoms produced by cervical ribs and the scalenus anticus muscle. Surg Gynecol Obstet 1947; 85(6): 687-700.
- Roos DB, Owens JC. Thoracic outlet syndrome. Arch Surg 1966; 93(1): 71-74.
- Demondion X, Herbinet P, Van Sint JS, Boutry N, Chantelot C, Cotten A. Imaging assessment of thoracic outlet syndrome. Radiographics 2006; 26(6): 1735- 1750.
- Wadhwani R, Chaubal N, Sukthankar R, Shroff M, Agarwala S. Color Doppler and duplex sonography in 5 patients with thoracic outlet syndrome. J Ultrasound Med 2001; 20(7): 795-801.
- Hachulla E, Camilleri G, Fournier C, Vinckier L. [Clinical, flowmetric and radiologic study of the thoracic outlet in 95 healthy subjects: physiologic limitations and practical impact]. Rev Med Interne 1990; 11(1): 19-24.
- Remy-Jardin M, Remy J, Masson P, Bonnel F, Debatselier P, Vinckier L et al. Helical CT angiography of thoracic outlet syndrome: functional anatomy. AJR Am J Roentgenol 2000; 174(6): 1667-1674.
- Jeung MY, Gangi A, Gasser B, Vasilescu C, Massard G, Wihlm JM et al. Imaging of chest wall disorders. Radiographics 1999; 19(3): 617-637.
- Hasanadka R, Towne JB, Seabrook GR, Brown KR, Lewis BD, Foley WD. Computed tomography angiography to evaluate thoracic outlet neurovascular compression. Vasc Endovascular Surg 2007; 41(4): 316-321.
- Charon JP, Milne W, Sheppard DG, Houston JG. Evaluation of MR angiographic technique in the assessment of thoracic outlet syndrome. Clin Radiol 2004; 59(7): 588-595.
- Demondion X, Bacqueville E, Paul C, Duquesnoy B, Hachulla E, Cotten A. Thoracic outlet: assessment with MR imaging in asymptomatic and symptomatic populations. Radiology 2003; 227(2): 461-468.
- Hagspiel KD, Spinosa DJ, Angle JF, Matsumoto AH. Diagnosis of vascular compression at the thoracic outlet using gadolinium-enhanced high-resolution ultrafast MR angiography in abduction and adduction. Cardiovasc Intervent Radiol 2000; 23(2): 152-154.
- Reeser JC. Diagnosis and management of vascular injuries in the shoulder girdle of the overhead athlete. Curr Sports Med Rep 2007; 6(5): 322-327.
- Sanders RJ, Pearce WH. The treatment of thoracic outlet syndrome: a comparison of different operations. J Vasc Surg 1989; 10(6): 626-634.
- Thompson RW, Petrinec D. Surgical treatment of thoracic outlet compression syndromes: diagnostic considerations and transaxillary first rib resection. Ann Vasc Surg 1997; 11(3): 315-323.
- Farina C, Mingoli A, Schultz RD, Castrucci M, Feldhaus RJ, Rossi P et al. Percutaneous transluminal angioplasty versus surgery for subclavian artery occlusive disease. Am J Surg 1989; 158(6): 511-514.
- Illig KA, Doyle AJ. A comprehensive review of Paget- Schroetter syndrome. J Vasc Surg 2010; 51(6): 1538- 1547.
- Doyle A, Wolford HY, Davies MG, Adams JT, Singh MJ, Saad WE et al. Management of effort thrombosis of the subclavian vein: today's treatment. Ann Vasc Surg 2007; 21(6): 723-729.
- Urschel HC, Jr., Razzuk MA. Paget-Schroetter syndrome: what is the best management? Ann Thorac Surg 2000; 69(6): 1663-1668.
- Angle N, Gelabert HA, Farooq MM, Ahn SS, Caswell DR, Freischlag JA et al. Safety and efficacy of early surgical decompression of the thoracic outlet for Paget- Schroetter syndrome. Ann Vasc Surg 2001; 15(1): 37- 42.
- Melby SJ, Vedantham S, Narra VR, Paletta GA Jr, Khoo-Summers L, Driskill M et al. Comprehensive surgical management of the competitive athlete with effort thrombosis of the subclavian vein (Paget- Schroetter syndrome). J Vasc Surg 2008; 47(4): 809- 820.