Case Report - Biomedical Research (2021) Volume 32, Issue 2
Use of application of navigation system to odontogenic benign tumors with maxilla.
Julia Koseki1*, Takahiro Abe1,3, Yoshiyuki Miyamoto1, Miki Kashiwagi1, Makiko Ishibashi1, Asako Taniguchi1, Hideyuki Suenaga1, Hiroyuki Abe2, Masanobu Abe1, Kazuto Hoshi1
1Department of Oral and Maxillofacial Surgery, The University of Tokyo Hospital, 7-3-1 Hongo, Bunkyo-ku, Tokyo 113- 8655, Japan
2Department of Pathology, The University of Tokyo Hospital, 7-3-1 Hongo, Bunkyo-ku, Tokyo 113-8655, Japan
3Department of Dentomaxillofacial Diagnosis and Treatment, Graduate School of Kanagawa Dental University, 1-23 Ogawacho, Yokosuka 238-8580, Japan
- Corresponding Author:
- Julia Koseki Department of Oral and Maxillofacial Surgery
The University of Tokyo Hospital
7-3-1 Hongo, Bunkyo-ku
Tokyo
Japan
Accepted date: February 09, 2021
Abstract
Oral and maxillofacial region has a complicated anatomy with critical nerves and arteries inside. Therefore, oral surgeons sometimes do not have enough operative fields during surgeries and anatomic changes caused by tumors and fractures make the surgeries more difficult. The application of navigation system in oral surgery has started in such cases that tumors are close to cranial base and have risks to damage important anatomical structures like nerves and vessels. It can make doctors more confident with their operations and decrease operative risks, but the use is still limited because of several obstacles. In this context, we applied navigation system to the operations of removing recurrent ameloblastoma on sphenoid bone and myxoma. The surgeries we performed with navigation system were successful and we have not had any postoperative complications at all. This report presents to use navigation system to remove benign tumor that occurs in deep area of craniofacial bone completely in a minimally invasive way.
Keywords
Navigation system, Odontogenic tumor resection, Ameloblastoma.
Introduction
For surgeons, it is always a critical issue whether it is possible to resect tumors from patient’s body safely or not. The more deeply tumors invade inside, the more difficult surgeries become due to its complicated anatomy. To solve this problem, navigation system has been introduced in the field of neurosurgery, head and neck surgery, orthopedic surgery and hepato-biliary-pancreatic surgery, and its effectiveness has been recognized widely in these field. Therefore, navigation system and robot-assisted surgery like DaVinci have been developed rapidly [1-3] and become mainstream to minimize surgical stress. In the field of hepato-biliary-pancreatic surgery, navigation system using projection mapping and fluorescently labeled antibody is developed and used [4]. In oral surgery, on the other hand, navigation system has been applied to reconstruction of fractured bones [5,6], osteotomy [7-10], dental implants, removal of foreign bodies [11] and tumor resection [12- 16]. Recently, we applied a navigation system to the resection of relapsed ameloblastomas and myxoma that were close to skull base and orbit. Here we report those cases to confirm the effectiveness of navigation system in oral surgery along with related literature surveys.
Case Series
Case 1
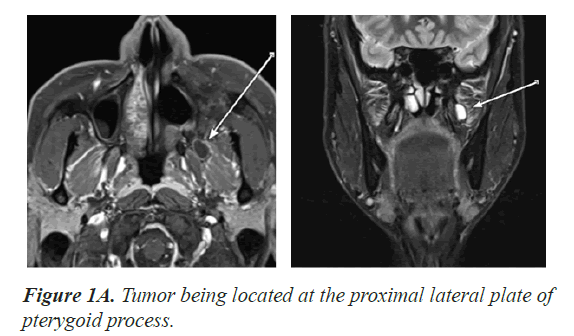
The first case was for a 37-year-old male patient who experienced reoccurrences of ameloblastomas twice, in 2002 and 2010. In 2002, he felt swelling with his left cheek, and had medical examination at a dental hospital. The cause of the swelling was diagnosed as a cyst, and the excision of the cyst was conducted. In 2010, he felt swelling again and the reoccurrence of ameloblastoma was pointed out at the same hospital. He was proposed to have an operation with Weber incision. However, since he did not want skin incision in his face, he came to our hospital to ask for the first medical examination. In the same year, an intraoral operation was done; after the surgery, his oral cavity was opened to left sinus and he was requested to use a maxillary prosthetic. In 2016, unfortunately the third reoccurrence was identified. The reoccurrence was recognized at the proximal lateral plate of pterygoid process. Since a tendency of its increase in size was identified, we decided to move on to resection by surgery. The area of the surgery was really narrow and close to the cranial base, as shown in Figure 1A, we also decided to use a navigation system.
