Research Article - Biomedical Research (2017) Volume 28, Issue 16
Value of multi-slice spiral CT and magnetic resonance imaging in diagnosis of hepatic veno-occlusive disease (HVOD)
Zhitao Shi#, Yuhong Wang#, Yanhui Wang and Yueqin Chen*
Department of Medical Imaging, Affiliated Hospital of Jining Medical College, Jining, Shandong, PR China
#These authors contributed equally to this work
- *Corresponding Author:
- Yueqin Chen
Department of Medical Imaging
Affiliated Hospital of Jining Medical College, PR China
Accepted on July 26, 2017
Abstract
Objective: To analyse the diagnostic value of multi-slice spiral CT and magnetic resonance imaging in treatment of Hepatic Veno-Occlusive Disease (HVOD).
Methods: 30 cases of hepatic veno-occlusive disease treated in our hospital from January 12, 2015 to January 12, 2016 were selected as the objects and all patients were treated with multi-slice spiral CT and magnetic resonance imaging.
Results: All patients suffered degrees of liver injury and imaging examination results showed such symptoms as increased liver mass, liver ascites and uneven signal. Accuracy rate of the imaging diagnosis highly reached 93.33% with mere 2 cases of misdiagnosis.
Conclusion: Multi-slice spiral CT and magnetic resonance imaging have moderately high diagnostic accuracy in treatment of hepatic veno occlusive disease, enabling to carefully observe actual pathological changes of the patients and guide follow-up treatment of the disease thereby.
Keywords
Hepatic veno-occlusive disease, Multi-slice spiral CT, Magnetic resonance imaging, Diagnosis.
Introduction
Hepatic Veno-Occlusive Disease (HVOD) is also called hepatic sinus obstruction syndrome with low incidence in clinical practice [1-3]. Relevant studies point out that [4,5] the incidence of this disease has been recently increasing year by year, causing serious harm to the health of the patients. It occurs after ingestion of certain plant alkaloids such as pyrrolizidine alkaloids (in some herbal teas), and has been described as part of a rare hereditary disease called hepatic veno-occlusive disease with immunodeficiency. However, no specific treatment is available. Defibrotide is frequently used, mainly based on limited studies (historic comparisons) and because side effects are uncommon. Preventive treatment with heparin is often indicated, but its efficacy has not been proven. In case of hematopoietic stem cell transplantation, the main prophylactic treatment is the use of less hepatotoxic conditioning regimens.
The early diagnosis helps to guide the treatment of the disease. Diagnosis of HVOD is based on recognition of the clinical manifestations (hepatomegaly, jaundice, and weight gain) and their association with a potential cause of hepatic VOD (hematopoietic stem cell transplantation or chemotherapy, exposure to pyrrolizidine alkaloids), together with exclusion of other causes of liver disease. Liver biopsy is often indicated. Imaging studies, particularly hepatic Doppler-ultrasonography, may help to confirm the diagnosis. To conduct more in-depth analysis on the application effects of the imaging examination, multi slice spiral CT and magnetic resonance imaging are adopted in this study to analyse the application value of imaging.
Materials and Methods
Basic information
30 cases of HVOD treated in our hospital from January 12, 2015 to January 12, 2016 were selected as the objects with all confirmed by pathological examination. The medical staff have explained to all objects the process, importance and significance of this study in detail and conduct the study with the informed consent of all subjects; main clinical symptoms in the course of treatment include loss of appetite, diarrhea, abdominal pain, ascites, jaundice, and jugular venous distention with different degrees of percussion tenderness over hepatic region in all patients among whom there are 17 males and 13 females, aged from 21-68 with an average age of 45.22 ± 3.28.
Methods
Multislice spiral CT and MRI were performed in all patients.
A: Multi slice spiral CT test: Multi slice spiral CT has the advantages of wide inspection scope, relatively fast scanning speed, high resolution images and moderately good image quality, which attributes to the fact that this diagnostic measure enables to perform 3D reconstruction and timely discover small lesions followed by detailed diagnosis. The thickness of and the distance between layers are both set as 5 mm. Before the test the patients were told to drink about 800 ml water and then 80 ml iohexol was given through cubital veins of the patients (3 ml/s), followed by the scan at three different phases. Arterial phase, portal venous phase and delayed phase scan were respectively performed from the superior margin of the diaphragm to the superior edge of the iliac crest with the window width and window level, in the process of diagnosis, respectively set as 180 and 50. Later the scanning parameter was reset to 1.25 mm with the tube voltage and tube current respectively as 120 kv and 250 mA.
