Research Article - Biomedical Research (2017) Volume 28, Issue 20
Traumatic rupture of the diaphragm: A 22-patient experience
1Department of Thoracic Surgery, Bursa Yuksek Ihtisas Training and Research Hospital, Bursa, Turkey
2Department of Emergency Medicine, Bursa Yuksek Ihtisas Training and Research Hospital, Bursa, Turkey
- *Corresponding Author:
- Erkan Akar
Department of Thoracic Surgery
Bursa Yuksek Ihtisas Training and Research Hospital, Turkey
Accepted date: September 6, 2017
Abstract
This study evaluated the demographic and clinical properties, diagnostic and therapeutic approaches, and outcomes of patients with traumatic diaphragmatic injury. Among 853 patients who presented with blunt or penetrating thoracic injury between January 2010 and December 2016, 22 patients with traumatic diaphragmatic rupture were retrospectively studied. The analysed parameters included age, sex, accompanying injuries, surgical management approach, postoperative morbidity and mortality rates, and duration of hospital stay. Among 853 patients treated at our clinic for blunt or penetrating thoracic trauma, 22 patients with diaphragmatic injury (16 males, 6 females) were evaluated. The mean age was 32 (range 19-67 y). Twenty-one patients were evaluated in the acute setting and 1 in the chronic setting (with a history of trauma 8 years earlier). The most common complaints and physical examination findings were dyspnea, chest pain, abdominal distention, and loss of breath sounds over the affected hemithorax. On chest X-Ray the most common signs included loss of dipahragma shadow, diaphragmatic elevation, and visceral organ herniation into thoracic cavity. All patients were operated. As the surgical method, thoracotomy was carried out in 18 patients and laparotomy+thoracotomy was performed in 4 patients. Three patients underwent diagnostic video-assisted thoracoscopy before thoracotomy. Diaphragma was repaired on the left side in 20 patients and on the right side in 2. In 21 patients, a diaphragmatic injury was accompanied by intraabdominal organ injuries, lung injuries, and other system injuries. Stomach was the organ whose injury most commonly accompanied blunt and penetrating injuries. Pulmonary complications were more common in blunt traumas (10%). Death was seen in only one (5%) patient with penetrating trauma. The mean duration of chest drainage tube staying in place was 3 (range 2-8 d); the mean duration of hospital stay was 6 (range 4-10 d).
Keywords
Diaphragmatic hernia, Blunt, Penetrating, Injury
Introduction
Traumatic Diaphragmatic Injury (TDI) may occur after both blunt and penetrating injuries involving thorax and abdomen [1,2]. The rate of diaphragmatic rupture is 0.8-1.6% with abdominal injuries and 10-15% with thoracic injuries [3]. TDI is commonly associated with multiple organ injuries. In blunt trauma, diaphragm rupture due to a sudden increase in intraabdominal pressure is mostly left-sided, with the left/right rupture ratio being 3/1 [4].
Penetrating diaphragmatic injury, on the other hand, generally occurs after sharp penetrating object or gunshot injuries and blunt trauma, and particularly affects lower thoracic and upper abdominal regions [3].
The clinical course of TDI is varied by its size, origin, and location. Masking of TDI by other more severe lesions and injuries necessitating urgent care often complicates or delays its diagnosis [5,6].
Small lesions, particularly those that develop secondary to penetrating injuries or those affecting the right hemidiaphragm, may be missed or diagnosed late in the course. Injuries below the intramammarian line or above the umbilicus should raise suspicion of the condition [7].
Clinical presentation may include respiratory difficulty, cardiac signs, trachea deviation, and auscultation of bowel sounds in the thoracic cavity. The most important point to remember is being suspicious of diaphragm injury in trauma patients.
The diagnosis is made by plain chest film, Ultrasonography (USG), Computerized Tomography (CT), fluoroscopy, stomach and colon films, and Video-Assisted Thoracoscopy (VATS). Abdominal herniation aiding in diagnosis may be absent and an initial chest film may be non-diagnostic in some cases [5,8,9].
Rupture must be surgically repaired before complications like incarceration and strangulation develop as soon as a diagnosis is made. Laparotomy is preferred particularly for left-sided injuries due to the presence of potential additional intraabdominal organ injuries at the acute stage [10].
