Case Report - Current Pediatric Research (2017) Volume 21, Issue 3
Tuberculosis in children in a hospital in the Suburbs of Dakar, Senegal
Jean Baptiste Diouf1, Khadime Sylla2, Amadou Lamine Fall31Departement of Pediatric, Centre Hospitalier Roi Baudouin, Guédiawaye, Senegal.
2Laboratory of Parasitology-Mycology, Faculty of Medicine, Cheikh Anta Diop University, Dakar, Sénégal.
3Department of Pediatric, Faculty of Medicine, University Cheikh Anta Diop, Dakar, Sénégal.
- Corresponding Author:
- Jean Baptiste Diouf
Centre Hospitalier Roi Baudouin de Guédiawaye
Dakar, Sénégal
Tel: 00221338374647
Fax: 00221338770261
E-mail: jeanniokhor@yahoo.fr
Accepted date: June 21, 2017
Abstract
Introduction: Tuberculosis remains a major public health problem in Senegal despite all the means used to deal with this disease. In an attempt to strengthen tuberculosis control in children, it was envisaged to undertake this study, the main objective of which was to describe the epidemiological, clinical and evolutionary profile of tuberculosis cases, all types taken together, in children monitored at the Centre hospitalier Roi Baudouin de Guédiawaye. Materials and methods: A descriptive retrospective study was carried out from 1 January 2010 to 31 December 2014 in the Centre hospitalier Roi Baudouin de Guédiawaye located in the Dakar suburbs. Tuberculosis cases diagnosed in children during the reporting period were compiled from patient records specially designed for this purpose. The data was entered on Excel and the analysis was done using Stata IC 12 software. Results: A total of 121 new cases of tuberculosis were reported in children during the study period. The average age of the children was 10.84 years. The study population was predominantly female (52.89%). Pulmonary location was more frequent with 70.25% of cases. Extra pulmonary locations were mainly represented by lymph node (30.55%), osteoarticular (16.67%) and pleural (13.89%) forms. The bacilloscopy was positive in 47.93% of the cases. Tuberculosis was associated with HIV in 14.05% of cases. The evolution was favourable in the majority of cases and the hospital mortality was 4.96%. Conclusion: Given that childhood tuberculosis is still common and mortality high, there is need for further studies to identify the factors contributing to the fact that this epidemiological situation remains unchanged.
Keywords
Tuberculosis, Children, Senegal.
Introduction
Tuberculosis is a major global public health problem. Its prevalence increases with HIV infection. According to the WHO, in 2015, 10.4 million of tuberculosis cases were noted with about 1.8 million deaths. More than 95% of deaths occur in low- and middle-income countries [1]. An estimated one million children with tuberculosis and 170,000 deaths are found in HIV-negative children [1].
Putting an end to the TB epidemic by 2030 is one of the health targets set out in the recently adopted sustainable development goals of the United Nations. In Senegal, while major advances have been made in screening for and successfully treating the disease, it must be recognized that tuberculosis management in children is still inadequate. Indeed for the year 2012, infant forms accounted for only 5.2% of the cases instead of the 11% expected [2].
In an attempt to strengthen tuberculosis control in children, it is necessary to re-evaluate tuberculosis epidemiology in children. It is in this context that this study was conducted with the main objective to evaluate the epidemiological, clinical and evolutionary aspects of tuberculosis in children seen at the Centre hospitalier Roi Baudouin de Guédiawaye.
Patients and Methods
A descriptive retrospective study was conducted from 1 January 2010 to 31 December 2014 at the Centre hospitalier Roi Baudouin de Guédiawaye. This health facility is located in Guédiawaye, which is one of the four departments in the Dakar region. It is located 17 km from the city centre of the capital city in a peri-urban area located in the Niayes with a sub-Sahelian climate.
The Centre hospitalier Roi Baudouin is a level 1 public health institution with outpatient services, medical and surgical hospitalization and diagnostic assistance (medical imaging and laboratory). It also has a tuberculosis treatment centre headed by a state nurse in charge of providing tuberculosis treatment in accordance with the protocol of the National Tuberculosis Control Programme. Treatment is administered daily under direct supervision in children and adults. It consists of two phases: an intensive phase followed by a continuation phase. The treatment schedule will depend on the category, age and location.