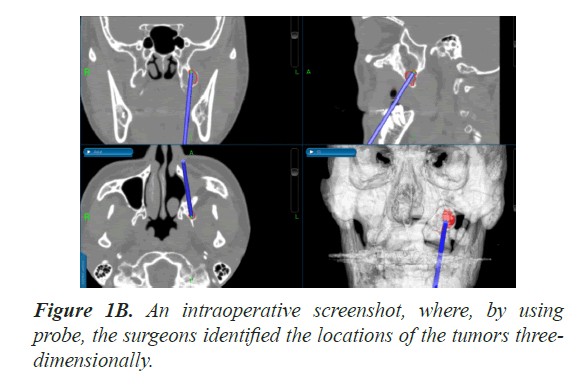
We used the magnetic field navigation system (Stealth Station S7, Medtronic). First, we put the emitter next to the patient’s head and patient tracker on the forehead of the patient. Then, we traced the forehead and dorsum of nose to register the positional information with images so that we could simulate the surgery using the images in advance. After this operation, we started the surgery. We cut just above the tumor and exfoliated the mucoperiosteal flap. We removed tumor carefully checking the location and anatomical structures around tumor by navigation system, as shown in Figure 1B. After we removed the tumor, we removed the surface of bones by cutting with round bur. We also checked if there was no remaining of the tumor by comparing the actual anatomical structures with CT images that we draw our plan on for excision. Though there was a risk of postoperative bleeding by damaging pterygoid venous plexus, the patient showed steady progress without any surgical complications. We now check his condition regularly, but have not identified any symptoms of the reoccurrence of ameloblastoma.
Case 2
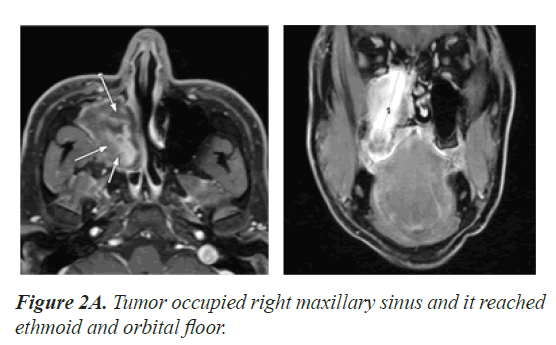
The second case was for a 35-year-old male patient suffering from odontogenic myxoma. He had an experience of the treatment and osteotomy to cure jaw deformity. In 2014, the existence of cystic lesion was found in his right maxillary sinus by panoramic radiographs of his dental treatment. Three years later, he noticed nasal congestion with his right side. He had a fine-needle aspiration biopsy with the right maxillary sinus and a computed tomographic sonography. Then, odontogenic myxoma was suspected and he came to see us finally. We also took MRI and contrast-enhanced CT and decided to use navigation system as the tumor occupied his right maxillary sinus and it eroded the maxillary bone in front of the sinus. What is worse is that it reached ethmoid horizontally and orbital floor vertically, as shown in Figure 2A.
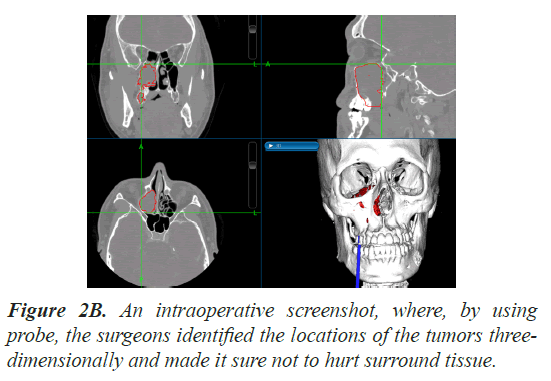
In the operation, we set up the navigation system similarly to the first case and registered the patient’s positional information with images. We cut into with Matis incision and extracted the right first premolar. Then, we removed the thinned alveolar bone of the right first and second molars and the former and side bones of maxillary sinus to have an enough field of operation. We peeled off the tumor from the maxillary sinus and removed it by using navigation system in order not to hurt the surrounding tissues, as shown in Figure 2B. After removing the tumor, we also used endoscope with some otolaryngologists to check if tumor was not left and if there was no abnormal bleeding. The patient showed steady progress without any surgical complications after the surgery. We have not identified any symptoms of the reoccurrence of myxoma so far.