Thoracotomy is feasible for right-sided lesions when intraabdominal injury is not considered. Thoracotomy is preferred for delayed ruptures due to presence of adhesions [11]. Here in we aimed to stress the importance and outcomes of diaphragmatic injuries associated with thoracic injuries.
Materials and Methods
We conducted a retrospective cohort study of adult patients with TDIs treated at Bursa Yuksek Ihtisas Training and Research Hospital, Turkey, using its trauma data registry. The study was approved by its ethics committee.
Among 853 patients who presented with blunt or penetrating thoracic injury between January 2010 and December 2016, 22 patients with traumatic diaphragmatic rupture were retrospectively studied for their demographic properties, age and sex, cause of injury, clinical findings, diagnostic modalities, surgical approach and surgical repair type, organs herniated into thoracic cavity, simultaneous organ injuries, and morbidity and mortality rates. The majority of injuries were above the arcus costalis, i.e. the lower thoracoabdominal border. Diagnostic modalities used for diagnosis included plain chest films, CT, (thoracic and lower thoracoabdominal) USG, and imaging studies with contrast. However, VATS was carried out in some suspected cases where definitive diagnosis could not be made.
Diaphragmatic rupture was suspected in case of an inability to distinguish diaphragmatic contours, diaphragm elevation, left lower lobe atelectasis, and appearances of colonic haustrations and auscultation of intestinal sounds in the thoracic cavity.
Surgical intervention was based on the type of occurrence and localization of trauma, and included thoracotomy, laparotomy, and thoracoabdominal intervention. The operation was started with VATS, and when a diaphragm rupture was localized, that defect was repaired. While the defect was repaired with a number 0 nonabsorbable single silk sutures, a polypropylene graft was placed to diaphragma in the case of delayed diagnosis. All patients were applied tube thoracostomy.
Data was analysed using descriptive statistics via IBM SPSS Statistics version 21.0 (IBM Corp, Armonk, NY, USA). The parameters of sex and age were compared using the Student’s t test; Fisher’s exact test was used for the comparison of sex and blunt and penetrating trauma; univariate Chi-square test was used to test compare additional injuries and complications. A p value of less than <0.05 was considered statistically significant.
Results
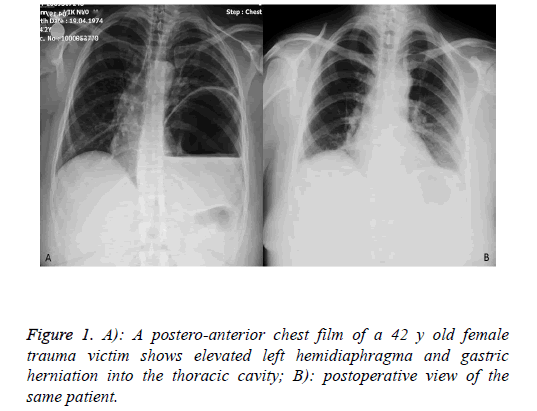
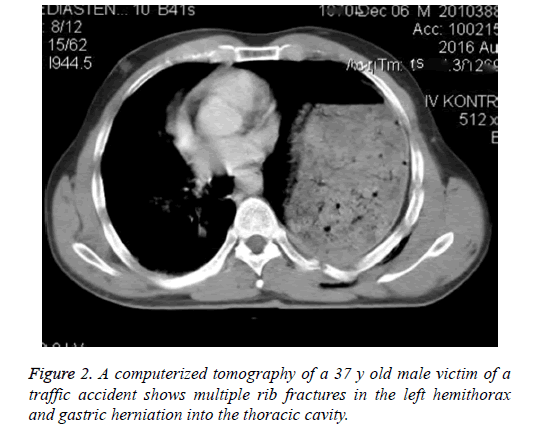
Among 853 patients who presented with blunt or penetrating thoracic trauma between January 2010 and December 2016, 22 (16 males and 6 females) patients with TDR had a mean age of 32 (range, 19-67 y). Twenty-one patients were evaluated in the acute setting and 1 in the chronic setting (traffic accident 8 years earlier). The most common complaints and physical examination findings were dyspnea, chest pain, abdominal distention, and loss of breath sounds over the affected hemithorax. The most common findings on plain chest film included loss of diaphragmatic shadow, diaphragm elevation, and visceral organ herniation into the thoracic cavity. The diagnosis was made by a chest film, a thoracic CT, and VATS (Figures 1 and 2).