All children aged 0-15 years received in this Centre for tuberculosis, all types taken together, were included. Sociodemographic (age and sex), clinical (type and location of tuberculosis), biological (search for BAAR) and evolutionary information (cured, lost to follow-up, transferred or deceased) were collected. Age was defined in three categories: under-5 age group; category between 5 to 10 years and category of over 10 years. The data was entered on Excel and the analysis was performed using STATA IC 12 software. Quantitative variables were described in terms of mean and standard deviation. Qualitative variables were described in terms of numbers and percentages of data. The tests significance threshold was set at 5%.
Results
Demographic Characteristics of Patients
Children's ages varied between 3 months and 15 years with an average of 10.84 years. The study population was predominantly children aged over 10 years, with a percentage of 71.90% (n=87). Children under 5 years of age accounted for 14.88% and those aged 5 to 10 represented 13.22%. The study population was predominantly female (52.89%). Male subjects accounted for 47.11%, i.e., a sex ratio of 0.9 (Table 1).
| Parameters | Total n° | Percentage (%) |
|---|---|---|
| Age | ||
| <5 years | 18 | 14.88 |
| 5-10 years | 16 | 13.22 |
| ³ 10 years | 87 | 71.90 |
| Sex | ||
| Male | 57 | 47.11 |
| Female | 64 | 52.89 |
Table 1: Socio-demographic characteristics of patients
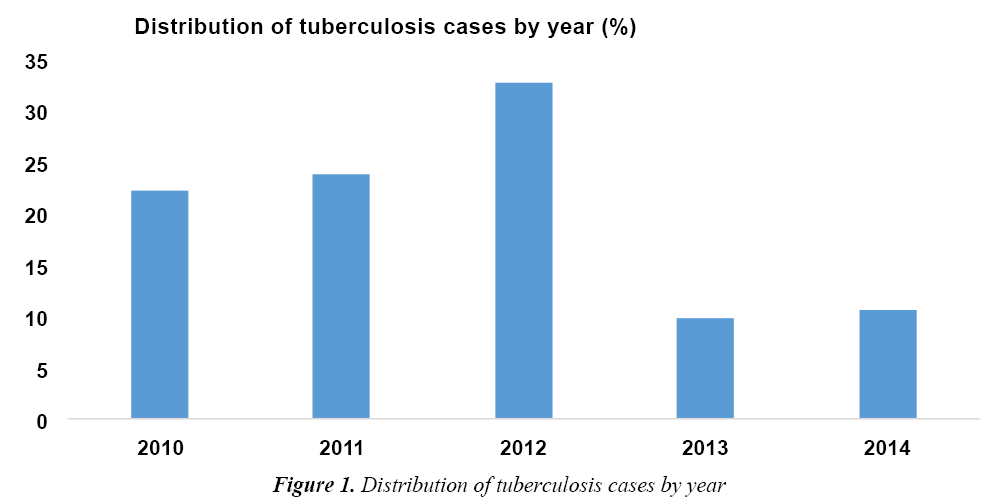
Distribution of Tuberculosis Cases by Year
During the study period, 846 patients received tuberculosis treatment, of which 121 were between 0 and 15 years of age, i.e., an infantile proportion of 14.3%. The distribution by year showed that the number of tuberculosis cases was higher in 2012 (40 cases), i.e., 33.05%, followed by 2011 (23.9%) and 2010 (22.3%). The incidence of tuberculosis in 2013 and 2014 was 12 and 13 cases, respectively (Figure 1).
Clinical, Biological and Evolutionary Patient Profile
Pulmonary tuberculosis forms were predominant with 70.25% of cases (n=85). In contrast, extra pulmonary forms accounted for 29.75%. For these extra pulmonary forms, the lymph node forms represented 30.55%, the osteo-articular forms 16.67% and the pleural forms 13.89%.
In 22.22% of cases, the location of the extra pulmonary form was not specified. A positive bacilloscopy was found in 47.93% of cases. Co-infection with HIV was found in 14.05% of cases.
With regard to evolution, the cure was obtained in 90.91% of the cases, 3 patients (2.48%) were lost to follow-up and 2 patients (1.65%) transferred. 6 death cases were recorded, i.e., a mortality rate of 4.96%. One case of relapse was noted after follow-up (Table 2).
| Parameters | Total n° | Percentage (%) |
|---|---|---|
| Location | ||
| Pulmonary | 85 | 70.25 |
| Extra pulmonary | 36 | 29.75 |
| Bacilloscopy | ||
| Positive | 58 | 47.93 |
| Negative | 63 | 52.07 |
| Co-infection VIH | ||
| Yes | 17 | 14.05 |
| No | 104 | 85.95 |
| Evolution | ||
| Cured | 110 | 90.91 |
| Deceased | 6 | 4.96 |
| Lost to follow-up | 3 | 2.48 |
| Transferred | 2 | 1.65 |
Table 2: Clinical, biological and evolutionary patient profile
Of the extra pulmonary forms, lymph node, osteo-articular and pleural locations were more frequent with 30.55%, 16.67% and 13.89%, respectively. Cutaneous forms accounted for 5.56%.
