Case Report - Journal of Cell Biology and Metabolism (2018) Histology and Cell Biology
Tromboembolic recurrence parallel to the progression of breast cancer: Risk factors and central venous catheter thrombosis.
Losada B1*, Gutierrez D1, Pantin MC1, Anton B1, Guerra JA1, De Torres MV2
1Department of Medical Oncologist, Fuenlabrada Universitary Hospital, Madrid, Spain
2Department of Radiation Oncologist, Fuenlabrada Universitary Hospital, Madrid, Spain
- *Corresponding Author:
- Losada B
Department of Medical Oncologist
Fuenlabrada Universitary Hospital
Madrid
Spain
Tel: +34 916 00 60 00
E-mail: beamenta@hotmail.com
Accepted Date: May 31, 2018
Citation: Losada B, Gutierrez D, Pantin MC, et al. Tromboembolic recurrence parallel to the progression of breast cancer: Risk factors and central venous catheter thrombosis. J Child Adolesc Health. 2018;1(1):6-7.
Abstract
Thromboembolic disease (VTE) is a very important cause of morbidity and mortality in cancer patients, with a recurrence rate between 10% -17% of patients treated with anti-Vitamin K drugs and 6-9% of low molecular weight heparin (LMWH) (1). This case reflects on the recurrence of VTE, the management of thrombosis associated with central venous catheter (CVC) and prothrombotic risk factors.
Keywords
Thromboembolic disease (VTE), Anti-Vitamin K, Risk factors, Thrombophlebitis, Anticoagulation.
Case Presentation
A 60 years old patient with antecedent of righ breast infiltrating ductal carcinoma pT1cN0M0 RRHH + c-erb2- in 2004 treated with mastectomy with axillary lymphadenectomy and adjuvant treatment with aromatase inhibitor until February 2009 (5 years).
After 2 years without treatment (July 2011), he went to the Emergency Department due to dyspnea with the appearance of a right pleural effusion of tumor origin. Before starting chemotherapy, the patient presented with tachycardia, oxygen saturation of 89% and D-Dimer determination of 5340 ng / mL. Urgent angio-CT showed congruent findings with acute pulmonary thromboembolism (segmental main pulmonary arteries). The echocardiogram showed no signs of overload in the right ventricle. Since there was no contraindication for anticoagulation and it was not a massive pulmonary thromboembolism, tinzaparin was started at 14,000 IU / ML and 1st line of chemotherapy (Paclitaxel), and a port-a-cath was placed for it.
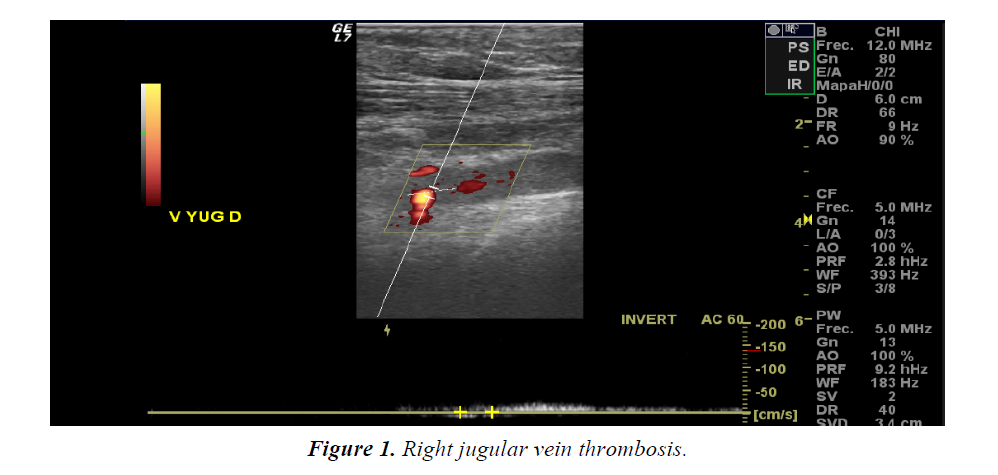
At 12 months (July 2012) he went to the Emergency Department for laterocervical discomfort and in the right supraclavicular fossa without increasing dyspnea. An upper Doppler echocardiogram was performed (Figure 1) showing right subclavian thrombosis secondary to catheter. We decided to withdraw from Port-a-cath since it was already anticoagulated with LMWH at therapeutic doses and the dose of tinzaparin was increased to 16,000 IU/ mL and anti-XA was monitored (always with values in normal range). Thrombophilia study showed no alterations. After 2 weeks, the dose of tinzaparin was again reduced to 14,000 IU / ml and there were no new complications or signs of bleeding.
The tumor disease was reevaluated at that time, presenting progression at a bone level, so the treatment scheme was modified to Fulvestrant intramuscular (hormone therapy), remaining with stable disease since then and without new signs of bleeding. He maintains anticoagulant treatment and has not needed a new port-a-cath placement because he continues receiving an intramuscular treatment.
Conclusion
• Thromboembolic disease is a very important cause of morbidity and mortality in cancer patients. Recurrence rate is 10-17% with anti-Vitamin K and 6-9% with low molecular weight heparins [1].
• 12% of VTE are synchronous with the diagnosis of the tumor, and in hospitalized patients the incidence ranges between 0.6% and 18% [2].
• This patient presents as risk factors the following ones: breast cancer (risk of 2.8%), advanced stage, a recent diagnosis (first 3-6 months increases by 2.2 times) and chemotherapy (increaseses the risk by 6.5 times) [3]
• Ottawa score assesses risk according to age, sex, type of primary tumor and stage [4]. The risk of thromboembolic recurrence is more frequent in tumor progression, as occurred in our patient.
• In thromboembolic recurrence, there is no evidence to support the change to another LMWH or the inferior Vena Cava filter.
• Before a catheter-associated thrombosis, withdrawal is not recommended if the distal area is correctly positioned, its use is vital or there are no signs of infection or thrombophlebitis. In our case, given that the patient was already anticoagulated and was thought to be in progression, we decided to withdraw to avoid further complications [5].
• There are no data about anticoagulation with duration beyond 6 months, but before active disease such as that of our patient, it must be maintained indefinitely unless the risk of bleeding or other complications outweighs the benefit [6].
References
- Chew HK, Wun T, Harvey D, et al. Incidence of venous thromboembolism and its effect on survival among patients with common cancers. Arch Intern Med. 2006;166:458-64.
- Khorana AA, Francis CW, Culakova E, et al. Frequency, risk factors, and trends for venous thromboembolism among hospitalized cancer patients. Cancer. 2007;110:2339-46.
- Horner T, Mahan CE . Venous thromboembolism: role of pharmacists and managed care considerations. Am J Manag Care. 2017;23(20):391-98.
- Alatri A, Mazzolai L, Kucher N, et al. The Modified Ottawa Score and Clinical Events in Hospitalized Patients with Cancer-Associated Thrombosis from the Swiss VTE Registry. Semin Thromb Hemost. 2017;43(8):871-76.
- Simon EM, Summers SM. Vascular Access Complications: An Emergency Medicine Approach. Emerg Med Clin North Am. 2017;35(4):771-88.
- Prandoni P, Lensing AW, Piccioli A, et al. Recurrent venous thromboembolism and bleeding complications during anticoagulant treatment in patients with cancer and venous thrombosis. Blood. 2002;100:3484-8.