TDI occurred after traffic accidents in 14 (63.6%) patients, sharp object injury in 4 (18.2%), fall from a height in 3 (13.6%), and gunshot injury in 1 (0.6%). The most common injury occurring in addition to the diaphragm was stomach perforation in 4 (19.0%) patients, multiple rib fractures in 6 (28.6%) patients, extremity fracture in 2 (9.5%) patients, liver injury in 2 (9.5%) patients, splenic injury in 1 (4.8%) patient, pelvic fracture in 3 (14.3%) patients, scapula fracture in 1 (4.8%) patient, and transverse process fracture in 2 (4.8%) patients.
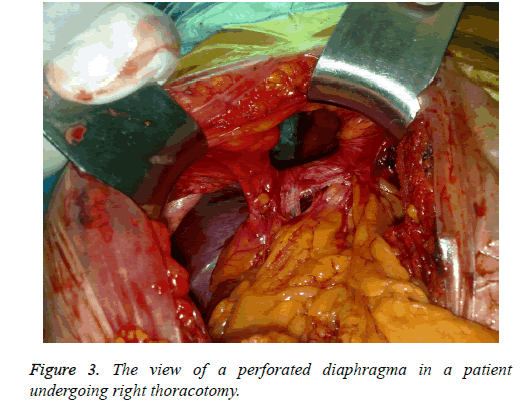
TDI involved the left side in 20 (91%) patients and the right side in 2 (9%) patients. Liver laceration was identified by thoracotomy+laparotomy in these patients. Thoracotomy was applied in 18 patients as the surgical approach (Figure 3). In four patients who underwent thoracotomy for active hemorrhage, gastric perforation was identified at the operation and the incision was converted to a thoracoabdominal one. Three patients underwent VATS for diagnostic purposes before thoracotomy. Six patients were operated within the first six hours whereas one patient was diagnosed 8 years later. In the remaining 15 patients, the diagnosis and operations were made in the first 1-2 d. A left-sided diaphragmatic repair was performed in 20 cases and a right-sided one in 2 cases. Diaphragmatic injury was associated with intraabdominal organ injuries, lung injuries, and other systemic injuries in 21 cases. The most commonly herniated organ after blunt and penetrating diaphragm injury was the stomach in 11 patients, followed by omentum in 9 patients, and the stomach, omentum, colon, and spleen combined in 1 patient. As morbidity, pulmonary complications occurred more commonly after blunt trauma (10%). Only one case of death due to acute respiratory failure and hypovolemic shock occurred in a victim of a penetrating trauma (5%). The mean duration of chest drainage tube staying in place was 3 (range, 2-8 d); the mean duration of hospital stay was 6 (range, 4-10 d). The patients were followed for a mean of 18 (range, 3-24 months), and respiratory function tests and plain chest films were taken as the follow-up tests. The patients were evaluated for changes in clinical status, recovery process, and complications. No significant differences were found between the groups with respect to injury type, sex, and age (p>0.05).
Discussion
TDI occurs in 0.8-7% of patients with blunt trauma and 10-15% of patients with penetrating trauma [12]. It has been reported that 75% of all diaphragmatic injuries occur by blunt trauma and 25% by penetrating trauma [13]. In our study, 77% of all diaphragmatic injuries were caused by blunt trauma and 23% by sharp object injury. The most common cause was traffic accidents (63.6%).
Penetrating diaphragmatic injuries occur as a result of sharp object or gunshot injuries affecting lower chest or upper abdomen from anterior, posterior, or lateral aspects. Sharp object or gunshot injuries affecting diaphragm may give rise to smaller defects. Injuries associated with sharp object injury tend to be missed at first but they may cause serious complications in the long term [14].
