Case Report - Ophthalmology Case Reports (2020) Volume 4, Issue 1
Traumatic cataract in young
Rishi Sharma1*, BV Rao1 and Rakesh Maggon21Military Hospital Yol, Himachal Pradesh, India
2Department of Ophthalmology, Command Hospital (WC), Chandigarh
- Corresponding Author:
- Rishi Sharma
Military Hospital Yol
Himachal Pradesh
India
E-mail: rs19april81@gmail.com
Accepted date: April 10, 2020
Citation: Sharma R, Rao BV, Maggon R. Traumatic cataract in young. Ophthalmol Case Rep. 2020;4(1):38-40.
Abstract
A 27-year-old male patient presented with a history of trauma in the left eye one month back sustained with a pin of a rifle while cleaning weapons in his unit. Post-injury, he developed pain, redness, and diminution of vision in the eye. Vision at presentation was 6/6 unaided in the right eye and 6/24 in the left eye with no further improvement. Lids and adnexa were normal with no retained foreign body in both eyes. The right eye anterior segment and fundus evaluation were normal. The left eye had clear cornea, no cells, and flare in AC, no hyphema. Pupillary reactions were normal and no iris sphincter tear was seen. Rosette shaped cataract was seen. The fundus examination was normal. Phacoemulsification with Intraocular lens implantation was done. Post-operative day vision was 6/6 unaided, clear cornea, mild AC reaction normal reacting pupil with well-centered IOL in the capsular bag. IOP was 16 and 19 mm Hg. The patient was placed on topical antibiotic-steroid eye drops and is kept on regular follow-up.
Keywords
Rosette cataract, Closed globe injury, Irrigation/Aspiration.
Introduction
The incidence of ocular trauma is relatively common despite the anatomic and functional protective mechanisms of the visual system. It occurs most frequently in men and young people [1]. World Health Organization estimated that up to 55 million eye injuries occur annually worldwide and approximately 1.6 million people lose their vision due to eye trauma [2]. Several guidelines for ocular trauma have been published to help determine the visual prognosis [3]. The visual outcome generally depends on the initial visual acuity, pupillary reflex response, and severity of the trauma [4]. In this article, we will focus on the presentation and management of injury to the lens and, in particular, traumatic cataracts.
Case Report
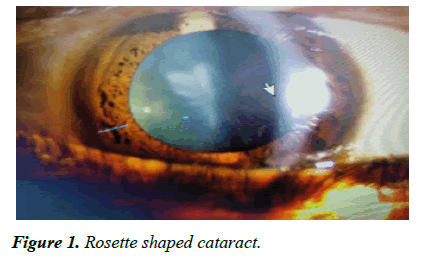
A 27-year-old male patient presented with a history of trauma in the left eye one month back sustained with a pin of a rifle while cleaning weapons in his unit. Post-injury, he developed pain, redness, and diminution of vision in the eye. Vision at presentation was 6/6 unaided in the right eye and 6/24 in the left eye with no further improvement. Lids and adnexa were normal with no retained foreign body in both eyes. The right eye anterior segment and fundus evaluation were normal. The left eye had clear cornea, no cells, and flare in AC, no hyphema. Pupillary reactions were normal and no iris sphincter tear was seen. Rosette shaped cataract was seen (Figure 1). There was no lens subluxation/zonular dialysis/phacodonesis. The fundus examination was normal. Ultrasonography B-Scan of both eyes was normal. IOP was 16 mm Hg (RE) and 18 mm Hg(LE) with applanation tonometry.
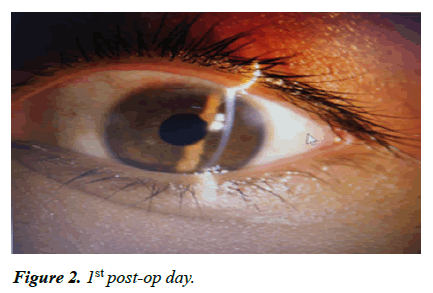
The individual was taken up for cataract surgery. Bimanual I/A was used for removal followed by Intraocular lens implantation. Postoperative day #1 vision (Figure 2) was 6/6 unaided, clear cornea, mild AC reaction normal reacting pupil with well-centered IOL in the capsular bag. IOP was 14 mm Hg and 16 mm Hg. The patient was placed on topical antibiotic and steroid eye drops. Postoperative week #1 his vision was 6/5. He has been kept on regular follow-up. Last check-up(after 01 months) revealed the vision of 6/5 unaided in the left eye, clear cornea, quiet AC, and well centered IOL in the capsular bag. Fundus-normal IOP-13 mm Hg and 14 mm Hg with applanation tonometry. Gonioscopy revealed open angles grade 4 with no signs of angle recession in both eyes. The steroid antibiotic drops were tapered off as per the standard regime followed. The patient has been counseled and advised to report immediately in case of pain, redness, diminution of vision, floaters, and flashes in the operated eye. On follow-up visual acuity, IOP recording, recording, detailed slit lamp biomicroscopy to rule out any uveitis, intraocular lens decentration, synechiae, pupillary capture, and posterior capsular opacification were done. Posterior segment evaluation was done with indirect ophthalmoscopy and it was normal.