B: Magnetic resonance imaging: PHILPS 1.5 T was selected to conduct the diagnosis by using respiratory gating with the body coil of 6 channels. T1 weighted imaging could be used to check injury sites of the patients with the echo time as 4.2 s, repetition time 1850 ns, Number of Excitation (NEX) 12 times, the layer’s thickness 8 mm, the layers distance 1 mm and the vision of 40 C. Axial fast spin echo scanning was performed by way of T2-weighted imaging and in terms of dynamic scan, the patients were required to hold the breath with 4-6 s for each time. Then 4 d THRIVE was applied for scanning and in this course, there will be 6 dynamics with the time of 5.5 s as the duration of each dynamic and 100 layers of image. In addition, 20 ml GD-DTPA was injected into the patient's body before the scanning followed by the scan at the time phase of 15 s, 40 s and 300 s. The scanning images were acquired and processed.
Judgment criteria
Patients suffered pain in the upper right site of liver and abdomen or clinical examination revealed liver enlargement; hyperbilirubinemia was detected with unexplained cause with total bilirubin level of serum above 4.2 mol/L; increasing extent of body weight of the patients was more than 2% with the exclusion of special circumstances. The result can be determined by liver biopsy, which can be performed by way of venous cannula for the patients with poor physical condition. The venous cannula method can be taken to detect Hepatic Venous Pressure Gradient (HVPG) of the patients with hepatic vein impaction followed by the analysis on the possibility of portal hypertension combined with the histological specimens [6-8].
Statistical processing
Count data were described as percentage (%) and measurement data Mean ± SD. Chi square test and T test were applied of statistical significance, P<0.05. Statistical software: SPSS 18.0 and Microsoft office excel.
Results
The results of both spiral CT imaging and MRI examination showed that all patients had such symptoms as increased liver mass of different degrees and massive ascites with the uneven density leading to uneven signal of diagnostic image. T2 WI examination of nuclear magnetic resonance showed high slice signal with shadow like the shape of "clouds" on the image. Arterial enhancement scan results showed a different degree of enhancement between the venous phase and the arterial phase with the appearance of "mottled" shape; the phenomenon was more significant after the enhancement scanning of the delayed phase.
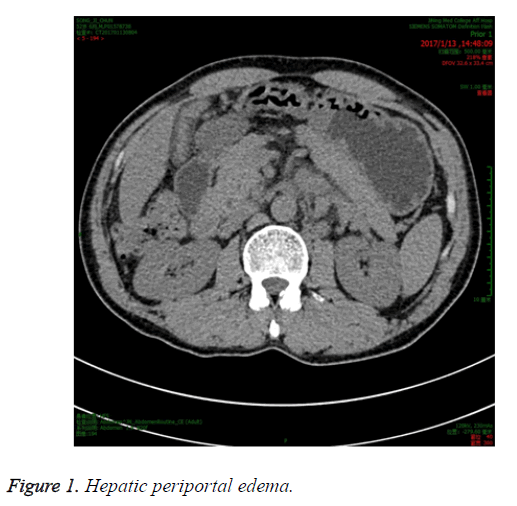
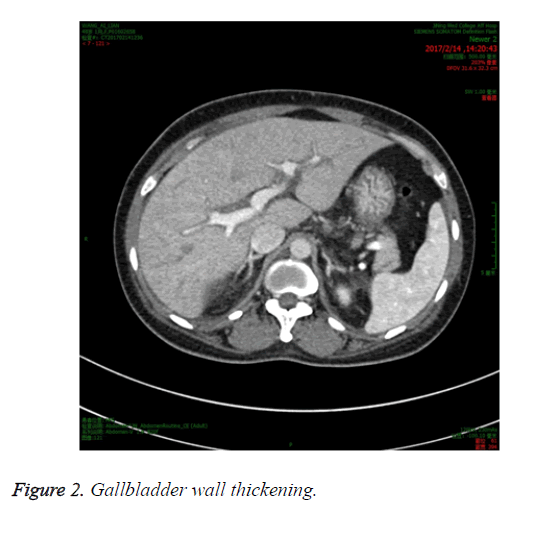
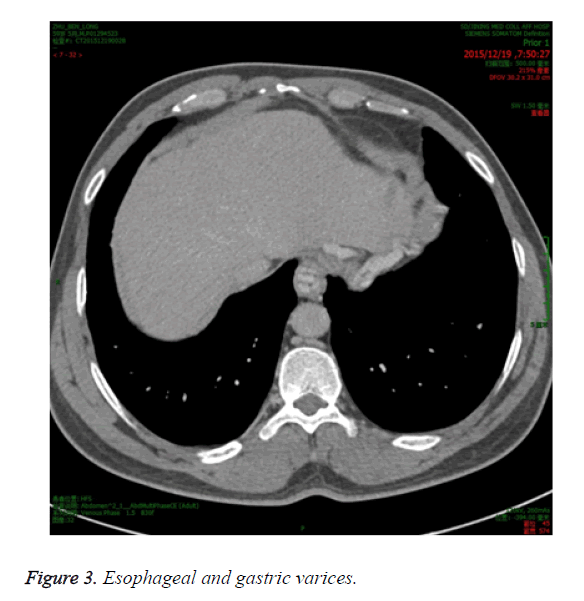
