Research Article - Biomedical Research (2017) Volume 28, Issue 3
Two-year follow-up of closed reduction and external fixation treatment of unstable fractures at the base of the first metacarpal
Zhang Y*, Xu N, Gu W and Jiang SDepartment of Orthopaedics, Changzhou No.2 People's Hospital Affiliated to Nanjing Medical University, China
- *Corresponding Author:
- Zhang Y
Department of Orthopaedics
Changzhou No.2 People's Hospital affiliated to Nanjing Medical University, China
Accepted date: September 12, 2016
Abstract
This retrospective analysis investigated the clinical effect of closed reduction and external fixation on unstable fractures at the base of the first metacarpal. A total of 23 patients with unstable fractures at the base of the first metacarpal were treated, including six with Bennett fractures, three with Rolando fractures, six with extra-articular transverse fractures, and eight with extra-articular oblique fractures. If closed reduction by all fracture manual reset techniques was satisfactory, external fixation was used. Postoperative fracture healing was assessed by X-ray imaging. In the 24-month follow-up period, functional recovery was assessed by, Disability of the Arm, Shoulder, and Hand (DASH), total active motion test of the thumb, Jamar dynamometer thumb muscle testing. The fracture healing time was 8-12 weeks. Nineteen cases were followed up for up to 24 months (82.6%). The average DASH score was 3.4 ± 0.8. The total active motion loss of the thumb was 7.5 ± 1.3°. The thumb grip strength of the affected side on Jamar dynamometer testing was 65.5-113% of the uninjured side, while the pinch strength of the affected side was 66.6-104.5% of the uninjured side. Patients with unstable fractures at the base of the first metacarpal treated with closed reduction and external fixation underwent 2 years of follow-up, which revealed good functional thumb recovery.
Keywords
Unstable fracture, Closed reduction, External fixation.
Introduction
The base of the first metacarpal and trapezium constitutes the thumb carpometacarpal joint, an important anatomical structure that enables complete complex thumb activities. When the thumb endures axial force, damage can be transmitted to the epiphysis along the first metacarpal, resulting in fracture of the base of the first metacarpal bone. Malreduction at the base of the first metacarpal fracture leads to malunion and traumatic arthritis, particularly affecting thumb opposition [1]. Since conservative treatment makes it difficult to achieve accurate setting of the articular surface and maintain the metacarpal length, it is widely accepted that surgery should be chosen as treatment of an unstable fracture at the base of the first metacarpal, but the choice of surgical approach has not gained consensus [2,3]. Closed reduction and percutaneous Kirschner wire fixation have been widely used and shown to have high efficacy in long-term follow-up [4]. The fixation effect of open reduction using pins or screws is more reliable [5]. However, in most of these methods, the fixture penetrates the articular cartilage surface to increase cartilage damage, which creates the potential risk of traumatic arthritis. Open reduction by plates and screws has the same satisfactory results [6] but also involves disadvantages such as higher cost and the need for a second surgery to remove the internal fixation. After closed reduction, fixation of the first and the second metacarpal bones indirectly fixes the fractures, which can effectively maintain the metacarpal length, but limits the activities of the second metacarpal and reduces the first web space [7,8]. Therefore, closed reduction and external fixation is a minimally invasive and effective treatment for fractures at the base of the first metacarpal that can achieve a better stabilizing effect than that of Kirschner wire internal fixation [9], which has been widely reported in clinical studies [10-13], but long-term follow-up studies are lacking. From 2008 to 2013, 23 cases of unstable fracture at the base of the first metacarpal were subjected to external fixation after closed reduction, radiological evaluation, and clinical observation for 2 years after surgery.
Materials and Methods
Clinical data
Patients with unstable fracture at the base of the first metacarpal treated at our hospital with closed reduction and external fixation between January 2008 and January 2013 were retrospectively analyzed. A total of 23 patients (16 men and seven women) with a mean age of 43.8 years (range, 19-71 years) were enrolled. This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Nanjing Medical University. Written informed consent was obtained from all participants.
The causes of injury included 10 cases of motorcycle traffic accident, 10 cases of falls, and three cases of hits. The treatment time after injury was 0.5-24 hours.