Discussion
Blunt or penetrating ocular trauma resulting in traumatic cataract needs special consideration because of associated injury to ocular and periorbital structures. Surgery of traumatic cataracts can be primary or secondary. Primary cataract removal is suggested if the lens is fragmentized or, swollen causing a pupillary block or to examine the posterior segment blocked by lens opacity. Secondary cataract removal is more beneficial because of improved visibility, proper intraocular lens calculation, and fewer chances of postoperative inflammation [5].
The morphology of traumatic cataracts plays an important role in determining the appropriate surgical technique and the final visual outcome [6]. In this case, the cataract was Rosette shaped (Figure 1) with no associated injury to the surrounding ocular structures and therefore, we used I/A Cannula to aspirate the lens after good hydrodissection. This aligns with the study done by Shah MA et al. [7]. They stated that the surgical technique should be selected according to morphology and the condition of tissues other than the lens. They advocated the use of Phacoemulsification to operate on cataracts with hard and large nuclei. In a lens with white, soft or rosette type of cataract, bimanual/co-axial I/Awas used. Membranectomy and vitrectomy, via anterior /pars plana route, was used, in membranous cataract. Implantation of intraocular lens (IOL) in traumatized eyes after removal of traumatic cataract depends on the availability of capsular support. Capsular bag or sulcus fixation is preferred if there is sufficient capsular and Zonular support. Patients with insufficient capsular or Zonular support are the candidates for Artisan lenses, scleral fixation IOLS (SFIOLs) and anterior chamber IOLS (ACIOLs). One must assess and consider the capsular bag’s long term stability for intra-capsular fixation of the IOL [8-10]. In this case, the capsule and the bag were intact, therefore IOL was placed in the capsular bag.
Post-operative inflammation is a common complication following traumatic cataract and hampers visual outcome. Other complications leading to decreased post-operative vision are corneal scar, uveitis, secondary glaucoma, pupillary capture, posterior capsular opacification and retinal scar [11]. The major postoperative complications encountered on the first postoperative day are severe uveitis which response to medical therapy. Cheema and coworkers reported that the fibrinous uveitis was the most common postoperative complication (25%) [12]. It may be mainly due to surgical trauma in an already traumatized eye and not related to the type or location of IOL inside the eye. The commonest late post-operative complication in these traumatic cataractous eyes is posterior capsular opacification seen at 6 months postoperatively. Eckstein and colleagues reported that posterior capsular opacity was seen in almost 92% [13].
The patient has been kept on follow-up for early diagnosis and management of these complications including cystoid macular edema which may warrant an OCT in case of diminution of vision.
Conclusion
Traumatic cataract resulting from ocular trauma is a common cause of ocular morbidity, especially in the young population. Management of traumatic cataract for good visual outcomes requires a holistic approach consisting of meticulous pre-op evaluation, uneventful surgery, and post-op follow-up to evaluate and manage any delayed complications which could hinder the post-op recovery of vision.
Conflicts of Interest
None.
References
- Serna-Ojeda JC, Cordova-Cervantes J, Lopez-Salas M, et al. Management of traumatic cataract in adults at a reference center in Mexico City. IntOphthalmol. 2015;35(4):451-8.
- Négrel AD, Thylefors B. The global impact of eye injuries. Ophthalmic Epidemiol. 1998;5(3):143-169.
- Kuhn F, Morris R, Witherspoon CD, et al. The Birmingham eye trauma terminology system (BETT). J Fr Ophtalmol. 2004;27(2):206-10.
- Mian ST, Azar DT, Colby K. Managment of traumatic cataracts. Int Ophthalmol Clin. 2002;42:23-31.
- Kuhn F, Pieramici DJ. Ocular trauma: principles and practice. New York (NY): Thieme. 2002.
- Mehul AS, Shreya MS, Shashank BS, et al. Effect of interval between time of injury and timing of intervention on final visual outcome in cases of traumatic cataract. Eur J Ophthalmol. 2011;21:760-5.
- Shah MA, Shah SM, Shah S, et al. Morphology of traumatic cataract: does it play a role in final visual outcome? BMJ Open. 2011;1:e000060.
- Sminia ML, Odenthal MT, Wenniger-Prick LJ, et al. Traumatic paediatric cataract: a decade of follow-up after artisan aphakia intraocular lens implantation. JAAPOS. 2007;11:555-8.
- Buckley EG. Hanging by a thread: The long-term efficacy and safety of transscleraltrans scleral sutured intraocular lenses in children (an American Ophthalmological Society thesis). Trans Am Ophthalmol Soc. 2007;105:294-311.
- Bekibele CO, Fasina O. Visual outcome of traumatic cataract surgery in Ibadan, Nigeria. Niger J Clin Pract. 2008;11(4):372-5.
- Mohammadpour M, Jafarinasab MR, Javadi MA. Outcomes of acute postoperative inflammation after cataract surgery. Eur J Ophthalmol. 2007;17(1):20-8.
- Cheema RA, Lukran AD. Visual recovery in unilateral traumatic paediatric cataracts related with posterior chamber intraocular lens and anterior vitrectomy in Pakistan. Int Ophthalmol. 1999;23:85-9.
- Eckstein M, Vijaya Lakshmi P, Kelladar M, et al. Use of intraocular lens in children with traumatic cataract in South India. Br J Ophthalmol. 1998;82:911-5.