Research Article - Current Pediatric Research (2023) Volume 27, Issue 4
Unannounced standardized patients to assess child abuse management.
Rao Chandrika*, Sunil Kumar BM, Venkatesh D, Vijaydas Muradi
Department of Pediatrics, MS Ramaiah Medical College and Hospital, Bangalore, India
- Corresponding Author:
- Rao Chandrika
Department of Pediatrics and Medical Education,
MS Ramaiah Medical College and Hospital,
Bangalore, India
E-mail: docrao2000@yahoo.com
Received: 27 March, 2023, Manuscript No. AAJCP-23-92545; Editor assigned: 29 March, 2023, Pre QC No. AAJCP-23-92545(PQ); Reviewed: 14 April, 2023, QC No. AAJCP-23-92545; Revised: 21 April, 2023, Manuscript No. AAJCP-23-92545(R); Published: 28 April, 2023, DOI:10.35841/0971-9032.27.04.1185-1189.
Abstract
Background: Unannounced Standardized Patients (USP) can contribute to skill learning of medical students to manage child abuse cases. Objective: To compare the forensic interviewing and counseling skills of Post Graduates (PG) during and after exposure to USP encounter. Study design: Interventional study with USP encounter. Participants: Pediatric postgraduates. Intervention: USPs was selected from volunteer students, trained in two abuse case scenarios. Checklist and feedback form was validated USP encounter as a real patient was managed by the PGs under supervision. Focused Group Discussion (FGD) was held. PGs had a second planned encounter with same SPs in Objective Structured Clinical Examination (OSCE) format. Outcomes: Scores of SP encounters, PG feedback, reflections, FGD. Results: The SPs were able to portray themselves as a patient. The USP feedback revealed that postgraduates demonstrated poor listening skills, were distracted, used mobile phone, did not display adequate confidence and empathy and demonstrated fair competency. The PGs performed better in second encounter. Wilcoxin analysis was significant with P-value<0.001 (z-value=-4.0145). Postgraduates felt that SP appeared authentic, cooperated in history, asked relevant questions, and was natural in interactions. The PGs and SPs reflected that USP was an effective tool, which improved their confidence and counseling skills. The FGD revealed themes about their lack of confidence and awkwardness in child abuse cases, necessity of training, personal barriers, and sensitivity of topic. Conclusion: Interviewing and counseling skills of a PG during and after exposure to an unannounced SP encounter improved. SPs could be trained, could assess and provided constructive and objective feedback.
Keywords
Child abuse, Sexual abuse, Child protection, Unannounced standardised patient.
Introduction
Child abuse cases require competent handling, apt communication and empathetic management of the cases. Gaps exist in the management and handling the family and the child. Medical students are not taught, trained or exposed to cases of child abuse. The topic is covered briefly in the present undergraduate curriculum. It does not train the doctors and empower them with confidence enough to manage the cases after graduation. The ability to communicate and counsel is often lacking. There is a need to focus on the training outcomes in this area with added public and media attention in such cases [1,2].
Hypothesis
Hawthorne-like effects wherein awareness that the quality of care is being assessed actually influences the care provided, can also provide strong and convincing evidence that helps motivate sceptical professionals to change system practices.
The present study was undertaken to see if Unannounced Standardized Patient (USP) as teaching intervention improved the management of child abuse cases by postgraduates. The objective was to compare the forensic interviewing and counseling skills of a PG during and after exposure to an unannounced SP encounter.
Methodology
The study was planned by the pediatric and medical education department and conducted in a tertiary care medical college hospital, where cases of child abuse are referred and managed regularly. It was an Interventional study with an unannounced standardized patient encounter. Ethical clearance was obtained from the institutional ethics committee. Sensitization and training program on child abuse management was taken for the postgraduates, 4-12 weeks before the planned encounter.
Postgraduates (Paediatrics) were trained in child abuse history and examination as a routine at the start of the residency. Consent was taken during this training period, from Post graduates for assessment by an Unannounced Standardized Patient (USP) in the following six months. The USP encounter was planned only after all PGs had had a real patient encounter.