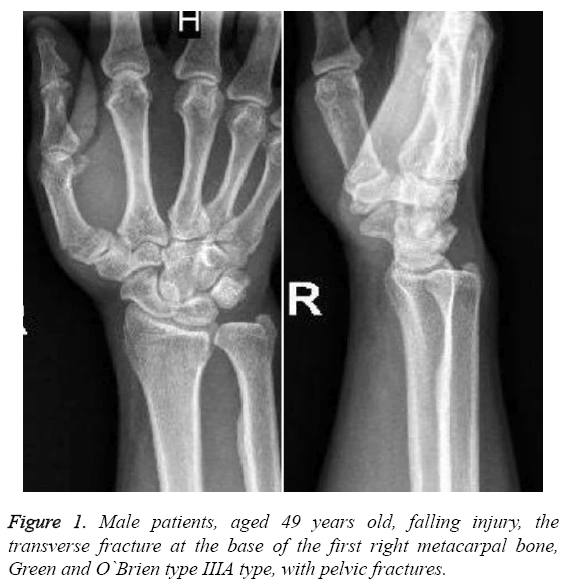
Clinical manifestations included thumb pain and swelling. Physical examination showed deformity, tenderness, and bone friction sensitivity at the base of the first metacarpal, and restricted thumb flexion and extension activities. All cases had closed fractures, but two also had partial abrasion bleeding. Xray examinations showed fractures at the base of the first metacarpal. In accordance with the classification criteria of Green and O’Brien in 1972, there were six cases of type I fracture (Bennett fracture), three cases of type II fracture (Rolando fracture), six cases of type IIIA fracture (extraarticular transverse fracture), and eight cases of type IIIB fracture (extra-articular oblique fracture). All patients were subjected to manual reduction in outpatient service, but the reset could not be maintained due to significant fracture displacement. Of all patients, one had a double fracture of the right radius and ulna, one had a combined pelvic fracture, and two had combined distal radial fractures. The surgery was performed 2-7 days after the injury and finished by the same group of physicians (Table 1).
| Number | Gender | Age | Injury causes | Fracture type | Combined injury |
|---|---|---|---|---|---|
| 1 | Male | 68 | Falling | I | |
| 2 | Male | 63 | Falling | II Y | Distal radius fractures |
| 3 | Male | 26 | Hit | III A | |
| 4 | Female | 24 | Traffic | I | |
| 5 | Male | 28 | Falling | III A | |
| 6 | Male | 19 | Traffic | III B | Fracture of ulna and radius |
| 7 | Male | 58 | Traffic | I | |
| 8 | Female | 33 | Falling | III B | |
| 9 | Female | 61 | Traffic | II T | |
| 10 | Male | 26 | Falling | III B | |
| 11 | Male | 27 | Traffic | I | |
| 12 | Female | 38 | Falling | III B | |
| 13 | Male | 35 | Traffic | I | |
| 14 | Male | 57 | Falling | III A | Pelvic fracture |
| 15 | Male | 43 | Falling | III B | |
| 16 | Female | 49 | Traffic | III B | |
| 17 | Female | 63 | Falling | I | |
| 18 | Male | 39 | Traffic | III B | |
| 19 | Male | 71 | Hit | III A | |
| 20 | Male | 38 | Falling | III A | |
| 21 | Male | 45 | Hit | III B | |
| 22 | Male | 37 | Traffic | II T | |
| 23 | Female | 59 | Traffic | III A | Distal radius fractures |
Table 1: Patients’ basic information
Treatment methods
Patients were positioned supine and anesthetized by a brachial plexus block. The upper limb was outreached and placed on a hand surgery operating table. A bar tourniquet was tied on the proximal upper arm and inflated to a pressure of 40 Kpa. Conventional povidone-iodine disinfection was used for the operative field, and a sterile towel and C-arm were placed.
Closed reduction techniques
Under X-ray perspective of the C-arm, the manual reset technique was used first. (1) In Rolando fracture reduction, the first metacarpal bone can be subjected to internal rotation, axial traction, and outreaching dorsiflexion to the first metacarpophalangeal joints to shorten the angular deformity and restore the force lines of the first metacarpal bone (2). For transverse and oblique fractures outside the joints, the surgeons turned the top over in traction by the thumb to correct the angular deformity (3). The Bennett fracture used “screw home” reset, that is, tensing of the dorsal ligaments of the first carpometacarpal joint to achieve indirect reduction. During surgery, the surgeons placed the patient’s thumb in the passive opposition position and tried to internally rotate the first metacarpal to position the thumb mound opposite to the index and middle finger mounds. The dorsal ligament was placed under tension to help reset the ulnar displacement bone of the Bennett fracture. The reduction quality was confirmed by Xray. Surgeons must ensure that the articular surface is smooth and avoid articular surface displacement >2 mm.
