Case Report - Journal of Clinical Ophthalmology (2022) Volume 6, Issue 2
Traumatic phacocele: Case report and its peculiarities.
Gabriel Castilho Sandoval Barbosa1*, Thiago José Muniz Machado Mazzeo1, Allan Gomes da Silva1, Luciano Fuzzato Filho1, Rafael Garcia1, Cleide Guimarães Machado1,2, André Marcelo Vieira Gomes1,2
1Department of Ophthalmology, Suel Abujamra Institute, São Paulo, SP, Brazil
2Department of Ophthalmology, University of São Paulo, São Paulo, SP, Brazil
- Dr. Gabriel Castilho Sandoval Barbosa
Department of Vitreous and Retina,
Suel Abujamra Institute,
Sao Paulo,
Brazil
E-mail: gabrielcastilho66@gmail.com
Received: 01-Mar-2022, Manuscript No. AACOVS-22-58620; Editor assigned: 04-Mar-2022, PreQC No. AACOVS-22-58620 (PQ); Reviewed: 18-Mar-2022, QC No. AACOVS-22-58620; Revised: 23-Mar-2022, Manuscript No. AACOVS-22-58620 (R); Published: 01-Apr-2022, DOI: 10.35841/aacovs.6.2.530-532.
Citation: Farvardin M, Johari MK, Nami M, et al. Annular choroidal detachment one year after argus-II retinal prosthes is implantation. Ophthalmol Case Rep. 2020;4(1):23-25.
Abstract
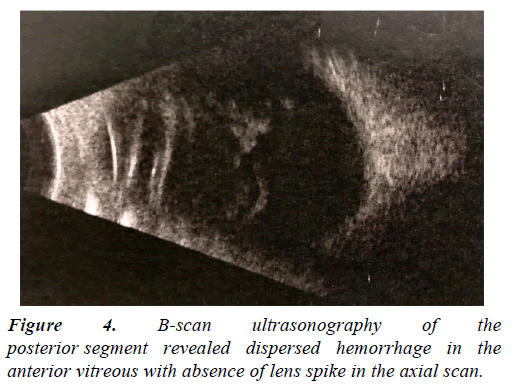
Subconjunctival dislocation of the crystalline lens is known as phacocele. Most cases of phacocele are associated with blunt trauma, the existence of scleral rigidity, hard crystalline lens, and history of scleral surgery. We report a case of a 45-year-old man who had been through an ocular blunt trauma with an iron bar, and consequent traumatic phacocele with a scleral defect. B-scan ultrasonography of the posterior segment revealed absence of lens spike in the axial scan, confirming the diagnosis. Successfully explorative surgery with pars plana vitrectomy was performed under retrobulbar anesthesia, and the eye was left primarily aphakic for better surgical preparation in a second approach.
Keywords
Blunt trauma, Phacocele, Pars plana vitrectomy.
Introduction
Posttraumatic dislocation of the crystalline lens into the subconjunctival space, also known as phacocele, is a rare entity resulting from indirect scleral rupture of the globe. Perforation cases that occur as a result of ocular trauma are among the emergencies of ophthalmology and are a condition that must be promptly and carefully conducted [1]. The presence of intense subconjunctival hemorrhage and hypotonia should suggest an occult perforation. B-scan Ultrasonography plays a key role in diagnosis, especially in cases with hyphema or vitreous hemorrhage. The lens echoes are absent, and the scan also aids in detecting vitreous hemorrhages, retinal detachments, suprachoroidal hemorrhages, and endophthalmitis [2].
This report brings illustrative information regarding a case of phacocele and its outcome, besides highlighting an interesting issue in this condition: Primary versus secondary implantation of the intraocular lens (IOL).