USPs was selected from a pool of student volunteers. Age, gender, was the criteria, along with ability to perform the role. We selected and trained four USPs to ensure consistency of the cases in case any one USP leave the study unexpectedly. Standardized patients were recruited who were above 18 years of age and portrayed case characters between 16-18 years trained in each clinical scenario (physical abuse–mother/ grandmother suspected to have caused head injury, sexual abuse 16 year girl alleging abuse) and will be referred to as USPs henceforth. USPs participated in a three day training program with follow-up trainings before meeting the postgraduate. Only the history and management was planned and included.
Examination findings were documented by senior physician and carried in the file and the USPs showed the same to the assessing physician at end of history. The USPs was trained in the case scenario, history questions checklist for assessing PGs, feedback forms and communication skills. Role play, simulation and videos were used to train the SPs. In addition, supervision by faculty was done to provide the USPs with reminders, and individual remediation. A pilot study was done to assess USP feedback after the assessing physician completed the pilot interview and counseling.
The checklist and feedback form was validated after the pilot study. Feedback was given to USPs and the case scenario was finalized. The dress, eye contact, posture and tone of speech were specifically emphasized. Two practice sessions were held after the pilot encounters. After each visit, a faculty reviewed the interview and completed a role consistency form to give the USP feedback on performance, including the USP’s ability to provide accurate information, affect, and believability.
After training, the USPs had an encounter with postgraduates as real patients unannounced in the outpatient department. Faculty observed the interaction with patient (unannounced SP), as is routinely done in child abuse case management in the hospital. USPs submitted their feedback after the encounter to the investigator. PGs submitted their history data sheet, feedback to the investigator as a routine case record. Focused group discussion was held by the investigator and PGs after all the PGs had an encounter. This was completed in 46 days. The feedbacks were discussed. Challenges faced by the PG in handling the case were discussed and resolved. PGs were retrained in management aspects and communication skills.
After training, all PGs had a planned encounter with same USPs in planned format after three months in order for PGs to compare their performance between USP and planned format. Scores of first and second SP encounter were compared. Scores of USP were noted. Feedback from PGs about USP encounter and reflections were collected. Focused group discussion on the whole process was being conducted with all postgraduates. The outcome parameters were patient encounter checklists for SPS, patient`s data collection sheets-filled by PGs, Feedback forms from PG, USP and PG reflection were collected. Focus group discussion was held with all the PGs participating.
Statistical analysis: It was a convenience sampling. 20 pediatric postgraduates were enrolled. Qualitative assessment was done by a focus group discussion involving postgraduates, faculty observers and investigator. The PGs data results and SP feedback was compared with pre and post intervention results. Qualitative analysis was done. Focus Group Discussion (FGD) was thematically analyzed. Reflections by PGs, USPs were collected. Scores of encounters were analyzed by Wilcoxin signed rank test and FGD thematically analyzed and submitted feedback in structured format.
Results
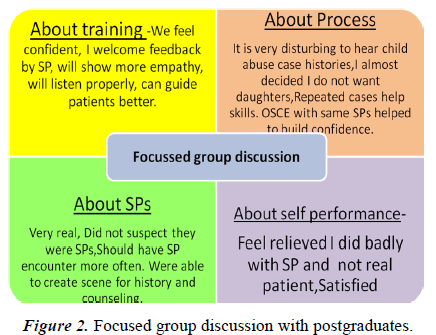
Each PG had one USP encounter. The USPs was able to portray themselves as a patient in the OPD. Their feedback revealed that 25% postgraduate poorly demonstrated skills as listening to their history without distraction, 30% of PGs used mobile phone while taking the history, 25%-30% did not display confidence and empathy to the patient and 60% demonstrated adequate competency in handling a child abuse case (Figure 1). The PGs performed better in second encounter with the USP. Comparison of both encounter scores with Wilcoxin analysis was significant with P-value<0.001 (zvalue=- 4.0145) (Table 1).