External fixation bracket type selection
Combined unilateral external fixators provided by the Beijing External Fixation Institute consisted of threaded half needles, clamps, connecting pieces, and other components. All items were made of medical-grade stainless steel.
After successful resetting confirmed by X-ray, traction was continued to maintain the reset state. After pre-drilling by a 2.5 mm diameter Kirschner wire, the screws were screwed into a threaded 2.5 mm diameter half needle perpendicular to the longitudinal axis of the first metacarpal. Surgeons should avoid making the two threaded half needles parallel; rather, the proximal threaded half needle should be as close to the fracture line as possible and the two threaded half needles should be kept as far apart as possible. In the same way, after pre-drilling with the 2.5 mm diameter Kirschner wire is performed, two threaded 2.5 mm diameter half needles were screwed crosswise into the centre of the trapezium at an angle of approximately 60˚C. For extra-articular transverse fractures, if the proximal end of the first metacarpal bone was of sufficient length, the two threaded half needles could be placed at the base of the first metacarpal bone. When the threaded half needles are placed, the surgeon should carefully avoid the extensor pollicis longus muscle tendon. Perspective was carried out to determine the satisfaction of needle position, both the length penetrated the cortex to connecting pieces in order to fix and lock the threaded half needles, connect the components. We moved the thumb, assessed the stability of fracture fixation again in perspective.
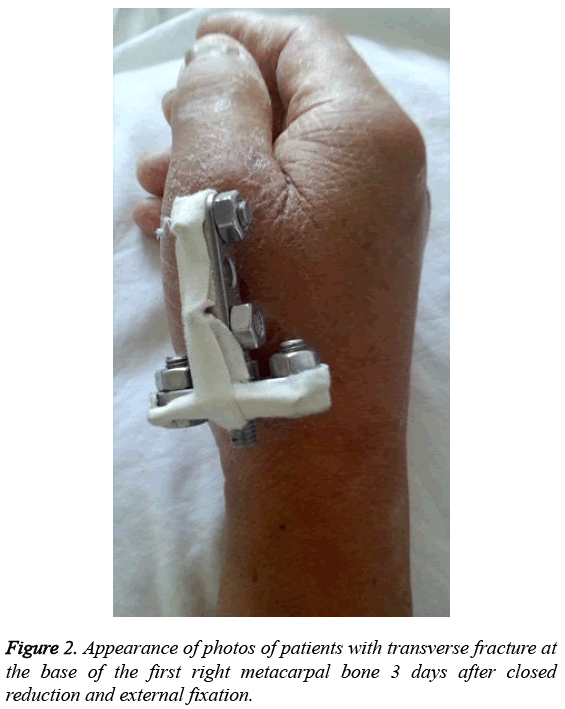
Postoperative treatment
None of the patients required plaster casting after surgery, and the needle tract was disinfected daily by 75% alcohol. The external fixation was removed when the X-ray showed continuous callus through the fracture line. After bracket removal, patients were gradually allowed to hold heavy objects and exercise.
Imaging evaluation
One month after surgery, radiographs of the hand were taken in the anteroposterior and oblique view every 2 weeks to assess fracture healing. Once the external fixation on X-ray images showed continuous callus through the fracture line, we took Xray images every month until the fracture line disappeared and the fracture completely healed. After 24 months, images were taken to assess the extent of traumatic arthritis. Arthritis was classified according to the Eaton-Littler classification criteria modified by van Niekerk and Owens as follows: class 1, no clear changes in arthritis; class 2, osteophytes <2 mm; class 3, osteophytes >2 mm or showed joint space narrowing; and class 4:partial or total disappearance of the joint space.