Blunt traumas can cause rupture from the congenitally weak posterior diaphragmatic region. Such injuries develop as a result of pressure changes associated with a sudden increase of intraabdominal pressure. The diaphragm is severely injured by high-energy traumas such as motor vehicle accidents and falls from a height, allowing the diagnosis being timely made by virtue of disrupted respiratory mechanics [1].
Diaphragmatic injuries can be having an insidious asymptomatic course. Diaphragmatic injury is not expected to be clinically apparent in a trauma patient [14]. Hence, TDI may be missed easily at the acute term. The radiological view of herniated organs may be confused with pneumothorax in delayed cases [15].
A person with chest injury having concurrent abdominal symptoms should raise suspicion of the condition. On the other hand, an abdominal injury or injuries sustained from the sides which are associated with thoracic symptoms strongly suggest a diaphragmatic injury. Nevertheless, many patients have no sign of diaphragmatic injury other than the entry hole, which makes the diagnosis only a possibility until the time of exploration. Diaphragmatic injury may be missed altogether when there exists no other indication for exploration for other injuries. The latter condition typically occurs following sharp object injuries since gunshot injuries usually necessitate abdominal and thoracic exploration [16,17].
Diaphragm moves between fourth and eighth ribs with deep expiration and inspiration. Hence, sharp object or gunshot injuries to this region absolutely necessitate the exclusion of diaphragmatic injury. Otherwise, small defects may give rise to serious complications in the long term [18,19].
Sharp object or gunshot injuries affecting diaphragmatic region may form smaller defects. Sharp object injuries tend to have a silent initial course but they also have potential to cause serious complications in the long term, because intraabdominal organs may migrate to thoracic cavity due to a pressure gradient between the positive-pressure abdomen and the negativepressure thorax, which may lead to colonic, gastric, splenic, and even omental necrosis in the long term [14,18]. This suggests the importance of thoracoscopy and/or laparoscopy.
Miller et al. [20] reported a study on penetrating diaphragmatic injuries affecting 94 patients. They showed that 43% of their patients had normal findings on chest films. Abnormalities noted on chest films may include hemothorax, pneumothorax, hemopneumothorax, abdominal organ herniation, and pneumoperitoneum. A study revealed that radiograms were negative among 1/3 of 185 patients [16]. Many series published so far have reported that the initial radiological tests produced normal findings in 30-50% of cases, and thus stressed the importance of repeat radiological tests [21,22]. We obtained two-sided chest films and CT for all cases except for those operated on an emergent basis.
Diaphragmatic injury should be suspected for all injuries affecting trunk, with the likelihood being especially raised for injuries from nipples to umbilicus. When there is no doubt about diaphragmatic injury or organ injury, exploration is not essential at the acute stage. However, diaphragmatic tears may be missed after some sharp object injuries [23].
Persistently abnormal findings over the diaphragmatic region or left lower lobe on chest film may necessitate diagnostic laparoscopy or VATS [24,25]. Diagnostic laparoscopy or thoracoscopy should be preferred for penetrating left thoracoabdominal injuries.
Acute diaphragmatic injury may be characterized with shoulder pain, epigastric pain, vomiting, and superficial respiration, which facilitate diagnosis. However, smaller injuries may lack specific signs and symptoms. When strong suspicion remains despite all negative examinations and tests, thoracoscopy and/or laparoscopy should be performed in the same session because this strategy considerably lowers mortality and morbidity [19].
Diaphragmatic injuries, particularly the delayed ones, may cause death. Associated organ injuries cause death at variable rates. The mortality rate in the literature varies between 1% and 28% [13]. Other organ injuries due to multi-trauma are the cause of death in the acute setting whereas it is the pulmonary complications that cause death in delayed cases. In a 480-case series the mortality rate was found 12.5% [26]. While the corresponding figure in our series was 5%.
Symbas et al. [27] reported a mortality rate of 2.2% among 185 patients with penetrating diaphragmatic injuries. Nel and Warren [24] examined 55 patients with diaphragmatic injury using thoracoscopy and reported that the modality was 100% sensitive and 90% specific, and had an accuracy rate of 94%. Some other authors have later confirmed their findings [9,25]. All patients were appropriately managed within 24-48 h. Three cases that remained undiagnosed despite all efforts but still had suspicious signs and symptoms were examined with diagnostic thoracoscopy and diagnosed with diaphragmatic rupture, which was primarily repaired.