Case Presentation
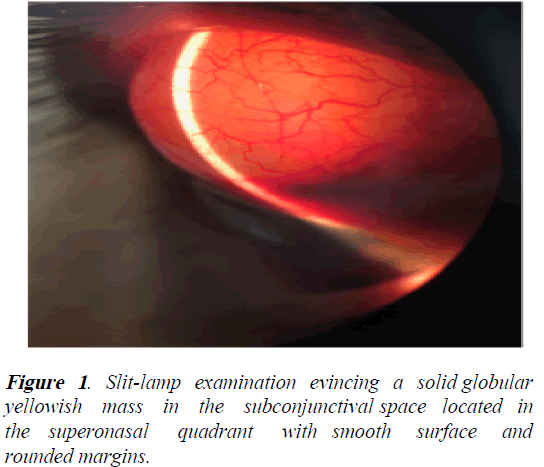
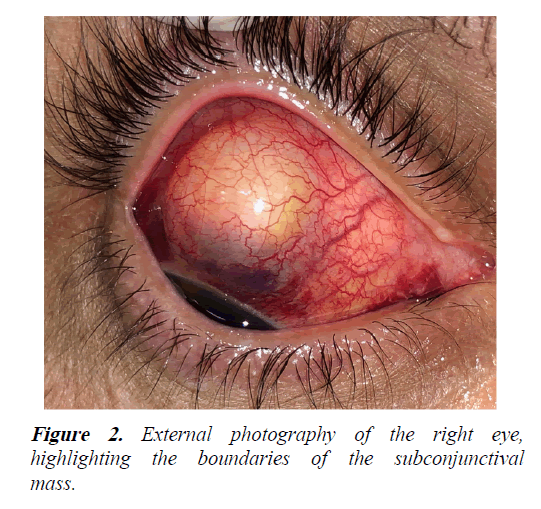
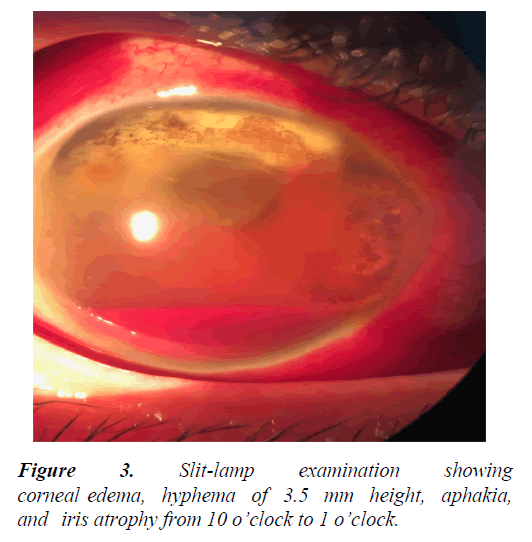
A 45-year-old man was referred to our institution 10 days after blunt trauma by an iron bar to the right eye. The patient presented with pain in the right eye, vision loss, and headache. There was no history of eye surgery, but the patient reports a history of blunt trauma with a soccer ball at age 13, accompanied by persistent visual impairment. At presentation, his right vision was light perception. On slit-lamp examination of the affected eye, there was a solid globular yellowish mass in the subconjunctival space located in the superonasal quadrant with a smooth surface and rounded margins (Figures 1 and 2). The anterior chamber details were poorly visualized due to cornea edema and a hyphema of 3.5 mm height (Figure 3). Aphakia and iris atrophy from 10 o’clock to 1 o’clock was present. The intraocular pressure (IOP) was 17 mmHg. There was no relative afferent pupillary defect in the affected eye. Bscan ultrasonography of the posterior segment revealed dispersed hemorrhage in the anterior vitreous with absence of lens spike in the axial scan (Figure 4). The diagnosis of traumatic phacocele was made.
Explorative surgery was performed under retrobulbar anesthesia. A 360° conjunctival peritomy was performed, and the lens with an intact capsule was removed from the subconjunctival space. There was a 7.0 mm superior scleral wound with uveal tissue remnant. Human scleral graft was prepared, but due to the linear and regular wound, it was not necessary for the surgery. A standard 3 port pars plana vitrectomy was performed followed by a scleral introflexion to relieve potential residual tractions in the wound site. During the vitrectomy, multiples scar fibrosis with hyperpigmented grayish lesions and well-defined boundaries were identifiedalong the retina. The eye was left primarily aphakic for better surgical preparation in a second approach.
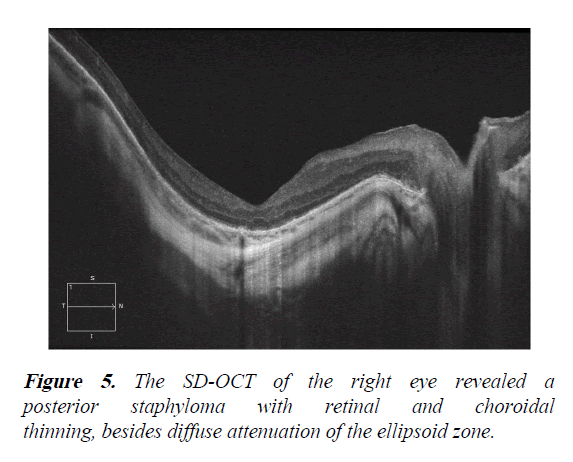
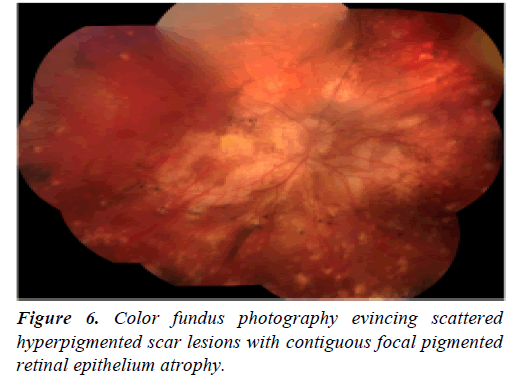
At 1-month follow-up, the Best-Corrected Visual Acuity (BCVA) of the right eye was 20/60 (+7,00 D Sph -2,50 D Cyl X70). The SD-OCT of the right eye revealed a posterior staphyloma with retinal and choroidal thinning, besides diffuse attenuation of the ellipsoid zone (Figure 5). Color fundus photography evinced scattered hyperpigmented scar lesions with contiguous focal pigmented retinal epithelium atrophy (Figure 6) suggestive of inactive idiopathic multifocal choroiditis, which was not related to the current trauma condition.