Clinical evaluation
In the 24-month follow-up period, questionnaires were used to assess each patient’s thumb function. The main included contents were as follows. (1) Joint function was assessed according to the Disability of the Arm, Shoulder and Hand (DASH) scale of 0-100 points in which a higher score indicated a greater loss of functionality. (2) The Total Active Motion (TAM) between the uninjured and affected side of the thumb was compared. For the thumb, the total active activity was equal to the flexion sum of the thumb carpometacarpal joint, metacarpophalangeal joints, and interphalangeal joint subtracted from the extension sum of the carpometacarpal joint, metacarpophalangeal joints, and interphalangeal joint. Compared with the uninjured side, the TAM of the affected side did not become better: 76-99% maintenance was taken as good, 50-75% as moderate, and <50% as poor. (3) The Jamar grip dynamometer was used to evaluate the thumb muscle force of the uninjured and affected sides of the thumb, including grip and pinch strength [14]. The calculated percentage of the muscle strength of the affected side was compared to that of the uninjured side.
Statistical analysis
The SPSS version 14.0 statistical package was used for the statistical analysis. Quantitative normally distributed data are expressed as ± s. Non-normally distributed data were analyzed by the non-parametric Mann-Whitney test method to compare the function of the uninjured and the affected sides. Significance was indicated at α=0.05.
Results
Patients attended follow-up appointments once every 2 weeks starting at 1 month after surgery until the fracture healed completely. Four patients were lost when the follow-up lasted for 6 months after surgery, whereas the other 19 patients (82.6%) completed the entire 24-month follow-up period.
The mean intraoperative time was 43.85 minutes (range, 20-62 minutes). The operative times of three cases of multiple fractures that were simultaneously subjected to multi-site surgery were not included in the statistics. Analysis of variance showed that surgery duration and fracture type did not differ among patients (P>0.05).
Three patients had swelling and exudate in the needle tract within about a week, including one case with primary skin abrasions. The exudate decreased after local cleaning and dressing and the administration of oral antibiotics. The needle tracts of all patients healed after external fixator removal.
Imaging evaluation
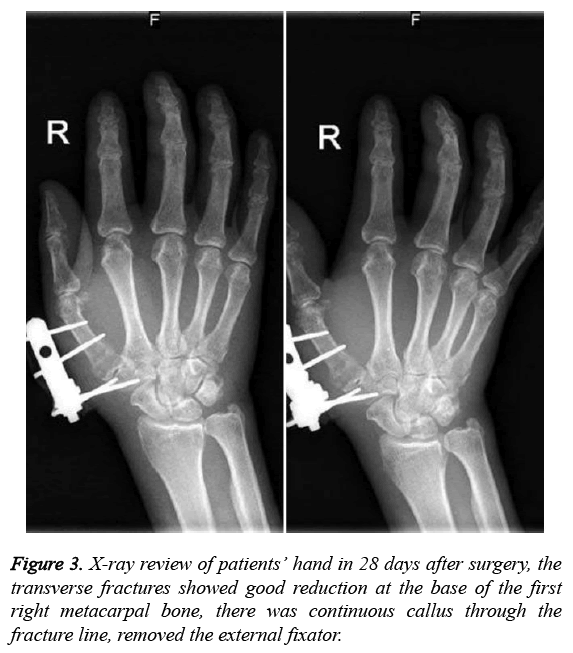
Approximately 1 month after surgery, X-ray of the 23 patients showed no fracture displacement and no loose or pulled-out threaded half needles. There were 18 cases of well-growing callus and a blurred fracture line, and the external fixator was removed.
Callus growth of five cases was unsatisfactory; of them, the bracket removal in four was extended to about 6 weeks, while that of an elderly patient was extended to 2 months when the images showed callus growth after surgery. Mean external fixation removal was 33.39 days (range, 27-60 days). The 3- month review radiography revealed fracture healing in all patients. Mean fracture healing time was 10 weeks (range, 8-12 weeks) (Figures 1-3).
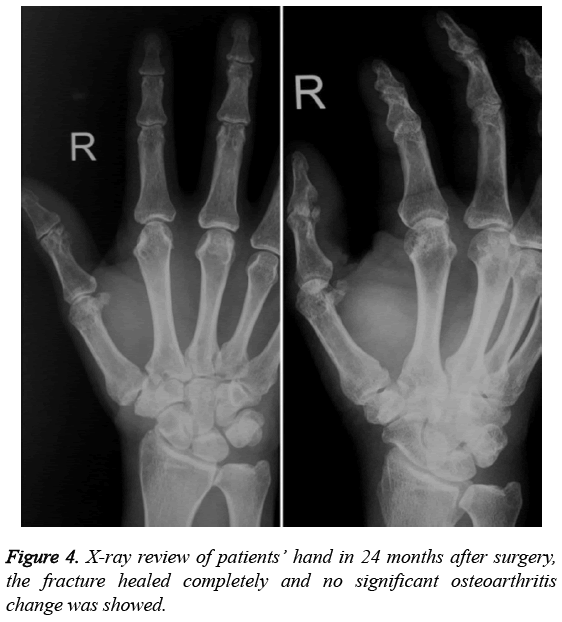
X-rays of the 24-month follow-up showed that carpometacarpal joints of one case with Bennett fracture and two cases with Rolando fracture had osteophytes <2 mm with Eaton-Littler class 2. The remaining patients had no significant osteoarthritis change with Eaton-Littler class 1 (Figure 4).