Discussion
As we experienced this time, maxillary benign tumors sometimes invade around the area of sphenoid bone and orbit, and mandible tumors invade around carotid artery with a possibility of reaching the area of sphenoid bone passing through pterygomandibular space. The tumor having such features increases the difficulty of surgery.
For example, ameloblastoma is a benign but aggressive tumor found in mandible (80%) and maxilla (20%) [17]. Especially, ameloblastoma in maxilla is often difficult to be detected in early stages and can invade into soft tissue and the vicinity. In the worst case, ameloblastoma can turn into carcinoma with lung metastases after suffering several relapses [18,19]. The treatment of ameloblastoma is usually performed by either radical resection or conservative resection [18,20]. Several studies have reported that its recurrence rate depends on the way of surgeries [18,21,22]. A wide range of the recurrence rate has been reported [23], but generally in those studies, conservative treatment showed a higher recurrence rate than radical treatment. In other studies, the recurrence rate of maxillary ameloblastoma was thought to depend on the site character (anterior/posterior of upper jaw), root resorption and presence of maxillary sinus invasion irrespective of the surgical methods [24]. In terms of resection margins, by taking into consideration the character of tumor, it is recommended to resect tumor with sufficient margin. Carlson et al. recommended 1 to 1.5 cm resection margins with radical resection [25]. According to De Silva et al., tumor cells are often found to extend by 2 to 8 mm beyond the clinical margin given by microscopic examination [26]. However, it is sometimes difficult to have enough margins depending on tumors’ anatomical position. This discussion is shared with our second case of myxoma. Myxoma is also a benign tumor that is classified as an odontogenic and maxillofacial bone tumor but locally aggressive and invasive tumor [27]. Therefore, some study recommended surgical resection with a minimum bone margin of 1 cm [28]. However, such operations may be difficult if conducted only by oral surgeons, and if the tumors are odontogenic, it would be all the more complicated. Since surgical procedures always accompany the risks of recurrence and the loss of function and aesthetics, more minimally invasive and effective options are always wanted.
Since 1990’s, navigation system has been used in the field of neurosurgery, head and neck surgery and orthopedic surgery. The navigation system can be divided two types; optical type and electromagnetic type. In optical type, we use navigation probe in combination with a reference flame aside of the patient’s head or a reflector on the head of the patient, where the infrared sensor recognizes the flame or the reflector and detects the anatomical position. However, there is a limitation. When other instruments or a person interrupt the detection, navigation system that regulates operator’s position during surgery will not work correctly. On the other hand, electromagnetic system uses electromagnetic fields to detect the navigation probe position, so the operator’s position will not be a problem at all. Therefore, we chose electromagnetic type this time.
There are several reasons why navigation system can help surgeons perform better surgery. First, by simulating and setting the area of tumor before surgery, surgeons can check whether the tumor can be completely resected or not. Also, simulation using navigation system allows surgeons to think about the most minimally invasive way in the surgery of interest [29]. Second, it can visualize the area of the tumor of interest and the relationship between the location of the tumor and adjacent anatomical structures three-dimensionally with help of CT and MRI images in real-time during the surgery. It is reported that the accuracy is less than 1-2 mm [11]. This reliability helps the surgeons resect not only benign tumors but also malignant ones without hurting untargeted anatomical structures. Moreover, if the surgeons put a mark and draw a line on CT or MRI data before the surgery, it is possible to show them during surgeries [16,30]. Also, Ivashchenko suggests that the combination with Cone-beam CT helps surgeons to make an adequate intraoperative assessment of planned surgical margins of maxillary tumors [31].
On the other hand, there are some disadvantages for the use of the system. First, navigation system requests the registration of exact location in advance, and if doctors fail this operation, the location pointed by the system could be wrong and the use of navigation system is meaningless. Some studies suggest that dorsal and dorsal cranial tumors that extend behind Ohngren’s line have a higher risk of incomplete resection due to difficulties of proper evaluation of preoperative imaging [32]. Also, when we have to perform surgery in emergency, the setting of the system is time-consuming. Second, the system is still expensive, which may make medical disparity between hospitals and between doctors. Third, at the moment, the application of the system is limited to neurosurgery, head and neck surgery and orthopedic surgery. Therefore, if odontogenic tumors invade around orbit or cranial base, oral surgeons have to collaborate with other departments. Moreover, when mandible is the target of the operation, oral surgeons have to deal with the operation using mirrorimage of unaffected side of mandible [14], mounting a dynamic reference frame directly on the mandible or using occlusion splint to fix the mandible with a defined position against maxilla. These strategies using direct tracking system via sensor or splint are sensitive to the relative movement of the mandible and are likely to lose accuracy during the surgery [11].
