Case Report - Otolaryngology Online Journal (2022) Volume 12, Issue 2
Unilateral Tongue Atrophy and Myosteatosis: A Late Surgical Complication
Pedro Marques Gomes*, Joana Borges Costa, Nuno Oliveira, Delfim Duarte, Paula AzevedoOtolaryngology Department, Unidade Local de Saúde de Matosinhos, Porto, Portugal
- Corresponding Author:
- Pedro Marques Gomes
Department of Otolaryngology
Unidade Local de Saúde de Matosinhos Porto
Zip code: 4464 513, Porto, Portugal
E-mail: pedrommarquesgomes@hotmail.com
Received: 31-Dec-2021, Manuscript No. JORL-22-53543; Editor assigned: 3-Jan-2022, PreQC No. JORL-22-53543 (PQ); Reviewed: 17-Jan-2022, QC No JORL-22-53543; Revised: 2-Feb-2022, Manuscript No. JORL-22-53543 (R); Published: 9-Feb-2022, DOI: 10.35841/2250-0359.12.1.255
Keywords
Unilateral hypoglossal nerve palsy, Neurogenic muscular atrophy, Myosteatosis, Acoustic neuroma, Neurosurgery
Introduction
The hypoglossal nerve (XII), a purely motor nerve, originates at the base of the 4th ventricle, ending in the extrinsic and intrinsic muscles of the tongue, except for the palatoglossus muscle. It is responsible for the movement and shape of the tongue, playing a vital role in swallowing and speaking [1].
The lesion of the hypoglossal nerve may be associated with hypomobility of half of the tongue. Cases of isolated damage to the hypoglossus are rare. Possible causes include neoplasms, trauma, infections, endocrine, autoimmune, vascular, iatrogenic, and idiopathic causes [2]. In some rare cases, adipose infiltration (myosteatosis) may occur after the muscle atrophy [3].
This paper presents a case of unilateral neurogenic atrophy of the tongue, with myosteatosis, after hypoglossal nerve injury in an acoustic schwannoma neurosurgery.
Case Report:
A female patient of 89 years old was referred to the Otorhinolaryngology department with worsening dysphagia. She had a history of severe degree dementia of mixed etiology (alcoholic, degenerative and vascular) and left acoustic neuroma neurosurgery, over 30 years ago.
Physical examination revealed swelling of the left half of the tongue, with regular surface and elastic consistency and ipsilateral tongue palsy.
Fiberoptic endoscopic evaluation of swallowing showed dysphagia mainly attributed to pharyngolaryngeal dysmotility related to the dementia, with little contribution from lingual dysmotility.
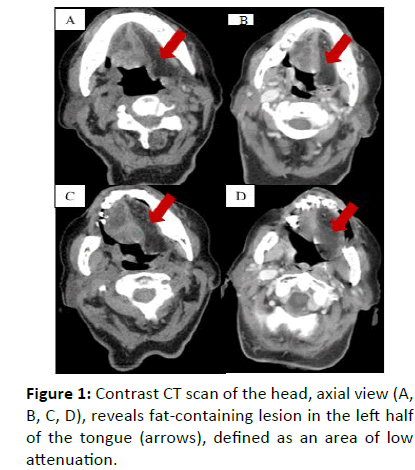
A CT scan of the head revealed myosteatosis of the intrinsic muscles of the tongue on the left (arrows), with bulging of the ipsilateral tongue base.
Considering the imaging findings biopsy was not performed.
Discussion:
Unilateral hypoglossal nerve damage has several possible etiologies. In the initial phase of the injury, a pattern of tissue edema is usually observed, followed by muscle atrophy and muscle replacement by adipose tissue in chronic and prolonged cases [3]. It is common to observe in these patients a swelling of the base of the tongue that may be confused by a tumor.
In this case it was essential to evaluate the patient's personal history and imaging findings to establish the etiology of the swelling and hypoglossal nerve palsy, thus avoiding an unnecessary biopsy.
Conclusion:
The otolaryngologist must take in account neurogenic unilateral atrophy of the tongue with myosteatosis as a possible differential diagnosis in tongue swellings.
Acknowledgements:
Not applicable.
Author Contributions:
PMG: patient management with JBC and NO and wrote the drafts and final article.
Conflict of Interest:
No conflict of interest was declared by the author.
Ethical Approval:
The study has been approved by the appropriate ethics. Published with consent of the patient family.
References
- Jain A, Kneale E, Böckeler G (2010) Unilateral neurogenic atrophy of the tongue. EURORAD Head Neck Imaging: Clinical Cases 1-8.
- Freedman M, Jayasundara H, Stassen LF (2008) Idiopathic isolated unilateral hypoglossal nerve palsy: a diagnosis of exclusion. Oral Surg Oral Med Oral Pathol Oral Radiol Endodonto 106:e22-6.
- Russo CP, Smoker WR, Weissman JL (1997) MR appearance of trigeminal and hypoglossal motor denervation. AJNR: Am J Neuroradiol 18(7):1375.
Indexed at, Google Scholar, Cross Ref