Clinical evaluation
The 24-month investigation questionnaire after surgery showed that the average DASH score was 3.4 ± 0.8, indicating that the patients in the follow-up could recover their pre-injury thumb activity level without negative effects on their daily life and work and physical exercise activities. The mean thumb TAM loss was 7.5 ± 1.3°; there were four cases of TAM>10°, including two elderly patients with TAM>30°. Compared with those in the uninjured side, seven cases were excellent, 11 were good, one was moderate, and none was bad.
On Jamar thumb muscle testing in 24-month follow-up, grip force of the affected side was 65.5-113% of the uninjured side. The grip force of the affected side for one case with type IIIB fractures showed a 34.5% loss compared with that of the uninjured side without any loss of function, DASH score was 2 points, and TAM was good. The pinch strength of the affected side was 66.6-104.5% of the uninjured side. The pinch strength of the affected side for one case with type I fractures was a 26.7% loss compared with that of the uninjured side without functional limitations, DASH score was 3 points, and TAM was excellent. Among the patients with type II fracture, one had a 33.4% loss of pinching force, DASH score was 2 points, and TAM was good. In statistical analysis, the grip strength of the affected side did not differ significantly from the grip or pinch strength of the uninjured side (P<0.05).
Discussion
Common unstable fractures at the base of the first metacarpal include both intra-articular fractures such as Bennett fractures and Rolando fractures and extra-articular oblique fracture and transverse fractures.
Treatment of unstable fractures at the base of the first metacarpal is challenging. Before the 1970s, closed reduction and cast immobilization were the conventional treatments and considered to have good results as non-surgical treatments in some historical reports. However, currently, surgical intervention is generally recommended as first-line treatment for unstable fracture at the base of the first metacarpal. The common available internal fixations consist of screws or Kirschner wire. However, this direct fixation method requires open reduction to ensure stability between ends during screw placement to prevent bone piece separation and displacement. This increases the degree of local trauma, which can damage the articular cartilage and cause traumatic arthritis. Another method was percutaneous fixation of the first and second metacarpal bones and the use of Kirschner wire to achieve indirect fixation [7]. However, this technique may damage the tenor muscles and limit the thumb’s flexion and extension activities. Therefore, the use of closed reduction and external fixation in the treatment of unstable fractures at the base of the first metacarpal is a better choice.
Closed reduction can be the treatment for the vast majority of Bennett fractures [15]. Closed reduction was indirect, and the chosen technique is very important. In conventional techniques, it was particularly stressed that the thumb be placed in an outreaching dorsal extension position and the abductor pollicis longus tensed through axial traction or pressure be applied simultaneously to the base of the thumb metacarpal to reduce the fracture. However, practice showed that this reduction technique often failed to achieve a satisfactory reduction effect. This incorrect reduction technique was derived from the understanding that “abductor pollicis longus is the main cause of Bennett fracture dislocation.” This misunderstanding was widely present in the literature as well as textbooks. Many surgeons have found that the thumb was in extreme opposition since the abductor pollicis longus was relaxed when three fingers grasped things but was tensed when the thumb was in abduction and dorsal extension. As such, the traction force of the abductor pollicis longus was not the main cause of Bennett fracture displacement, so there was no need to put the thumb in the abduction and dorsal extension state to neutralize the traction force of the abductor pollicis longus in fracture reduction [16]. However, in the abduction and dorsal extension position, the base of the first metacarpal and the volar bone was separated to increase the fracture-separating gap and impede the fracture’s anatomical reduction.
