Commentary - Biomedical Research (2017) Volume 28, Issue 12
Underweight is associated with periodontitis among Korean female adults
Kyungdo Han1 and Jun-Beom Park2*
1Department of Biostatistics, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea
2Department of Periodontics, College of Medicine, The Catholic University of Korea, Seoul, Republic of Korea
- *Corresponding Author:
- Jun-Beom Park
Department of Periodontics
The Catholic University of Korea
Republic of Korea
Accepted date: May 08, 2017
Abstract
The relationship between underweight and periodontitis has not been well revealed. This study was performed to assess the relationship between underweight, defined by body mass index, and periodontitis, using nationally representative data. The final number of participants in this study was 3,285, and they were surveyed using the Korean National Health and Nutrition Examination Survey. An association between periodontitis and body mass index was obtained using multivariate logistic regression models after adjustment for age, frequency of tooth brushing per day, self-reported oral status, waist circumference, white blood cell count, smoking, drinking, and walking. Adjusted odds ratios and their 95% confidence intervals for periodontitis in men was 0.614 (0.126-2.987), 1 (reference), 1.103 (0.668-1.821), and 1.300 (0.726-2.328), for a body mass index of <18.5, 18.5 ≤ x<23, 23 ≤ x<25, and ≥ 25 kg/m2, respectively, after adjustment. Adjusted odds ratios and their 95% confidence intervals for periodontitis in women was 2.400 (1.028-5.605), 1 (reference), 1.152 (0.594-2.235), and 0.971(0.416-2.268), for a body mass index of <18.5, 18.5 ≤ x<23, 23 ≤ x<25, and ≥ 25 kg/m2, respectively, after adjustment. Conclusively, the association between underweight, defined by body mass index, and periodontitis was proven among Korean female adults by multiple logistic regression analyses after adjusting for confounding factors.
Keywords
Epidemiology, Health surveys, Oral health, Periodontitis
Abbreviations
CPI: Community Periodontal Index
Introduction
Previous reports have shown that a high body mass index is associated with general health [1]. It was shown that a high body mass index were associated with the osteoarthritis of the knee defined by Kellgren-Lawrence grading scale [1,2]. A previous study explored factors affecting cardiorespiratory fitness with different values for body mass index, and it was shown that obese male subjects, defined by body mass index, with diabetes had a lower estimated maximal oxygen uptake [2]. Similarly, previous research reported that an increase in body mass index was associated with greater leg pain scores [3]. The association between obesity and periodontal diseases has been suggested in previous reports. In the overweight and obese groups, the odds ratios for periodontitis were 1.27 (95% confidence of interval of 1.10 and 1.48) after adjustments [4]. A previous report has shown that obesity defined by body mass index was associated with increased levels of pathogens associated with periodontitis [5]. Resistin, an adipocyte-derived hormone from gingival crevicular fluid, was higher in obese participants with periodontitis when compared with non-obese subjects with healthy periodontium [6]. However, the relationship between underweight and periodontitis is not well revealed. It was hypothesized that there is no statistically significant association between underweight and periodontitis. Thus, this study was performed to assess the relationship between underweight, defined by body mass index, and periodontitis using nationally representative data.
Material and methods
Subjects
Findings from the Korean National Health and Nutrition Examination Survey conducted between 2012 and 2014 were used for this study. Informed consent was obtained from all the participants. The Institutional Review Board of the Korea Centers for Disease Control approved the Korean National Health and Nutrition Examination Survey, and this study was performed based on the Helsinki Declaration-based ethical principles for medical research involving human subjects. The design of this study was approved by the Review Board at Seoul St Mary’s Hospital, the Catholic University of Korea (KC14EISI0636).
