- Biomedical Research (2008) Volume 19, Issue 1
Vaginal delivery in large cephaloceles with good perinatal out-come (two case reports)
Papa Dasari*Department of Obstetrics and Gynaecology, JIPMER, Puducherry. India
- Corresponding Author:
- Papa Dasari
Department of Obstetrics and Gynaecology
JIPMER, Puducherry.
India
E-mail: pdasari@jipmer.edu
Accepted Date: November 17, 2007
Abstract
One may encounter Cephaloceles at term or in labour especially in developing countries where a second trimester USG is not feasible for most of the women. Two such cases are re-ported here. Diagnostic difficulties were encounterd in both cases. In the second case the Ul-trasonographic picture resembled that of a cystic hygroma. In both cases the cephalocele was the leading part during labour and as the cephalocele was very large rupture was pre-vented by careful cephalocentesis in the first case. As the prognosis was guarded and chro-mosomal anomalies could not be ruled out, vaginal delivery was undertaken. As there is controversy regarding the mode of delivery in literature, the outcome of vaginal delivery in these two cases is reported
Keywords
Cephalocele, Cystic hygroma, Vaginal delivery, Cephalocentesis
Introduction
Cephaloceles are protrusions of meninges with CSF herniating through a defect in cranial bones. When the brain tissue also herniates along, these are termed encephaloceles. The prognosis to the fetus is worse when there is herniation of brain tissue. The prenatal sonographic identification of encephalocele is easy, but the differentiation of a large cephalocele from soft tissue edema or cystic hygroma of the neck is difficult [1]. Recognition of the bony defect confirms the diagnosis but many defects are small, few mm in size [2]. Most often caesarean delivery is recommended in large cranial cephaloceles to achieve good perinatal outcome [3]. Two cases with good perinatal outcome following vaginal delivery are reported here.
Case 1
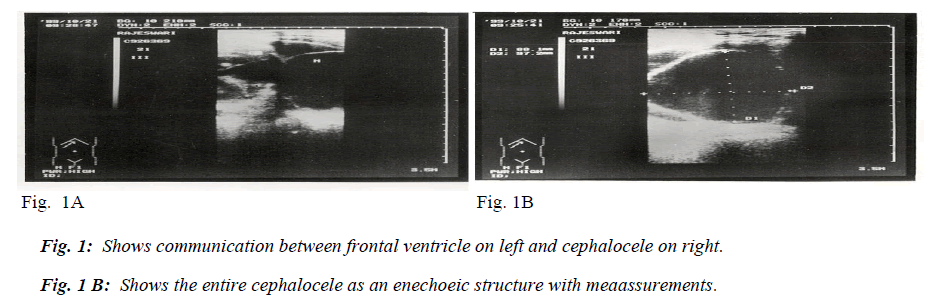
A 22-year-old primigravida at 35 weeks of gestation was referred to our institute as a case of polyhydramnios. Usg evalution showed an AFI of > 20 cm, single fetus in cephalic presentation. BPD measured 101 mm and there was mild bilateral ventriculomegaly. Ventricles were found to be communicating with another structure (Fig. 1A) near the frontal pole resembling another cephalic pole measuring 88 x 97 mm which was completely enechoeic (Fig. 1B). Spine and other structures were normal.
Labour was induced with oxytocin after ripening the cervix by PGE2 gel. ARM was avoided. The cephalocele was the presenting part. At about 8 cm dilatation, cephalocentesis was done with 22 gauge needle and 2 litres of CSF was drained under aseptic precautions. An alive female neonate weighed 2.8 kg was born with an apgar of 6/10 at 1 min and 8/10 at 5 min showed frontal cephalocele.
Case 2
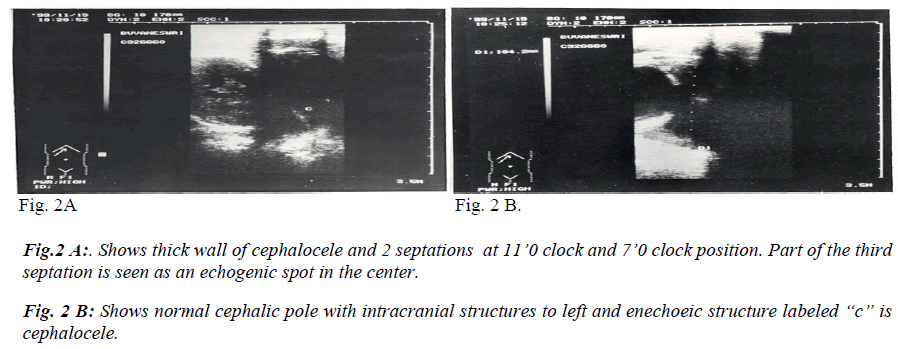
A 20-year-old unbooked primigravida was admitted in active phase of labour with history of premature rupture of membranes. On abdominal examination single live fetus with oblique lie was present with cephalic pole in left iliac fossa. Per vaginal examination showed cervix to be fully effaced 6 cm dilated and a tense cystic mass was felt high up at –4 cm station. On tracing, the mass ended near the neck of the fetus. Cephalic pole was not felt per vaginum an membranes were absent. Trans abdominal USG performed showed the following features. Single live fetus in oblique lie with the cephalic pole in left iliac fossa. The BPD measured 90 mm. A separate cystic mass with multiple septations (Fig. 2 A) was present near the occipital bone and no communication was seen between the mass and the cranial structures. Differentiation was not possible between a cystic hygroma and cephalocele.