To solve these problems, new techniques and systems have been developed. Wang et al presented an augmented reality navigation system with automatic maker-free image registration using 3-D image overlay [2] . The technique for accurate registration has also been examined by others [14,33-35]. In near future, these technologies could make surgeries using navigation system easier and more reliable
Acknowledgement
The author would like to thank Dr. K.Kondo, Dr. H.Nishijima, the Department of Otolaryngology, Head and Neck Surgery, University of Tokyo Hospital, for his technical contribution to this study.
Ethical Approval
Not applicable.
Conflict of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Kim Y, Kim H, Kim YO. Virtual Reality and Augmented Reality in Plastic Surgery: A Review. Arch Plast Surg 2017; 44: 179-187.
- Wang J, Suenaga H, Hoshi K, Yang L, Kobayashi E, Sakuma I. Augmented reality navigation with automatic marker-free image registration using 3-D image overlay for dental surgery. IEEE Trans Biomed Eng 2014; 61: 1295-1304.
- Liu HH, Li LJ, Shi B, Xu CW, Luo E. Robotic surgical systems in maxillofacial surgery: A review. Int J Oral Sci 2017; 9: 63-73.
- Nishino H, Hatano E, Seo S, Nitta T, Saito T, Nakamura M. Real-time Navigation for Liver Surgery Using Projection Mapping With Indocyanine Green Fluorescence: Development of the Novel Medical Imaging Projection System. Ann Surg 2018; 267: 1134-1140.
- Pham AM, Rafii AA, Metzger MC, Jamali A, Strong EB. Computer modeling and intraoperative navigation in maxillofacial surgery. Otolaryngol Head Neck Surg 2007; 137: 624-631.
- Han C, Dilxat D, Zhang X, Li H, Chen J, Liu L. Does Intraoperative Navigation Improve the Anatomical Reduction of Intracapsular Condylar Fractures? J Oral Maxillofac Surg 2018; 76: 2583-2591.
- Yu H, Shen SG, Wang X, Zhang L, Zhang S. The indication and application of computer-assisted navigation in oral and maxillofacial surgery-Shanghai's experience based on 104 cases. J Cranio-maxillofacial Surg 2013; 41: 770-774.
- Zhu M, Liu F, Zhou C, Lin L, Zhang Y, Chai G. Does intraoperative navigation improve the accuracy of mandibular angle osteotomy: Comparison between augmented reality navigation, individualised templates and free-hand techniques. J Plast Reconstr Aesthet Surg 2018; 71: 1188-1195.
- Tsai CY, Chang YJ, Wu TJ, Lai JP, Chen TY, Lin SS. Blood loss and operative time associated with orthognathic surgery utilizing a novel navigation system in cleft lip and palate patients. J Formos Med Assoc 2019; 118: 588-599.
- Lin L, Fan B, Yu Z, Xu L, Yuan J, Wu J. Application of computer-assisted navigation in mandibular angle osteotomy. J Int Med Res 2019; 47: 3160-3170.
- Sukegawa S, Kanno T, Furuki Y. Application of computer-assisted navigation systems in oral and maxillofacial surgery. Jpn Dent Sci Rev 2018; 54: 139-149.
- Kawachi H, Kawachi Y, Ikeda C, Takagi R, Katakura A, Shibahara T. Oral and maxillofacial surgery with computer-assisted navigation system. Bull Tokyo Dent Coll 2010; 51: 35-39.
- Catanzaro S, Copelli C, Manfuso A, Tewfik K, Pederneschi N, Cassano L. Intraoperative navigation in complex head and neck resections: indications and limits. Int J Comput Assist Radiol Surg 2017; 12: 881-887.
- Wu J, Sun J, Shen SG, Xu B, Li J, Zhang S. Computer-assisted navigation: its role in intraoperatively accurate mandibular reconstruction. Oral Surg Oral Med Oral Pathol Oral Radiol 2016; 122: 134-142.
- Yu H, Wang X, Zhang S, Zhang L, Xin P, Shen SG. Navigation-guided en bloc resection and defect reconstruction of craniomaxillary bony tumours. Int J Oral Maxillofac Surg 2013; 42: 1409-1413.