| History | 1-Poor | 2-Fair | 3-Good | 4 Very good | 5-Excellent |
|---|---|---|---|---|---|
| How is the doctor at: | n (OSCE) | n(OSCE) | n(OSCE) | n(OSCE) | n(OSCE) |
| Quality of care | |||||
| Greeting you by name | 6 | 2 | 6 (10) | 6 (10) | |
| Letting you tell your case without interruption | 6 | 4 (12) | 8 (8) | 2 | |
| Listening(or distracted) | 4 | 10 | 4 (16) | 2 (4) | |
| Shows interest | 4 | 2 | 6 (10) | 4 (6) | 4 (4) |
| Takes history of following protocol | |||||
| Family demographics | 4 | 2 | 6 | 6 (18) | 2 (2) |
| Incident details | 2 | 0 | 10 (2) | 6 (16) | 2 (2) |
| Displaying empathy | |||||
| Social concerns | 4 | 2 | 10(6) | 4 (14) | |
| Emotional impact | 4 | 12 (4) | 2 (14) | 2 (2) | |
| Support at home | 6 | 6 | 6 | 0 (16) | 2 (4) |
| Communication skills | |||||
| Displayed awkwardness | 6 | 2 | 10 (12) | 2 (8) | |
| Used simple words | 2 | 4 | 10 | 0 (16) | 4 (4) |
| Used open ended questions | 4 | 6 | 10 (4) | 0 (10) | 0 (6) |
| Used sensitive language | 2 | 14 | 2 (18) | 2 (2) | |
| How did the doctor advise-following management protocol | |||||
| Urine test | 10 | 2 | 2 | 6 (20) | |
| Pregnancy test | 10 | 2 | 2 | 6 (20) | |
| HIV, Hep B | 10 | 2 | 2 | 6 (18) | 0 (2) |
| Bone age | 10 | 2 | 2 | 6 (18) | 0 (2) |
| Contraception | 10 | 4 | 2 (4) | 4 ( 16) | |
| Psychological assistance | 12 | 2 | 2 | 4 (18) | 0 (2) |
| Made follow up appointment | 4 | 12 | 2 | 2 (20) | |
| Completed interview and consultation with reassurance | 6 | 4 | 4 | 6 (20) | |
| Wilcoxin analysis: p-value<0.001 (z value=-4.0145) | |||||
| What was done well during Consultation? | Eye contact, communication, history taking | ||||
| State areas which could be improved upon? | Counselling | ||||
| Note:n=number of PGs in Unannounced SP encounter-Brackets-Number of PGs in OSCE | |||||
Table 1. Standardized patient feedback of unannounced SP encounter and OSCE encounter.
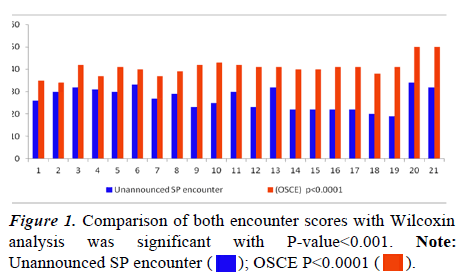
The focus group discussion with the postgraduates revealed themes about their lack of confidence and awkwardness when encountering child abuse cases as compared to medical emergencies, necessity of training in counseling and communication, poor self-performance, improving counseling, personal barriers and fears about topic, sensitivity of topic. 90% of the PGs felt that the USP was realistic and asked relevant questions (Figure 2 and Table 2).
| Complete disagreement | Moderate disagreement | Moderate agreement | Complete agreement | |
|---|---|---|---|---|
| SP appeared authentic as a patient | - | - | 5% | 95% |
| SP is clearly role playing | 90% | 5% | 5% | - |
| SP stays in his/her role all the time | - | 5% | 60% | 35% |
| SP was natural in interactions | - | 5% | 25% | 70% |
| SP cooperated in history | - | - | - | 100% |
| SP asked relevant questions during counseling | 5% | 5% | 10% | 80% |
Table 2. Evaluations of unannounced SP by postgraduates.