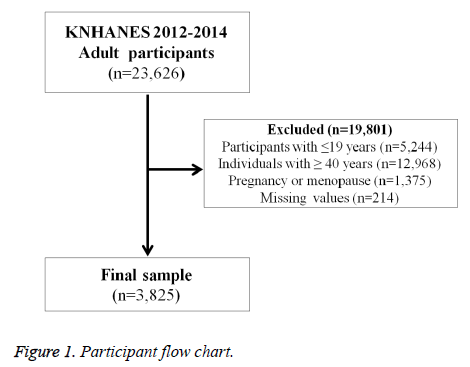
A total of 23,626 participants were candidates from the Korean National Health and Nutrition Examination Survey survey. The number was reduced to 18,382 by excluding the participants younger than 19. The number was 5,414 by excluding the participants 40 or older. The individuals with pregnancy or menopause were excluded from this study. The final number of individuals was 3,285 for this study after excluding the participants with missing values (Figure 1).
Measurement and classification of variables
Staff members with training performed anthropometric measurements for this study. Body mass index was measured by the following calculation: weight (kg) divided by squared height (m2). Measurement of waist circumference was done at the time of the end of normal expiration at the level midway between the costal margin and the iliac crest.
Smoking status was categorized as current smoker or not and was derived from the interview. Individuals were categorized as heavy drinkers if the individuals declared that they consumed more than 30 g in their answers to the self-reported questionnaire [7]. Individuals were regarded as regular exercisers if they performed walking at least 5 times per week for at least 30 minutes per session. Economic status was categorized as the lowest quartile, which included households with a monthly income <$1092.4. Education level was categorized as university graduate or higher. Residential areas were categorized into urban areas in the case of administrative divisions of “dong” [8].
Metabolic syndrome was defined based on the American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement criteria for Asians [9]. Three or more of the following must be fulfilled to be diagnosed with metabolic syndrome: use of lipid-lowering medication or fasting triglycerides ≥ 150 mg/dL; use of cholesterol-lowering medication or high-density lipoprotein cholesterol <40 mg/dL in men and <50 mg/dL in women; waist circumference ≥ 90 cm in men and ≥ 80 cm in women; use of antihypertensive medication or blood pressure ≥1 30/85 mm Hg; or current use of antidiabetic medication or fasting blood glucose ≥ 100 mg/dL.
Oral health behaviors and number of natural teeth
The time of day of the participants’ tooth brushing was recorded, and the frequency of tooth brushing per day was calculated based on the interview. Self-reported oral status was categorized into three: favorable, average, and problematic. Dental checkup within a year was also evaluated. The presence of periodontitis was evaluated using the World Health Organization community periodontal index (CPI). Presence of periodontitis was defined if CPI score was ≥ 3 according to the previous report [10]. Dental checkup was also evaluated.
Statistical analysis
The data are presented as means ± standard errors for continuous variables and as proportions (standard errors) for categorical variables. A chi-square test for categorical variables or an independent t-test for continuous variables was performed to assess the differences in characteristics categorized by the presence of periodontitis. Sensitivity test was performed to evaluate the interactions of parameters with periodontitis. A multivariable logistic regression analysis was used to evaluate the odds ratios of periodontitis in relation to body mass index. Model 1 was adjusted for age, whereas Model 2 was adjusted for age, frequency of tooth brushing per day, self-reported oral status, waist circumference, and white blood cell count. In Model 3, adjustments were made for the variables in Model 2 plus smoking, drinking, and walking.
Results
Table 1 shows the characteristics of the participants of the present study categorized by sex according to the presence of periodontitis. Regardless of sex, the average age was higher with the presence of periodontitis (P<0.05). The average body mass index was significantly higher in female participants with periodontitis (P<0.05). Average waist circumference was statistically higher with the presence of periodontitis regardless of sex (P<0.05).