A large number of anatomical studies confirmed that when the carpometacarpal joint was in a rest position, the palmaris of the first metacarpal bone was separated from the trapezium, carpometacarpal joint space was large, and palm oblique ligament and dorsal ligamentous complex were in a relaxed state. When the thumb was in a clenched clinched state, that is, when the thumb was in an active opposition or passive palm rotation position, the dorsal ligament was tensed and the palm oblique ligament was more relaxed than the rest, while the metacarpal palmaris was closer to the trapezium, carpometacarpal joint space was narrowing, and extension forces provided by the abductor pollicis longus and dorsal tension formed a dynamic couple with the strained oblique ligaments, which steered the instability of the carpometacarpal joint toward stability. This was the reset principle of the “screw home” technique.
In the use of closed reduction, physicians still need to pay attention to reduction quality; it must be repeatedly confirmed on the X-ray prior to fixation. Some authors studied the correlation between the quality and surgical reduction effect. The early literature reported that fracture reduction quality was not correlated with postoperative pain, activity, or incidence of osteoarthritis. Demir retrospectively studied 24 cases of Bennett fractures and six of comminute intra-articular fractures and reported that metacarpal base articular surface reduction quality and radiographic results had no correlation with subjective perception [17]. Cullen conducted a series of biomechanical studies and suggested that a partial shift of 2 mm on the articular surface can significantly increase the contact area of the carpometacarpal joint surfaces. Therefore, an intra-articular shift ≤ 2 mm was considered acceptable [18].
In recent years, a variety of clinical studies have reported on the importance of anatomical reduction and decreasing the articular surface step. Many scholars believed that reduction quality was associated with the incidence of osteoarthritis. The reduction standard should be more stringent, especially when the first carpometacarpal joint cartilage contact area was small. Kjaer-Petersen reported the treatment of 41 cases with Bennett fractures, including closed reduction and cast immobilization, closed reduction and percutaneous Kirschner wire fixation, and open reduction and internal fixation and analyzed the correlation between reduction treatment and clinical efficacy and found that anatomical reduction was achieved with a step <1 mm in 86% of patients, none of whom had any local symptoms; in contrast, only 46% of the patients with poor reduction and a step >1 mm did not have local complications [19]. Lutz reported the 7-year follow-up data of 32 cases of Bennett fracture treated with open reduction and internal fixation or closed reduction and percutaneous Kirschner wire fixation across the joints. Treatment methods and final clinical results were not correlated with the incidence of osteoarthritis. However, during surgery, the approach should be shifted to open reduction if the intra-articular displacement is >1 mm after closed reduction. This finding suggested that our longterm efficacy depended on reset quality rather than surgical method [5]. In our study, the reduction standard was also defined as articular surface displacement ≤ 1 mm, and the clinical results were satisfactory.
Many studies to date have examined the treatment of the base of the first metacarpal fractures using external fixators but lacked longer-term follow-up observations, particularly a description of specific functional recovery. In our study, a 24- month follow-up study was performed of the external fixation of fractures at the base of the first metacarpal in addition to radiographic comparisons, while other studies focused on subjective and objective evaluations of thumb function to fully evaluate the effect of surgery. The follow-up revealed that the treatment of unstable fractures at the base of the first metacarpal using closed reduction and external fixation had good therapeutic effect according to both, subjective indicators reflecting pain and function and objective indicators reflecting range of motion and muscle strength. However, age was an important prognostic factor, and elderly patients were more likely to have postoperative partial pain and decreased muscle strength and were more prone to joint degeneration in the advanced disease stage.
It was generally believed that the subcutaneously implanted threaded half needles reduced soft-tissue irritation to the maximum degree, reducing the possibility of infection and tendon injury [20]. However, there were three cases of needle tract infection treated with oral antibiotics. Needle tract infection can occur both inside and outside articular fractures. One patient had preoperative skin abrasions. As such, even in treatment using external fixators, surgeons should closely examine the soft tissue during the preoperative assessment and strengthen postoperative needle tract management to prevent infection.
In summary, closed reduction and external fixation can be effective and safe treatments for unstable fractures at the base of the first metacarpal. Such external fixation structures are simple and versatile and able to simultaneously achieve effects such as meeting the retractor, adjusting the angulation, and shortening the displacement, especially for local wounds. However, exposed external fixation is inconvenient in daily life and there was a certain needle tract infection rate. The limitations of the present study were that nearly 20% of patients did not complete the 24-months follow-up period. This was a case study that lacked a control group. In addition, objective assessment criteria were lacking. Finally, during the Jamar dynamometer strength test, the dominant hand was not considered and some errors occurred.