Reflection of the PGs and USPs was taken on five aspects, namely: What was most effective, least effective, most disappointing, and difficult for you and has the process changed anything. Responses are reflected in Table 3. They reflected that unannounced SP was an effective tool, which improved their confidence and counseling skills.
| Reflections | SP | PG |
|---|---|---|
| What was most effective? | Unannounced, | Unannounced, |
| Standardized Patient | Standardized patient | |
| What was least effective? | Counseling, | Counseling, |
| Confidence | Investigations, | |
| Confidence, Privacy inadequate. | ||
| What was disappointing? | When doctors did not pay complete attention, | Did not counsel, |
| Did not counsel. | In my communication | |
| What was difficult for you? | Child abuse | Confidence, |
| Not to be distracted, | ||
| To be careful in a medico legal case. | ||
| Has the process changed anything? | The doctor was trained, More empathy for victim | Training, |
| Confidence, | ||
| Now more comfortable with child abuse cases. Approach to case can be improved. | ||
| Training important for management of Child abuse cases. |
Table 3. Reflections of postgraduates and standardized patient.
Discussion
Management of a patient with alleged abuse and the family in a competent and empathetic manner is important. The doctors require competency in cognitive, psychomotor and affective domains in dealing with child abuse cases specifically. Actual observation by senior doctors is a definite way of ensuring competency [1]. Feasibility is however a constraint. The postgraduates do encounter cases and handle it in their professional capacity. However they may not have been guided completely in the skills and nuances of interview, evidence collection and counseling of management of a case of child abuse [2]. The training in undergraduate medical education is an apt timing to enforce child protection behavior [3].
The SP approach has been referred to as the ‘gold standard’ for capturing actual provider behavior in the healthcare setting. Many unpredictable communications may occur which are rare and difficult to capture [4]. The parent or the child may disclose the reason for the visit in midst of the visit which may then miss assessment by the senior. Communication studies, hence find it difficult to capture real time communications between patients and their physicians.
Unannounced SP methodology is ideal to capture such communication behavior, [5] though challenges exist. USPs can capture aspects of the history taking and examination that are important to clinical care and difficult to gather with other methodologies. USPs can provide feedback into the patient`s from the very start (walking in the front door) to the end (walking out the front door) and therefore all the health system parameters that may affect quality of care, patient safety, and patient outcomes can be observed [5-7].
In this study, we employed Unannounced Standardized Patients (USPs) to directly observe physician behaviors at managing alleged child abuse cases. The unique aspect of USP is the different perspective on the functioning of health care systems because they combine a number of methodological strengths: 1) They avoid the "Hawthorne effect" by capturing the practices of health care professionals when they are not aware of being assessed; 2) They involve a highly trained observer/ assessor (the USP); 3) They focus on the vantage point of the patient; 4) They control not only for the influence of patient characteristics on recall and evaluation of care through the use of a trained person, and they are standardized in terms of the clinical features of the case, demeanour and personality of the patient [8].
A major ethical concern surrounding SPs is the deception of healthcare providers and whether or not informed consent should be sought from them. Studies have shown that seeking informed consent from doctor can alter the scientific validity of the study by influencing the decision of providers to take part (creating selection bias) or influencing their behavior (Hawthorne effect) if they think SP visits are imminent [9].
It is possible that informing residents that USPs would be visiting them in the ED improved performance. Zabar, et al. in their study have said that the majority of residents did not feel that the possibility of encountering a USP had any negative impact on their daily practice [10]. Likely obstacles include concerns about the ethics of sending health professionals incorrect portrayal as patients, the technical challenges of the confidential visit, and concerns about the relatively small sample sizes and substantial costs which may be present to train SPs [11].
Using Standardised Patients (SP) for child abuse management is challenging. Use of children as SPs (less than 18 years) has been questioned with regard to ethics. The use of young SPs should be avoided as far as possible and limited only to situations and assessments that cannot be satisfactorily be measured by any other assessment [12,13]. Identity of the USP, training the USPs and creating their identities and analyzing the resultant data should be confidential. The limitations of our study are that it is a small sample size, but has been able to captures the issues in history taking and treating the patient.
The strengths are USPs provide a penetrating assessment of clinician performance because they assess actual clinician behaviors rather than what is recorded in the medical record. They enable feedback which is personal that postgraduates can utilize to improve their care and potentially enhance valuebased care [14,15]. Management of child abuse needs training in cognitive and affective domain skills. The requisite theory and clinical skills needed to manage Clinical Sexual Abuse (CSA) should be included in the medical curriculum. Demonstration of basic interview techniques in history taking should be conducted using role-plays along with video demonstrations of correct interviewing methods.