| Variables | Male | Female | ||||
|---|---|---|---|---|---|---|
| Periodontitis | ||||||
| No | Yes | P-value | No | Yes | P-value | |
| Unweighted n | 1,872 | 225 | 1,624 | 104 | ||
| Age (years) | 29 ± 0.2 | 33.1 ± 0.4 | <0.0001 | 29.1 ± 0.2 | 33.6 ± 0.6 | <0.0001 |
| Body mass index (kg/m2) | 24.2 ± 0.1 | 24.6 ± 0.2 | 0.0944 | 21.8 ± 0.1 | 23 ± 0.5 | 0.0226 |
| Waist circumference (cm) | 82.7 ± 0.3 | 84.5 ± 0.7 | 0.0111 | 72.7 ± 0.3 | 76.7 ± 1.3 | 0.0031 |
| Number of natural teeth | 27.45 ± 0.04 | 26.92 ± 0.17 | 0.0024 | 27.35 ± 0.04 | 26.93 ± 0.2 | 0.0323 |
| Smoking (current) | 40.5 (1.3) | 56.1 (3.7) | <0.0001 | 7.7 (0.9) | 8.5 (3.3) | 0.8045 |
| Heavy drinker (>30g/day) | 14.5 (0.9) | 19.5 (3.2) | 0.0900 | 4.6 (0.8) | 2.4 (1.6) | 0.3276 |
| Walking (yes) | 12.0 (1.2) | 8.3 (1.1) | 0.0174 | 5.8 (0.8) | 5.6 (1.0) | 0.8793 |
| Income (lowest quartile) | 7.4 (0.8) | 8.0 (1.9) | 0.7585 | 5.5 (0.7) | 12.7 (3.9) | 0.0093 |
| University degree or higher | 45.9 (1.5) | 46.3 (3.8) | 0.9134 | 52.4 (1.6) | 50 (5.5) | 0.665 |
| Residence (urban) | 85.4 (1.7) | 82.3 (3.9) | 0.3699 | 87.9 (1.8) | 77.3 (5.6) | 0.0116 |
| Metabolic syndrome (yes) | 13.9 (0.9) | 24.4 (3.4) | 0.0002 | 6.2 (0.7) | 12.6 (3.6) | 0.0249 |
| Body mass index ≥ 25 (kg/m2) | 36.5 (1.2) | 44.8 (3.6) | 0.0218 | 16.8 (1.2) | 26.8 (4.8) | 0.0186 |
| Frequency of tooth brushing per day | 0.7367 | 0.0026 | ||||
| ≤ 1 | 9.1 (0.7) | 10.6 (2.4) | 3.3 (0.5) | 5.2 (2.6) | ||
| 2 | 38.2 (1.4) | 39.2 (3.8) | 27.9 (1.3) | 44.5 (5.8) | ||
| ≥3 | 52.7 (1.4) | 50.2 (3.5) | 68.8 (1.3) | 50.3 (5.8) | ||
| Dental checkup within a year (yes) | 23.0 (1.2) | 23.7 (3.1) | 0.8283 | 29.8 (1.3) | 31.6 (5.3) | 0.7293 |
| Self-reported oral status | <0.0001 | 0.0002 | ||||
| Favorable | 16.8 (1.1) | 7.3 (1.8) | 12.4 (1.0) | 4.0 (2.2) | ||
| Average | 44.5 (1.4) | 37.2 (3.8) | 47.5 (1.6) | 34.8 (4.8) | ||
| Problematic | 38.7 (1.4) | 55.4 (3.7) | 40.1 (1.6) | 61.2 (5.0) | ||
Table 1: Baseline characteristics of study participants according to presence of periodontitis.