Among 30 patients, there were 15 cases of hepatic periportal edema (Figure 1), 11 cases of hydrops under the mucous membrane of gallbladder wall and gallbladder wall thickening (Figure 2); 4 cases of obviously visible esophageal and gastric varices (Figure 3), resulting in the thickening of intestinal tube with the branches of hepatic artery and portal vein pressed and narrowed and without significant change found during hepatic venous phase. Inferior vena cava, especially for liver segment, underwent different degrees of compression with no obvious hepatic collateral circulation.
The imaging diagnosis among all the patients confirmed 28 cases with diagnostic accuracy amounting to 93.33% (28/30) with mere 2 cases of misdiagnosis.
Discussion
At present specific causes for hepatic veno-occlusive disease remain to be defined in clinical practices [9,10]. But most patients have received the treatment for abdominal radiation and hematopoietic stem cell transplantation, which would cause small hepatic vein injury and affect its normal function. Thus, many fibrins gradually deposit in the small hepatic veins, hindering its normal circulation. And the patients usually have the symptoms like right upper abdominal pain, diarrhea, jaundice and liver palms [11-13].
The clinical study found that [14,15] deterioration factors impossible to induce the should be promptly blocked. For example, it is feasible to take large doses of radiotherapy as well as chemotherapy in the treatment of other malignant tumor patients and maintain acid-base balance in vivo as well as the stability of environment and renal perfusion. In addition, many clinical studies showed a moderately large effect of dose size on therapeutic effect in process of actual treatment and the low dose treatment enables to cure the patient with good results.
Patients with this kind of disease typically suffer damages of small hepatic vein endothelial cells, hepatic lobule, hepatic sinusoidal cell [16] and then fibrin deposition, resulting in the formation of many polymers in the endothelium and causing poor drainage of liver tissues. In clinical trials, it can be found that there were different degrees of damages in the liver tissues according to the actual blocking time, and the imaging features on different conditions will be found in the actual imaging examination [17,18]. All patients involved in this study were diagnosed by multi-slice spiral CT and magnetic resonance imaging and both are key detection schemes in clinical and help to discover more subtle changes of the lesion. And enhanced inspection and image processing are conducive to the early diagnosis of the disease with their characteristics given full play in treatment of the patients with such disease [19,20]. The results of this research showed that all the patients suffered different degrees of liver injury and imaging examination showed such symptoms as increased liver mass, liver ascites and uneven signal in the patients; and the accuracy rate of the imaging diagnosis highly reached 93.33% with mere 2 cases of misdiagnosis.