Surgical approach to TDI varies by the location of an injury and operative duration. Laparoscopy or laparotomy offers the opportunity for providing the most rapid diaphragmatic repair following trauma. This approach facilitates a detailed intraabdominal examination and abdominal organ reduction [14,28,29].
When intrathoracic organ injury or major bleeding does not exist, an abdominal approach is preferred to detect an asymptomatic abdominal organ injury and to visualize both diaphragms. Thoracotomy does not allow the visualization of both diaphragms. VATS is as effective as laparoscopy for diagnosis and treatment of diaphragmatic injuries [10,30]. In our study, surgical intervention was performed using thoracotomy for cases without abdominal problems and with laparotomy for cases with concurrent abdominal injuries.
In acute injury, a non-absorbable (No. 0 or 1) suture should be used when diaphragmatic integrity is not disrupted. However, prosthetic mesh should be used to reinforce the defect when the latter is large or chronic [4,19].
Our study does have some limitations. First, this is a retrospective study, and cases cannot be randomized. Secondly, autopsy is not popular in our country due to custom. Therefore, we could not discover the missed diagnostic rate precisely.
Conclusion
TDI may be easily missed at the acute stage. The radiological appearance of herniated organs may be misdiagnosed as pneumothorax in delayed cases. Delayed traumatic TDI results in high morbidity and mortality. Therefore, in trauma patients, particularly those with lower chest and upper abdominal involvement, it is necessary remember the possibility of TDI, to re-assess patients with radiological diagnostic methods, not to spare thoracoscopy, and to carefully examine diaphragm during laparotomy and thoracotomy performed for other lesions.
Conflicts of Benefits
The authors have stated that in the preparation and publication of this article there are not any benefit conflicts.
Financial Support
The authors have not received any financial support for the processes of research and authorship involved in this study.
References
- Thiam O, Konate I, Gueye ML, Toure AO, Seck M, Cisse M. Traumatic diaphragmatic injuries: epidemiological, diagnostic and therapeutic aspects. Springer Plus 2016; 5: 1614.
- Bosanquet D, Farboud A, Luckraz H. A review diaphragmatic injury. Respir Med CME 2009; 2: 1-6.
- Al-Koudmani I, Darwish B, Al-Kateb K, Taifour Y. Chest trauma experience over eleven-year period at al-mouassat university teaching hospital-Damascus: a retrospective review of 888 cases. J Cardiothorac Surg 2012; 7: 35.
- Ercan M, Aziret M, Karaman K, Bostancab B, Akoaylu M. Dual mesh repair for a large diaphragmatic hernia defect: An unusual case report. Int J Surg Case Rep 2016; 28: 266-269.
- Marzona F, Parri N, Nocerino A, Giacalone M, Valentini E. Traumatic diaphragmatic rupture in pediatric age: review of the literature. Eur J Trauma Emerg Surg 2016.
- Turhan K, Makay O, Cakan A, Samancilar O, Firat O. Traumatic diaphragmatic rupture: look to see. Eur J Cardiothorac Surg 2008; 33: 1082-1085.
- Lim BL, Teo LT, Chiu MT, Asinas-Tan ML, Seow E. Traumatic diaphragmatic injuries: a retrospective review of the 12-year experience at a tertiary trauma centre. Singapore Med J 2016; 1-16.
- Gmachowska A, Pacho R, Anysz-Grodzicka A, Bakon L, Gorycka M, Jakuczun W. The role of computed tomography in the diagnostics of diaphragmatic injury after blunt thoraco-abdominal trauma. Pol J Radiol 2016; 81: 522-528.
- Ghionzoli M, Bongini M, Piccolo RL, Martin A, Persano G. Role of thoracoscopy in traumatic diaphragmatic hernia. Pediatr Int 2016; 58: 601-603.
- Yucel T, Gonullu D, Matur R, Akinci H, Ozkan SG. Laparoscopic management of left thoracoabdominal stab wounds: a prospective study. Surg Laparosc Endosc Percutan Tech 2010; 20: 42-45.