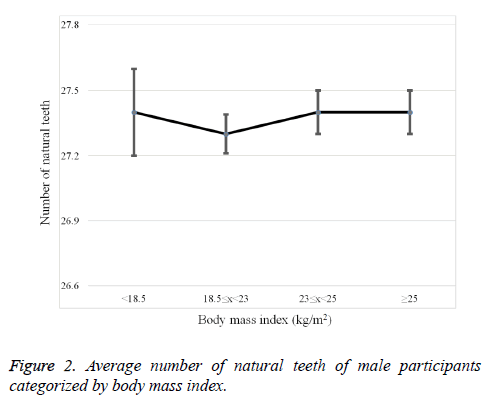
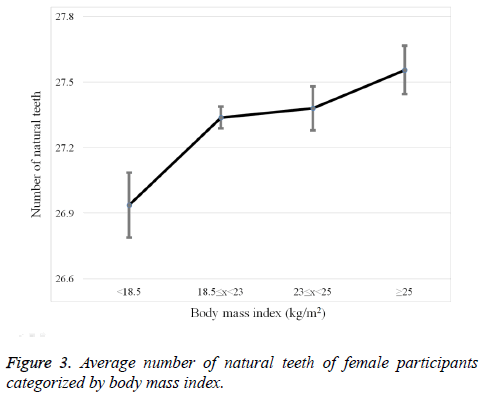
Percentage of participants with smoking was significantly higher in men with periodontitis (P<0.05). Percentage of participants with regular walking was significantly lower in men with periodontitis (P<0.05). Percentage of participants with lowest quartile income was significantly higher in women with periodontitis (P<0.05). Percentage of participants with metabolic syndrome was significantly higher with presence of periodontitis both in men and women (P<0.05). Percentage of individuals with body mass index 25 kg/m2 or greater was significantly higher with the presence of periodontitis both in men and women (P<0.05). Favorable self-reported oral status was significantly lower with the presence of periodontitis both in men and women (P<0.05). Average number of natural teeth defined by body mass index in men and women is shown in Figures 2 and 3, respectively.
Table 2 shows the association between body mass index and smoking, drinking, and periodontitis categorized by sex. Percentage of individuals with current smoking, categorized by body mass index, differed significantly between the groups both in men and women (P<0.05). Percentage of individuals with heavy drinking, categorized by body mass index, differed significantly between the groups both in men and women (P<0.05). Percentage of individuals with periodontitis, categorized by body mass index, differed significantly between the groups only in women (P<0.05).
| Body mass index (kg/m2) | |||||
|---|---|---|---|---|---|
| <18.5 | ≥ 18.5 and <23 | ≥ 23 and <25 | ≥ 25 | P-value | |
| Male | |||||
| Smoking (current) | 49.1 (6.9) | 38.4 (2.1) | 39.3 (2.8) | 46.7 (2.0) | 0.0159 |
| Heavy drinker (>30g/day) | 6.4 (3.6) | 12.8 (1.3) | 15.0 (2.0) | 17.9 (1.5) | 0.0260 |
| Periodontitis (yes) | 5.5 (3.2) | 8.5 (1.1) | 10.2 (1.6) | 12.2 (1.3) | 0.1078 |
| Female | |||||
| Smoking (current) | 11.7 (2.9) | 5.8 (0.9) | 7.3 (2.1) | 10.5 (2.3) | 0.0342 |
| Heavy drinker (>30g/day) | 5.1 (2.2) | 3.5 (0.7) | 3.8 (1.5) | 7.7 (1.9) | 0.0867 |
| Periodontitis (yes) | 5.1 (1.5) | 4.4 (0.7) | 7.9 (2.2) | 8.9 (1.8) | 0.0456 |
Table 2: Distribution of body mass index and smoking, drinking, and periodontitis categorized by sex.