Labour progressed normally and the mass descended down the vaginal canal with the cephalic pole and the malpresentation was spontaneously corrected to a vertex presentatation. An alive male fetus born with an apgar of 8/10 ‘weighed 2.4 kg had occipital cephalocele. Both neonates were referred to paediatric surgeon for further management. They underwent surgery for the same and were followed up for 2 years showed normal mile-stones.
Discussion
The incidence of cephalocele is approximately 1 in 2000 live births. They occur most commonly in occipital region but they can also occur in parietal, frontal and rarely in nasopharyngeal region [4]. Isolated cephaloceles are rare and one must look for associated anomalies like spinabifida and multiple anomalies in which case chromosomal abnormalities have to be ruled out. In a series of 8 cases of cephaloceles 5 had multiple congenital anomalies3. One can encounter cephaloceles at or near term when the patient has had no USG performed earlier or a small cephalocele was missed during the second trimester scan as most of them occur very early in pregnancy and are due to failure of closure of the rostral end of the neural tube.
The diagnosis is usually made easily by USG when the defect in the cranium is visible like in the first case. When the defect is not visible and there is absence of nonhomogenous appearance of the contents to suggest herniation of brain tissue, branchial cleft was diagnosed [4]. In the second case presence of septations and non-visuali-sation of defect made it difficult to defferentiate from cystic hygroma as described in the study of Chervenak FA and collegues [5].
The management of delivery in cephaloceles recognized for the first time near term is controversial. Caesarean section was advocated to avoid the possibility of obstructted labour [3].. However in these two cases obstructed labour did not result as the size is less than 10 cm and moreover it is compressible due to its cystic nature. The other concern is the possibility of rupture of cephalocele during vaginal delivery resulting in poor perinatal outcome. When the intrauterine pressure during labour is normal, i.e., when there is no hyperstimulation, and vaginal exmination is gentle and not frequent, the chances of rupture will be less. However, one must explain the prognosis to the parents as the prognosis will also depend on the post natal management of the neonate and not only on mode of delivery. Vaginal delivery was given in the first case as we expected the prognosis to be not so good due to mild dilatation of ventricles and in the second case the diagnosis of branchial cyst could not be excluded. Both the patients were young primigravidae and they opted for vaginal delivery accepting the possibility of trauma and poor neonatal outcome.
The good prognostic factors observed are isolated cephalocele and its frontal location and absence of hydrocephalous [6]. The prognosis is worse when there is herniation of brain tissue, microcephaly and other associated anomalies. Presence or absence of these factors and the wishes of the parents are to be taken in to account when one decides on the mode of delivery.
References
- Nicolini U, Ferrazzi E, Minonzio M et al. Prenatal diagnosis of cranial masses by Ultrasound: Report of 5 cases. J Clin Ultrasound 1983; 11: 170.
- Pearce JM, Little D, Campbell S. The diagnosis of abnormalities of the fetal central nervous System. P243. In Sanders RC,James AE (eds): The principles and practice of ultrasound in Obstetrics and Gynaecology. Appleton and hange E Norwalk, CT.1985.
- Chervenak AF, Issacson G, Mahoney JM, Berkowitz LR, Torotora M, Hibbins CJ. Diagnosis and management of fetal cephalocele. Obstet Gynecol 1984; 64: 86-90.
- Ingraham FD, Swah H: Spina bifida and cranium bifidum. A Survey of 546 cases. N Engl J Med 1943; 228: 559.
- Chervenak FA, Issacson G, Blakemore KJ et al: Fetal cystic hygroma: Cause and natural history. N Engl J Med. 1983; 309: 822
- Mealey J Ozenitis AJ, Hockley AA. The prognosis of encephaloceles. J Neurosurg 1970; 32; 209.