Hybrid curriculums are useful in training the students to suspect and identify probable child abuse, deal with the medico legal concerns with the families, network with the legal authorities and investigating agencies, facilitate a physical and psychological trauma impact assessment [16]. Problem based learning, reflective writing, role plays, videos can be used with traditional teaching. Postgraduate students and faculty should attend Continuing Medical Education (CME) courses, symposiums. This would help them in being confident in the OPD, identify their deficiencies. Structured interview proforma with diagrams can be used [17].
Conclusion
Unannounced Standard Patient (USP) program is a promising method for assessing the functioning of the clinical care system within a health care system. Interviewing and counselling skills of PG during and after exposure to an unannounced SP encounter improved. SPs could assess PGs, provided constructive and objective feedback. The conventional medical curriculum in India needs more focus on explicit teaching and assessment of interpersonal and communication skills, professionalism, team-work and reflection with appropriate teaching learning methodology.
References
- Whitcomb ME. Competency-based graduate medical education? Of course! But how should competency be assessed? Acad Med 2002; 77(5): 359-60.
- Giardino AP, Brayden RM, Sugarman JM. Residency training in child sexual abuse evaluation. Child Abuse Negl 1998; 22(4): 331-6.
- Kumar A, Chandran S, Rao K, et al. The need for training medical professionals in child sexual abuse. J Psychosexual Health 2019; 1(2): 192-194.
- Omo NA. Working with emotionally and sexual abused children: The therapeutic value of effective communication. Int J Res Arts Soc Sci 2015; 8(1): 151-161.
- Siminoff LA, Rogers HL, Waller AC, et al. The advantages and challenges of unannounced standardized patient methodology to assess healthcare communication. Patient Educ Couns 2011; 82(3): 318-24.
- Wiseman V, Lagarde M, Kovacs R, et al. Using unannounced standardised patients to obtain data on quality of care in low-income and middle-income countries: Key challenges and opportunities. BMJ Global Health 2019; 4: e001908.
- Weiner SJ, Schwartz A. Directly observed care: Can unannounced standardized patients address a gap in performance measurement? J Gen Intern Med 2014; 29: 1183–1187
- Zabar S, Hanley K, Stevens D, et al. Unannounced standardized patients: A promising method of assessing patient-centered care in your health care system. BMC Health Serv Res 2014; 14: 157.
- Krane NK, Anderson D, Lazarus CJ, et al. Physician practice behavior and practice guidelines: Using unannounced standardized patients to gather data. J Gen Intern Med 2009; 24: 53–6.
- Zabar S, Tavinder Ark MS, Colleen G, et al. Can unannounced standardized patients assess professionalism and communication skills in the emergency department? Acad Emerg Med 2009; 16(9): 915-918.
- Tsai TC. Using children as standardised patients for assessing clinical competence in paediatrics. Arch Dis Child 2004; 89(12): 1117-20.
- Plaksin J, Nicholson J, Kundrod S, et al. The benefits and risks of being a standardized patient: A narrative review of the literature. Patient 2016; 9(1): 15-25.
- Schwartz A, Peskin S, Spiro A, et al. Impact of unannounced standardized patient audit and feedback on care, documentation, and costs: An experiment and claims analysis. J Gen Intern Med 2021; 36: 27–34.
- Jan-Joost R, Simone G, Lonneke B, et al. Unannounced standardised patients in real practice: A systematic literature review. Med Educ 2007; 41(6): 537-49.
- Ivanoff CS, Hottel TL. Comprehensive training in suspected child abuse and neglect for dental students: A hybrid curriculum. J Dent Educ 2013; 77(6): 695-705.
- Botash A, Galloway A, Booth T, et al. Continuing medical education in child sexual abuse. Arch Pediatr Adolesc Med 2005; 159(6): 561.
- Kapoor A, Kapoor A, Badyal DK. Simulated patients for competency-based undergraduate medical education post COVID-19: A new normal in India. Indian Pediatr. 2021; 58(9): 881-887.
 OSCE P<0.0001
OSCE P<0.0001 .
.