The adjusted odds ratios and 95% confidence intervals of individuals with periodontitis categorized by body mass index in multivariate logistic regression models is shown in Table 3. Adjusted odds ratios and their 95% confidence intervals for periodontitis in men is 0.614 (0.126-2.987), 1 (reference), 1.103 (0.668-1.821), and 1.300 (0.726-2.328), for body mass index of <18.5, 18.5 ≤ x<23, 23 ≤ x<25, and ≥ 25 kg/m2, respectively, after adjustment for age, frequency of tooth brushing per day, self-reported oral status, waist circumference, white blood cell count, smoking, drinking, and walking. Adjusted odds ratios and their 95% confidence intervals for periodontitis in women was 2.400 (1.028-5.605), 1 (reference), 1.152 (0.594-2.235), and 0.971 (0.416-2.268), respectively, after adjustment for body mass index of <18.5, 18.5 ≤ x<23, 23 ≤ x<25, and ≥ 25 kg/m2.
| Periodontitis | |||
|---|---|---|---|
| Body mass index (kg/m2) | Model 1 | Model 2 | Model 3 |
| Male | |||
| <18.5 | 0.912 (0.255-3.268) | 0.639 (0.133-3.081) | 0.614 (0.126-2.987) |
| ≥ 18.5 and <23 | 1 (reference) | 1 (reference) | 1 (reference) |
| ≥ 23 and <25 | 1.013 (0.649-1.583) | 1.124 (0.686-1.841) | 1.103 (0.668-1.821) |
| ≥25 | 1.169 (0.826-1.653) | 1.286 (0.716-2.308) | 1.300 (0.726-2.328) |
| Female | |||
| <18.5 | 1.722 (0.826-3.589) | 2.357 (1.016-5.467) | 2.400 (1.028-5.605) |
| ≥ 18.5 and <23 | 1 (reference) | 1 (reference) | 1 (reference) |
| ≥ 23 and <25 | 1.534 (0.797-2.953) | 1.214 (0.618-2.382) | 1.152 (0.594-2.235) |
| ≥ 25 | 1.897 (1.088-3.308) | 1.006 (0.433-2.334) | 0.971 (0.416-2.268) |
| Model 1: Age adjusted Model 2: Model 1 + frequency of tooth brushing per day, self-reported oral status, waist circumference, and white blood cell count adjusted Model 3: Model 2 + smoking, drinking, and walking |
|||
Table 3: Adjusted odds ratios and 95% confidence intervals of individuals with periodontitis categorized by body mass index in multivariate logistic regression models.
Discussion
This study aimed to identify associations between underweight, determined by body mass index, and periodontal disease using nationally representative data. This study clearly showed that the females with body mass index lower than 18.5 had higher odds ratios of periodontitis.
To date, obesity has been considered a risk factor for health issues [11]. A previous report has shown that individuals with underweight, defined by body mass index, have a significantly increased risk of postsurgical complication compared to individuals with normal body mass index [12]. However, the association and the underlying mechanism between underweight and periodontal disease is not well known yet. Individuals with underweight may have a higher chance of inadequate consumption of food, and this may lead to malnutrition [13]. Underweight persons may have deficiency in essential amino acids and important vitamins [14]. Systemic inflammation has been suggested as being associated with malnutrition, and it has been shown that nutritional status is related to infection [15]. Similar to the association between underweight and systemic diseases, underweight may be served as a risk factor for periodontitis [16]. This study clearly showed the gender-specific association between underweight and periodontitis. It was shown that more than half of the females referred their ideal figure to be underweight and more females were underweight than males [17]. It was demonstrated that females tended to perceive themselves as overweight when they were not, failed to see themselves as underweight when they were underweight [18]. In a previous report, females diet more frequently and used laxatives as their weight-loss strategies and these may have affected the association [17].
The measurement of underweight and obesity may be evaluated by means of various methods including body mass index, waist circumference, waist to hip ratio, relative weight, percentage of body fat, and computed tomography [19]. This study used body mass index, which is considered one of the most commonly used ways to estimate whether a person is overweight and obese. It is used widely to measure population prevalence [20]. However, it should be noted that body mass index is also a widely criticized index [21]. A previous report has suggested that waist circumference may predict a greater variance in health risk than body mass index, and it was shown that obesity-related health risk could be explained by waist circumference and not by body mass index [22]. Previous reports identified the correlation between waist circumference, waist to hip ratio, and body mass index with cardiovascular disease risk, and it was shown that waist to hip ratio showed the strongest correlations [23]. Body fat percentage is calculated by the total mass of fat divided by total body mass, and body fat percentage may serve as better tool for determination of an individual’s health [24]. There may be differences between ethnic groups, and a previous study has shown that this may be due to differences in body build and energy balance [24]. Collectively, it cannot be concluded that one method serves all purposes. However, body mass index can be measured simply and inexpensively, and it can also be considered a useful and clinically important indicator for a large group of people [21].