Conflicts of Interest
All of the authors declare that they have no conflicts of interest regarding this paper.
References
- Mahmoud M, El Shafie S, Menorca RM, Elfar JC. Management of neglected Bennett fracture in manual laborers by tension fixation. J Hand Surg Am 2014; 39: 1728-1733.
- Giddins GE. The non-operative management of hand fractures. J Hand Surg Eur 2015; 40: 33-41.
- Liverneaux PA, Ichihara S, Hendriks S, Facca S, Bodin F. Fractures and dislocation of the base of the thumb metacarpal. J Hand Surg Eur Vol 2015; 40: 42-50.
- Middleton SD, McNiven N, Griffin EJ, Anakwe RE, Oliver CW. Long-term patient-reported outcomes following Bennett's fractures. Bone Joint J 2015; 97-B: 1004-1006.
- Lutz M, Sailer R, Zimmermann R, Gabl M, Ulmer H, Pechlaner S. Closed reduction transarticular kirschner wire fixation versus open reduction internal fixation in the treatment of Bennett fracture dislocation. J Hand Surg Br 2003; 28: 142-147.
- Diaconu M, Facca S, Gouzou S, Liverneaux P. Locking plates for fixation of extra-articular fractures of the first metacarpal base. Chir Main 2011; 30: 26-30.
- Greeven AP, Alta TD, Scholtens RE, de Heer P, van der Linden FM. Closedreduction intermetacarpal Kirschner wire fixation in the treatment of unstablefractures of the base of the first metacarpal. Injury 2012; 43: 246-251.
- Abid H, Shimi M, El Ibrahimi A, El Mrini A. Articular fracture of the base of the thumb metacarpal: comparative study between direct open fixation and extrafocal pinning. Chir Main 2015; 34: 122-125.
- Meng L, Zhang Y, Lu Y. Three-dimensional finite element analysis of mini-external fixation and Kirschner wire internal fixation in Bennett fracture treatment. Orthop Traumatol Surg Res 2013; 99: 21-29.
- Marsland D, Sanghrajka AP, Goldie B. Static monolateral external fixation for the Rolando fracture: a simple solution for a complex fracture. Ann R Coll Surg Engl 2012; 94: 112-115.
- Zhang X, Shao X, Zhang Z, Wen S, Sun J, Wang B. Treatment of a Bennettfracture using tension band wiring. J Hand Surg Am 2012; 37: 427-433.
- El-Sharkawy AA, El-Mofty AO, Moharram AN, Abou Elatta MM, Asal F. Management of Rolando fracture by modified dynamic external fixation: a new technique. Tech Hand Up Extrem Surg 2009; 13: 11-15.
- Niempoog S, Waitayawinyu T. Comminuted Rolando’s fracturess: treatment with modified wrist external fixator and transmetacarpal pinning. J Med Assoc Thai 2007; 90: 182-187.
- Maru M, Jettoo P, Tourret L, Jones M, Irwin L. Thumb carpometacarpal osteoarthritis: trapeziectomy versus pyrocarbon interposition implant (Pi2) arthroplasty. J Hand Surg Eur Vol 2012; 37: 617-620.
- Roth JJ, Auerback DM. Fixation of hand fractures with bicortical screws. J Hand Surg Am 2005; 30: 151-153.
- Weinstein LP, Hanel DP. Metacarpal fractures. J Am Soc Surg Hand 2002; 2: 168-180.
- Demir E, Unglaub F, Wittemann M, Germann G, Sauerbier M. Surgically treated intraarticular fractures of the trapeziometacarpal joint-a clinical and radiological outcome study. Unfallchirurg 2006; 109: 13-21.
- Cullen JP, Parentis MA, Chinchilli VM, Pellegrini VD Jr. Simulated Bennett fracture treated with closed reduction and percutaneous pinning. A biomechanical analysis of residual incongruity of the joint. J Bone Joint Surg 1997; 79: 413-420.
- Kjaer-Petersen K, Langhoff O, Andersen K. Bennett’s fracture. J Hand Surg Br 1990; 15: 58-61.
- Kozin SH, Thoder JJ, Lieberman G. Operative treatment of metacarpal and phalangeal shaft fractures. J Am Acad Orthop Surg 2000; 8: 111-121.