- Fangbiao Z, Chunhui Z, Chun Z, Hongcan S, Xiangyan Z. Thoracotomy for Traumatic Diaphragmatic Hernia. Indian J Surg 2016; 78: 371-374.
- Icme F, Balkan E, Becel S, Kavakli HS, Yuzbasioglu Y, Sener A. Evaluation of the patients diagnosed with diaphragmatic rupture in emergency room. Turkish J Thorac Cardiovasc Surg 2013; 21: 712-717.
- Dwivedi S, Banode P, Gharde P, Bhatt M, Ratanlal Johrapurkar S. Treating traumatic injuries of the diaphragm. J Emerg Trauma Shock 2010; 3: 173-176.
- Limmer KK, Kernstine KH, Granish FW, Weiss LM. Diaframanin malign veya benign hastaliklari. Nobel Tip Kitaplari. Istanbul 2011; 127: 1054-1067.
- Sanli M, Isik AF, Tuncozgur B, Meteroglu F, Elbeyli L. Diagnosis that should be remembered during evaluation of trauma patients: diaphragmatic rupture. Ulus Travma Acil Cerrahi Derg 2009; 15: 71-76.
- Symbas PN. Diaphragmatic injuries. General Thoracic Surgery (6th edn.). Lippincott Williams and Wilkins, Philadelphia, USA 2005; 1006-1014.
- Allan Z, Peng C, Chandra R. Traumatic diaphragmatic rupture with underlying lung laceration and tension pneumoperitoneum. J Surg Case Rep 2017; 2017: 120.
- Chatzoulis G, Papachristos IC, Daliakopoulos SI, Chatzoulis K, Lampridis S, Svarnas G. Septic shock with tension fecothorax as a delayed presentation of a gunshot diaphragmatic rupture. J Thorac Dis 2013; 5: 195-198.
- Hanna WC, Ferri LE. Acute traumatic diaphragmatic injury. Thorac Surg Clin 2009; 19: 485-489.
- Miller L, Bennett EV, Root HD, Trinkle JK, Grover FL. Management of penetrating and blunt diaphragmatic injury. J Trauma 1984; 24: 403-409.
- Sehitogullari A, Sayir F, Kahraman A, Oncu R, Soyoral L. Traumatic injuries of the diaphragm. Dicle Med J 2012; 39: 257-261.
- Okur MH, Uygun I, Arslan MS, Aydogdu B, Turkoglu A. Traumatic diaphragmatic rupture in children. J Pediatr Surg 2014; 49: 420-423.
- Sazaer EM, Ok E, Avayaroayullari L, Kaak C, Kerek M. Traumatic diaphragmatic ruptures. Ulus Travma Derg 2001; 7: 176-180.
- Nel JH, Warren BL. Thoracoscopic evaluation of the diaphragm in patients with knife wounds of the left lower chest. Br J Surg 1994; 81: 713-714.
- Freeman RK, Al-Dossari G, Hutcheson KA, Huber L, Jessen ME, Meyer DM. Indications for using video-assisted thoracoscopic surgery to diagnose diaphragmatic injuries after penetrating chest trauma. Ann Thorac Surg 2001; 72: 342-347.
- Simpson J, Lobo DN, Shah AB, Rowlands BJ. Traumatic diaphragmatic rupture: associated injuries and outcome. Ann R Coll Surg Engl 2000; 82: 97-100.
- Symbas PN, Vlasis SE, Hatcher C. Blunt and penetrating diaphragmatic injuries with or without herniation of organs into the chest. Ann Thorac Surg 1986; 42: 158-162.
- Smith RS, Fry WR, Tsoi EK, Morabito DJ, Koehler RH. Preliminary report on videothoracoscopy in the evaluation and treatment of thoracic injury. Am J Surg 1993; 166: 690-693.
- Martinez M, Briz JE, Carillo EH. Video thoracoscopy expedites the diagnosis and treatment of penetrating diaphragmatic injuries. Surg Endosc 2001; 15: 28-33.
- Yoo DG, Kim CW, Park CB, Ahn JH. Traumatic right diaphragmatic rupture combined with avulsion of the right kidney and herniation of the liver into the thorax. Korean J Thorac Cardiovasc Surg 2011; 44: 76-79.