This study can be considered as offering very well-organized and reliable data. First, data was collected by applying a rolling sampling design involving complex, stratified, and multistage probability samples [25]. Moreover, the interview and survey, along with periodontal examination, were performed by trained experts [26]. However, it should also be noted that the study is characterized by several limitations. The design of the study is cross-sectional, and the cause and effect relationship cannot be verified [27]. Some of the values, including smoking, drinking, exercise, and tooth brushing were obtained by interview, and there may be recall bias [28].
Conclusion
Conclusively, the association between underweight, defined by body mass index, and periodontitis was proven among Korean female adults by multiple logistic regression analyses after adjusting for confounding factors.
Acknowledgement
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, Information and Communication Technology & Future Planning (2017R1A1A1A05001307).
References
- Vasilic-Brasnjevic S, Marinkovic J, Vlajinac H, Vasiljevic N, Jakovljevic B, Nikic M, Maksimovic M. Association of body mass index and waist circumference with severity of knee osteoarthritis. Acta Reumatol Port 2016; 41: 226-231.
- Chen L, Kuang J, Pei JH, Chen HM, Chen Z, Li ZW. Predictors of cardiorespiratory fitness in female and male adults with different body mass index: National Health and Nutrition Examination Survey 1999-2004 Dataset. Ann Med 2016: 1-38.
- Segar AH, Urban JP, Fairbank JC, Judge A. The Association Between Body Mass Index (BMI) and Back or Leg Pain in Patients With Spinal Conditions: Results from the Genodisc Study. Spine (Phila Pa 1976) 2016; 41: E1237-E1243.
- Kim YS1, Kim JH. Body mass index and oral health status in Korean adults: the Fifth Korea National Health and Nutrition Examination Survey. Int J Dent Hyg 2016; .
- Maciel SD, Feres M, Goncalves TE, Zimmermann GS, da Silva HD, Figueiredo LC, et al. Does obesity influence the subgingival microbiota composition in periodontal health and disease? J Clin Periodontol 2016.
- Suresh S, Mahendra J, Singh G, Pradeep AR, Sundaravikram, Sekar H. Comparative Analysis of GCF Resistin Levels in Obese Subjects with and without Periodontal Disease. J Clin Diagnost Res JCDR 2016; 10: Zc71-74.
- Agarwal DP. Cardioprotective effects of light-moderate consumption of alcohol: a review of putative mechanisms. Alcohol Alcoholism (Oxford, Oxfordshire) 2002; 37: 409-415.
- Nam GE, Cho KH, Park YG, Han KD, Choi YS, Kim SM. Socioeconomic status and dyslipidemia in Korean adults: the 2008-2010 Korea National Health and Nutrition Examination Survey. Prev Med 2013; 57: 304-309.
- Chun YH, Kim HR, Han K, Park YG, Song HJ, Na KS. Total cholesterol and lipoprotein composition are associated with dry eye disease in Korean women. Lipids Health Dis 2013; 12: 84.
- Park JB, Han K, Park YG, Ko Y. Association between alcohol consumption and periodontal disease: the 2008 to 2010 Korea National Health and Nutrition Examination Survey. J Periodontol 2014; 85: 1521-1528.
- Jiang SZ, Lu W, Zong XF, Ruan HY, Liu Y. Obesity and hypertension. Exp Ther Med 2016; 12: 2395-2399.