- Rana M, Essig H, Eckardt AM, Tavassol F, Ruecker M, Schramm A. Advances and innovations in computer-assisted head and neck oncologic surgery. J Craniofac Surg 2012; 23: 272-278.
- Adeel M, Rajput MSA, Arain AA, Baloch M, Khan M. Ameloblastoma: Management and Outcome. Cureus 2018; 10: e3437.
- Effiom OA, Ogundana OM, Akinshipo AO, Akintoye SO. Ameloblastoma: current etiopathological concepts and management. Oral Dis 2018; 24: 307-316.
- Yang R, Liu Z, Gokavarapu S, Peng C, Ji T, Cao W. Recurrence and cancerization of ameloblastoma: multivariate analysis of 87 recurrent craniofacial ameloblastoma to assess risk factors associated with early recurrence and secondary ameloblastic carcinoma. Chin J Cancer Res 2017; 29: 189-195.
- Abe M, Zong L, Abe T, Hoshi K. A turning point in therapy for ameloblastomas. Oral Oncol 2018; 80: 95-96.
- Antonoglou GN, Sandor GK. Recurrence rates of intraosseous ameloblastomas of the jaws: a systematic review of conservative versus aggressive treatment approaches and meta-analysis of non-randomized studies. J Craniomaxillofac Surg 2015; 43: 149-157.
- Laborde A, Nicot R, Wojcik T, Ferri J, Raoul G. Ameloblastoma of the jaws: Management and recurrence rate. Eur Ann Otorhinolaryngol Head Neck Dis 2017; 134: 7-11.
- Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: biological profile of 3677 cases. Eur J Cancer B Oral Oncol 1995; 31: 86-99.
- Yang R, Liu Z, Peng C, Cao W, Ji T. Maxillary ameloblastoma: Factors associated with risk of recurrence. Head Neck 2017; 39: 996-1000.
- Carlson ER, Marx RE. The ameloblastoma: primary, curative surgical management. J Oral Maxillofac Surg 2006; 64: 484-494.
- De Silva I, Rozen WM, Ramakrishnan A, Mirkazemi M, Baillieu C, Ptasznik R. Achieving adequate margins in ameloblastoma resection: the role for intra-operative specimen imaging. Clinical report and systematic review. PLoS One 2012; 7: e47897.
- Chrcanovic BR, Gomez RS. Odontogenic myxoma: An updated analysis of 1,692 cases reported in the literature. Oral Dis 2019; 25: 676-683.
- Takahashi Y, Tanaka K, Hirai H, Marukawa E, Izumo T, Harada H. Appropriate surgical margin for odontogenic myxoma: a review of 12 cases. Oral Surg Oral Med Oral Pathol Oral Radiol 2018; 126: 404-408.
- Tarsitano A, Ricotta F, Baldino G, Badiali G, Pizzigallo A, Ramieri V. Navigation-guided resection of maxillary tumours: The accuracy of computer-assisted surgery in terms of control of resection margins - A feasibility study. J Craniomaxillofac Surg 2017; 45: 2109-2114.
- Schramm A, Suarez-Cunqueiro MM, Barth EL, Essig H, Bormann KH, Kokemueller H. Computer-assisted navigation in craniomaxillofacial tumors. J Craniofac Surg 2008; 19: 1067-1074.
- Ivashchenko O, Pouw B, de Witt JK, Koudounarakis E, Nijkamp J, van Veen RLP,. Intraoperative verification of resection margins of maxillary malignancies by cone-beam computed tomography. Br J Oral Maxillofac Surg 2019; 57: 174-181.
- Kreeft AM, Smeele LE, Rasch CR, Hauptmann M, Rietveld DH, Leemans CR. Preoperative imaging and surgical margins in maxillectomy patients. Head Neck 2012; 34: 1652-1656.
- Ohba S, Yoshimura H, Ishimaru K, Awara K, Sano K. Application of a real-time three-dimensional navigation system to various oral and maxillofacial surgical procedures. Odontology 2015; 103: 360-366.
- Hwang YE, Kang SH, Kim HK. Errors according to the number of registered markers used in navigation-assisted surgery of the mandible. Head Face Med 2019; 15: 6.
- Wang J, Shen Y, Yang S. A practical marker-less image registration method for augmented reality oral and maxillofacial surgery. Int J Comput Assist Radiol Surg 2019; 14: 763-773.