To sum up, multi-slice spiral CT and magnetic resonance imaging have moderately high diagnostic accuracy in the treatment of patients with hepatic veno-occlusive disease, enabling to observe actual pathological changes of the patients in detail and guide the follow up treatment.
References
- Yang S, Sun G, Zang R. Diagnostic value of multi-slice spiral CT and magnetic resonance imaging in treatment of hepatic veno occlusive disease. Chinese J Pract Med 2015; 42: 95-96.
- Bai J. Clinical value of multi-slice spiral CT and magnetic resonance imaging in the diagnosis of hepatic veno occlusive disease. World Clincal Med 2016; 10: 215.
- Kumamoto K, Mizuno S, Kuriyama N. Postoperative liver dysfunction in living donors after left-sided graft hepatectomy: Portal venous occlusion of the medial segment after lateral segmentectomy and hepatic venous congestion after left lobe hepatectomy. Transplant Proc 2012; 44: 332-337.
- Zhang L, Wu J, Xu H. Diagnosis and differential diagnosis of hepatic veno occlusive disease. J Interv Radiol 2012; 21: 987-990.
- Fu Z, Zhang G, Yi L. Clinical significance of spiral CT and magnetic resonance imaging in diagnosis of hepatic veno occlusive disease. Med Frontier 2015; 12: 47-48.
- Chen H, Shao H, Geng C. Diagnostic value of liver imaging in hepatic veno occlusive disease induced by gynura segetum. Clin Hepatol 2012; 28: 376-379.
- Tang W, Shi R, Liang B. Diagnostic value of dynamic contrast-enhanced CT in treatment of hepatic veno occlusive disease. Radiol Pract 2012; 27: 1235-1237.
- Zhu W, Chen S, Chen W. Cinical analysis on 50 cases of hepatic veno occlusive disease. Chinese J Digest 2012; 32: 620-624.
- Yin F. Clinical significance of spiral CT and magnetic resonance imaging in diagnosis of hepatic veno occlusive disease. Med Info 2013; 26: 219-220.
- Martins D, Deborah Penteado, Canola P, Alescio T, Luisa G. A reproducible venous thrombosis model in horses induced by the combination of an endothelial lesion and blood flow stasis. J Equine Veter Sci 2014; 34: 578-587.
- Shi T, He J, Shi J. CT imaging analysis of 37 cases of hepatic veno occlusive disease induced by gynura segetum. J Pract Radiol 2016; 32: 875-878.
- Wu X, Liu B, Yu Y. MDCT diagnosis and efficacy evaluation in treatment of hepatic veno occlusive disease. J Pract Radiol 2012; 28: 219-222.
- Guo W, Shi H, Ma X. CT diagnosis of hepatic veno occlusive disease. Chinese J Clin 2012; 6: 169-171.
- Xu X, Gong Y. The value of multi-slice spiral CT in the diagnosis of hepatic veno occlusive disease. Chinese J Med 2013; 15: 530-532.
- Jin X, Zhang K, Jin GQ. Diagnostic value of dynamic contrast-enhanced CT in treatment of hepatic veno occlusive disease. Clin Med Eng 2013; 20: 519-520.
- Kawaguchi Y, Ishizawa T, Miyata Y. Portal uptake function in veno-occlusive regions evaluated by real-time fluorescent imaging using indocyanine green. J Hepatol Eur Assoc Study Liver 2013; 58: 247-253.
- Zhang Y, Wang Y, Tian F. Clinical analysis and literature review on 6 cases of hepatic veno occlusive disease induced by gynura segetum. Pract Pharm Clin Remedies 2016; 19: 1137-1140.
- Zhang X. The clinical value of magnetic resonance imaging in the diagnosis of hepatic veno occlusive disease. Chinese J Health Nutr 2016; 26: 353.
- Zhang R, Leng A. Clinical analysis of 159 cases of hepatic veno occlusive disease induced by gynura segetum. The Second Summit Forum on Acute and Severe Clinical Experience 2015; 1-2.
- Yamagami T, Yoshimatsu R, Miura H. Successful balloon-occluded retrograde transvenous obliteration of gastric varix via pericardiacophrenic vein after embolization of portopulmonary venous anastomosis. J Vasc Interv Radiol 2013; 24: 137-139.