Results and Discussion
A phacocele is the dislocation of an intact crystalline lens into the subconjunctival space secondary to blunt trauma, resulting in scleral rupture. The superonasal quadrant near the limbus is the most common location of phacocele, because of projection of energy caused by the impact in the temporal region. The second most common site is superotemporal. The scleral rupture frequently occurs between the limbus and spiral of Tillaux [3,4]. It is seen more commonly in elderly people with rigid sclera rather than in children with elastic ocular tissues. Predisposing factors include previous surgical or traumatic scleral scar, recurrent episodes of scleritis, and others. Vitreous hemorrhage and retinal detachments may accompany these cases [5,6].
The primary goal in the management of a phacocele is the extraction of the displaced lens and maintenance of globe integrity [7,8]. Infusion port placement is advisable as the first approach in the surgery to avoid eye collapse when manipulating the lens near the open injury in the sclera, and then, the wound should be explored. Repair of scleral rupture if necessary, partial vitrectomy should be performed. A scleral introflexion to relieve potential residual tractions is advisable, as the treatment of the vitreous base is tricky in these cases. As in this particular case, Intraocular Lens (IOL) implantation can be left to a later session depending on the situation of the eye.
Cohen reported that primary IOL implantation, with the calculation of the IOL power using biometry measurements from the contralateral non-traumatic eye, may result in significant difference refraction of 4 dioptres. After a new approach of IOL exchange surgery using simulated keratometry and axial length measurements of the injured eye to calculate the IOL power, the patient reached emmetropia with BCVA of 20/20.8 On the other hand, Chuang and Lai emphasised that using the biometry of the injured eye after primary repair of the globe was more accurate than using biometry of the nontraumatic eye to determine the IOL power with refraction deviation of only 1 dioptre in secondary IOL implantation [9]. Further, timely and effective intervention can ensure good visual recovery.
Conclusion
In the case herein reported, the history of blunt trauma in youth may have acted as a facilitating factor of the scleral rupture after a new blunt trauma, which in turn led to the patient's current condition. Unfortunately, the patient had sequelae from previous ocular trauma, with retinal repercussions and visual impairment. The main goal of surgery was the maintenance of globe integrity so that a subsequent approach, with an optimized calculation of the IOL power, takes place with the best possible scenario.
Acknowledgment
None.
Conflict of Interest
None.
Funding Sources
None.
Data Availability Statement
The authors are responsible for the data described in the manuscript and assure full availability of the study material.
References
- Can HY, Koru M, Karahan E. A traumatic phacocele after blunt trauma: A case report. J Med Cases Updat. 2021;1:10-11.
- Neupane S, Das D, Korgaonkar S. Migrated subconjunctival crystalline lens: A traumatic phacocele. BMJ Case Rep. 2020;13:e237014
[Cross Ref] [Google Scholar] [Pub Med]
- Allen RC, Gupta RR, Poblete R, et al. Traumatic phacocele. J Cataract Refract Surg. 2001; 27:1333-4.
- Manavi SD, Deepesh M. A rare case of traumatic posterior phacocele with retinal detachment. Indian J Ophthalmol. 2016; 64:89-90.
[Cross Ref] [Google Scholar] [Pub Med]
- Bhattacharjee K, Bhattacharjee H, Deka A, et al. Traumatic phacocele: Review of eight cases. Indian J Ophthalmol. 2007; 55:466-8.
[Cross Ref] [Google Scholar] [Pub Med]
- Santos-Bueso E, Sáenz-Francés F, Díaz-Valle D, et al. Ocular rupture associated with lens dislocation to the subconjunctival space. Arch Soc Esp Oftalmol. 2007; 82:641-4.
[Cross Ref] [Google Scholar] [Pub Med]
- Sathish S, Chakrabarti A, Prajna V. Traumatic subconjunctival dislocation of the crystalline lens and its surgical management. Ophthalmic Surg Lasers. 1999; 30:684-6.
[Cross Ref] [Google Scholar] [Pub Med]
- Cohen KL. Inaccuracy of intraocular lens power calculation after traumatic corneal laceration and cataract. J Cataract Refract Surg. 2001;27:1519-22.
[Cross Ref] [Google Scholar] [Pub Med]
- Chuang LH, Lai CC. Secondary intraocular lens implantation of traumatic cataract in open-globe injury. Can J Ophthalmol. 2005; 40:454-9.
[Cross Ref] [Google Scholar] [Pub Med]