Miliary, meningeal, peritoneal and multifocal tuberculosis accounted each for 2.78%. In 22.22% of extra pulmonary location cases, the form was not specified (Table 3).
| Extra-pulmonary location | Total n° | Percentage (%) |
|---|---|---|
| Lymph node | 11 | 30.55 |
| Osteo-articular | 6 | 16.66 |
| Pleural | 5 | 13.89 |
| Cutaneous | 2 | 5.56 |
| Miliary | 1 | 2.78 |
| Multifocal | 1 | 2.78 |
| Meningeal | 1 | 2.78 |
| Peritoneal | 1 | 2.78 |
| Unspecified | 8 | 22.22 |
Table 3: Extra-pulmonary locations
Pulmonary forms were more frequent in children over 10 years of age. In contrast, extra pulmonary forms were noted in children less than 5 years of age. The difference was not significant between the different age groups (p=0.2).
Bacilloscopy turned positive in 60.91% in children over 10 years of age (p<10-3). Tuberculosis and HIV co-infection was higher in children over 10 years of age, i.e., 10.34% and in and those aged 5 to 10, i.e., 10.34% (p=0.82).
Two lost to follow-up cases were found in children less than 5 years of age and one case was reported in children over 10 years of age. No lost to follow-up case was observed in children aged between 5 and 10 years.
The cure rate was higher in children over 10 years of age (97.70%). On the other hand, it was almost similar in children under 5 years and in those aged between 5 and 10 years.
Tuberculosis mortality was higher in children under 5 years of age (16.67%), followed by children aged 5 to 10 years (12.50%). A single death case was noted in children over 10 years of age, i.e., a rate of 1.15% (Table 4).
| Variables | <5 years n=18 |
[5-10 years] n=16 |
³ 10 years n=87 |
|---|---|---|---|
| Location | n (%) | n (%) | n (%) |
| Pulmonary | 10 (55.56) | 10 (62.50) | 65 (74.71) |
| Extra pulmonary | 8 (44.44) | 6 (37.50) | 22 (25.29) |
| Bacilloscopy | |||
| Positive | 1 (5.55) | 4 (25) | 53 (60.91) |
| Negative | 17 (94.45) | 12 (75) | 34 (39.09) |
| Co-infection with HIV | |||
| Positive | 3 (16.67) | 5 (31.25) | 9 (10.34) |
| Negative | 15 (83.33) | 11 (68.75) | 78 (89.66) |
| Evolution | |||
| Cured | 12 (66.67) | 13 (81.25) | 85 (97.70) |
| Lost to follow-up | 2 (11.11) | 0 (00.00) | 1 (1.15) |
| Transferred | 1 (5.55) | 1 (6.25) | 0 (00.00) |
| Deceased | 3 (16.67) | 2 (12.50) | 1 (1.15) |
Table 4: Clinical, biological and evolutionary profile of patients by age
Discussion
The goal of our study was to study the epidemiological, clinical and evolutionary aspects of tuberculosis in children. Thus, an infant proportion of 14.3% with an age that varied between 3 months and 15 years was noted. The average age was 10.84 years. This average higher than that found in Dakar by Ba et al. [3] (5 years) and Hailu et al. [4] in Lomé (8.5 years) is identical with those found in other studies in Kenya (9 years) [5] and Algeria (9.7 years) [6].
In our study, major pulmonary forms with 70.25% of cases (n=85) were more frequent in children over 10 years of age. Ba et al. [3] in Senegal found 83% of pulmonary forms. In France, pulmonary locations account for 62% of reported cases in children under 5 and 49% between 5 and 15 years of age [7]. These different results confirm that pulmonary forms predominate in the reported tuberculosis cases.