- Alizadeh RF, Moghadamyeghaneh Z, Whealon MD, Hanna MH, Mills SD, Pigazzi A, et al. Body Mass Index Significantly Impacts Outcomes of Colorectal Surgery. Am Surg 2016; 82: 930-935.
- Barreto SM, Passos VM, Lima-Costa MF. Obesity and underweight among Brazilian elderly: the Bambui Health and Aging Study. Cadernos de saude publica 2003; 19: 605-612.
- Deutz NE, Bauer JM, Barazzoni R, Biolo G, Boirie Y, Bosy-Westphal A, et al. Protein intake and exercise for optimal muscle function with aging: recommendations from the ESPEN Expert Group. Clin Nutr 2014; 33: 929-936.
- DeBoer MD, Scharf RJ, Leite AM, Ferrer A, Havt A, Pinkerton R, et al. Systemic inflammation, growth factors, and linear growth in the setting of infection and malnutrition. Nutrition (Burbank, Los Angeles County, Calif) 2016.
- Girsen AI, Mayo JA, Carmichael SL, Phibbs CS, Shachar BZ, Stevenson DK, Lyell DJ, Shaw GM, Gould JB; March of Dimes Prematurity Research Center at Stanford University School of Medicine. Women's prepregnancy underweight as a risk factor for preterm birth: a retrospective study. BJOG 2016; 123: 2001-2007.
- Kuan PX, Ho HL, Shuhaili MS, Siti AA, Gudum HR. Gender differences in body mass index, body weight perception and weight loss strategies among undergraduates in Universiti Malaysia Sarawak. Malaysian J Nutrition 2011; 17: 67-75.
- Connor-Greene PA. Gender differences in body weight perception and weight-loss strategies of college students. Women Health 1988; 14: 27-42.
- Bray GA. Definition, measurement, and classification of the syndromes of obesity. Int J Obes 1978; 2: 99-112.
- Gurunathan U, Myles PS. Limitations of body mass index as an obesity measure of perioperative risk. Br J Anaesth 2016; 116: 319-321.
- Ortega FB, Sui X, Lavie CJ, Blair SN. Body Mass Index, the Most Widely Used But Also Widely Criticized Index: Would a Criterion Standard Measure of Total Body Fat Be a Better Predictor of Cardiovascular Disease Mortality? Mayo Clinic Proceed 2016; 91: 443-455.
- Janssen I, Katzmarzyk PT, Ross R. Waist circumference and not body mass index explains obesity-related health risk. Am J Clin Nutrition 2004; 79: 379-384.
- Dalton M, Cameron AJ, Zimmet PZ, Shaw JE, Jolley D, Dunstan DW. Waist circumference, waist-hip ratio and body mass index and their correlation with cardiovascular disease risk factors in Australian adults. J Int Med 2003; 254: 555-563.
- Deurenberg P, Yap M, van Staveren WA. Body mass index and percent body fat: a meta analysis among different ethnic groups. International journal of obesity and related metabolic disorders . J Int Assoc Study Obesity 1998; 22: 1164-1171.
- Han K, Hwang E, Park JB. Association between Consumption of Coffee and the Prevalence of Periodontitis: The 2008-2010 Korea National Health and Nutrition Examination Survey. PloS one 2016; 11: e0158845.
- Han K, Hwang E, Park JB. Excessive Consumption of Green Tea as a Risk Factor for Periodontal Disease among Korean Adults. Nutrients 2016; 8.
- Han K, Ko Y, Park YG, Park JB. Associations Between the Periodontal Disease in Women Before Menopause and Menstrual Cycle Irregularity: The 2010-2012 Korea National Health and Nutrition Examination Survey. Medicine (Baltimore) 2016; 95: e2791.
- Song IS, Han K, Ko Y, Park YG, Ryu JJ, Park JB. Associations between the consumption of carbonated beverages and periodontal disease: The 2008-2010 Korea national health and nutrition examination survey. Medicine 2016; 95: e4253.