The bacilloscopy was positive in 47.93% of the cases in our series. Similarly, Ba et al. [3] and Zemour et al. [6] found similar results in Senegal and Algeria with 41% and 53%, respectively. Sputum smears were positive only in 10-15% of cases and culture confirmation only in 30% to 40% [8,9]. Furthermore, the bacilloscopy in our series returned positive in 60.91% in children over 10 years (p<10-3). In France, cases with a positive direct examination result on breathing sampling accounted for 30% of pulmonary cases in children under 15 years of age, compared to 56% in patients aged 15 years and older (p<0.001) [7]. These results show that in older children, the bacilloscopy positivity rate is greater.
Extra pulmonary forms accounted for 29.75% and were dominated by lymph node (30.55%), osteo-articular (16.67%) and pleural (13.89%) forms. In 22.22% of cases the location of the extra pulmonary form was not specified. Similarly, these extra pulmonary forms were more marked in children under 5 years of age, but the difference was not significant between the different age groups (p=0.2). Elsewhere in Africa, for Zemour et al. [6], the extra-pulmonary tuberculosis forms accounted for 58.3% of cases, lymph node forms 60.9% and primary tuberculous infections 15.1%. In France, the incidence of extra pulmonary manifestations stood at 31% [10].
With regard to evolution, the cure was obtained in 90.91% of the cases. This result is similar to that found by Ba et al. in Senegal (89%) [3]. This recovery is greater in children over 10 years of age (97.70%).
There were 6 death cases, i.e., a lethality rate of 4.96%. Tuberculosis-related mortality was higher among children under five years of age (16.67%). This could be explained by the fact that severe forms are more frequent in this age group. Higher lethality has been reported in other studies in Botswana (10.5%) and Malawi (17%) [11,12].
Our study was conducted in hospital settings attended by sick children, which may be a limitation in the assessment of prevalence. Similarly, poor record keeping and lack of systematic screening for HIV and malnutrition among these children with TB are also limitations. Therefore, multicentric studies including more advanced diagnostic techniques (Genexpert, culture on specific environment) as well as research into contributing factors (HIV and malnutrition) could help to improve the tuberculosis characteristics in children in Senegal.
Conclusion
This study shows that tuberculosis prevalence remains high in children with a predominance of pulmonary forms. The bacilloscopy positivity rate is higher in children over 5 years of age, whereas severe and extra-pulmonary forms are dominated by children under 5 years of age. The still high mortality rate despite the treatment raises the problem of multi-resistance. It is therefore necessary to carry out further studies in order to identify the factors contributing to the perpetuation of this epidemiological situation.
References
- http://www.who.int/mediacentre/factsheets/fs104/en/
- Ministry of Health and Social Action, Senegal. A guide for the management of childhood tuberculosis (2012 Edn). Accessed May 17, 2017.
- Ba ID, Ba A, Faye PM, et al. Tuberculosis of the child in Senegal: Epidemiological, clinical, therapeutic and evolutionary aspects. Med Af Black 2015; 6204: 200-206.
- Hailu D, Abegaz We, Belay M. Childhood tuberculosis and its treatment outcomes in Addis Abeba: A 5 years retrospective study. BMC Pediatr 2014; 14: 61-67.
- Akolly DAEB, Guedenon KM, Mihluedo KA. Tuberculosis of immunocompetent children and adolescents in Lomé. Arch Pediatr 2015; 22: 233-371.
- Zemour L, Belghitri A, Chougrani S. Epidemiological profile of tuberculosis in children in Remchi (2000-2011). In: 16th Congress of French Language Respirology, Lyon 2012.
- Antoine D, Che D. Epidemiology of tuberculosis in France. Record of cases reported in 2008. BEH 2010; 27: 289-293.
- Starke JR. Pediatric tuberculosis: Time for a new approach. Tuberculosis 2003; 83: 208-212.
- Zar HJ, Hanslo D, Apolles P, et al. Induced sputum versus gastric lavage for microbiological confirmation of pulmonary tuberculosis in infants and young children: A prospective study. Lancet 2005; 365: 130-134.
- Pontual LD. Tuberculosis in adolescents. A French retrospective study of 52 cases. PIDJ 2006; 25: 130-132.
- Oeltmann Je, Chengeta B, Mboya JJ, et al. Reported childood tuberculosis treatment outcomes, Gabarone and Francistown, Botswana, 1998-2002. Int J Tuberc Lung Dis 2008; 12: 186-192.
- Tabho CM, Irongo CF, Boeree MJ, et al. Childhood tuberculosis in the Kilimanjaro region: Lesson from and for the TB programme. Trop Med Int Health 2010; 15: 496-501.