Research Article - Biomedical Research (2017) Volume 28, Issue 16
Translation and initial psychometric evaluation of the Chinese version of the partners in health scale
Zhang Xiaofei1,2, Feng Hui1, Sharon Lawn3, Sun Mei1, David Smith3, Wang Jingxia1, Ren Lu1, Chen Jiarui1 and Tang Siyuan1*
1Xiang Ya Nursing School, Central South University, Changsha, Hunan Province, PR China
2The Second Hospital of Hebei Medical University, Shijiazhuang, Hebei Province, PR China
3Flinders Human Behaviour and Health Research Unit, Flinders University, GPO Box 2100, Adelaide, SA, Australia
- *Corresponding Author:
- Tang Siyuan
Xiang Ya Nursing School
Central South University, Changsha
Hunan Province, PR China
Accepted date: August 03, 2017
Abstract
This study aimed to translate the Partner in Health (PIH) scale (12 items) into the mandarin Chinese language and investigate the psychometric properties of the Chinese version PIH scale in patients with chronic diseases in primary care settings in Changsha, China. The instrument was translated according to the Sousa guideline including the following steps: Forward translation, back translation, expert panel evaluation and pilot study, with achievement of consensus at each step. Psychometric properties of the Chinese version PIH were assessed in a random sample of 300 community-dwelling patients with chronic diseases in Changsha, China. These properties included content validity, internal consistency, test-retest reliability and structural validity. Survey response rate was 93.7%. The results showed that the Chinese PIH scale had satisfactory reliability and validity. The test-retest reliability was 0.832 and the Cronbach’s coefficient was 0.865. The content validity rate (S-CVI/Ave) was 0.965. The correlation between the Patient Activation Measure (PAM) and the PIH was 0.505 (p<0.001). Results of the confirmatory factor analysis suggest that the PIH scale consisted of four factors: knowledge, partnership, management and coping. The Chinese PIH scale yields high reliability and validity. It can be used as a generic self-rated tool to assess self-management of patients with chronic diseases in China.
Keywords
Self-management, Patient self-report, Psychometric evaluation, Chronic disease.
Introduction
Along with the aged population and increasing lifestyle risk factors, the prevalence of chronic diseases is gradually rising in China. It has been reported that the incidence of hypertension and diabetes mellitus were 25.2% and 9.7% in Chinese adults in 2012 and were on the rise compared with the statistics figures in 2002. The incidence of malignant tumors in 2012 was 235 per 100,000 which were also on the increase during the same period [1]. Chronic diseases have become the biggest health threat and the major burden of diseases in China. The mortality caused by chronic diseases was 533 per 100,000, accounting for 86.6% of overall mortality rate in 2012.
The Chronic Care model offers a framework for the health care system to effectively deal with the needs and concerns of individuals with chronic diseases and it is widely acknowledged that self-management by the patient is integral to good chronic disease care [2,3]. Besides, accumulated evidence has shown that effective self-management support and interventions by service providers improve health outcomes of patients with chronic disease, enhance patient’s quality of life, and reduce health service utilization [4]. China’s government, also recognizing the importance of selfmanagement, enacted the relevant policy to integrate selfmanagement into chronic disease management routine practice in 2010.
There is no agreed definition of self-management in the world though it is generally understood to include a focus on the person’s knowledge and behaviours, and how they manage the physical, social and emotional impacts of chronic disease on their everyday life, health and wellbeing [5-7]. Accordingly, scales to measure chronic disease self-management cannot be unified. Besides, scales appear to vary with different kinds of chronic diseases. In mainland China, self-management assessment scales are mainly disease-specific, such as scales to measure haemodialysis, liver transplant, hypertension, and diabetes mellitus [8]. The content of the scales is highly relevant to the disease which means the scale is only used in the disease-specific population. However, most patients with chronic disease, especially community-dwelling elders, have more than two types of chronic diseases, so a valid and reliable generic self-management assessment scale is needed in order to help professionals to determine individuals’ self-management abilities in a more holistic way, to provide targeted selfmanagement interventions and to monitor patient’s behaviour changes over time [9].
The Partner in Health (PIH) scale is a generic tool, developed by chronic disease management experts in Australia that has been psychometrically validated and used with several population groups and within various contexts to assess objectively a patient’s self-management knowledge and behaviours [10]. The development of the scale is based on the seven Australian nationally agreed principles of selfmanagement [11]:
1. Knowing about the condition and/or its management.
2. Adopting an agreed self-management care plan negotiated in partnership with health professionals, significant others and/or carers and other supporters.
3. Actively sharing in decision-making with health professionals, significant others and/or carers and other supporters.
4. Monitoring and managing signs and symptoms of the condition.
5. Managing the impact of the conditions on the physical, emotional, occupational and social functioning.
6. Adopting lifestyles that address risk factors and promote health by focusing on prevention and early intervention.
7. Having access to, and confidence in the ability to use support services.
The PIH scale has been tested and refined in clinical practice and research pilots and trials in many countries, such as Australia, Canada, New Zealand, USA, UK and the Netherlands [12-21]. It has been translated into Spanish, Dutch, German, Finnish, Swedish, Malaysian and Korea [22,23]. These studies have supported it to be an appropriate outcome measurement tool to evaluate chronic disease selfmanagement interventions. The updated scale has 12 items with good internal consistency and validity [24].
The aim of the study was to translate the PIH scale into Chinese, and test its reliability and structural validity.
Methods
Design
A cross-sectional survey of Chinese community dwelling patients with chronic diseases was conducted to evaluate the psychometric properties of the Chinese version of the PIH Scale. Subjects were recruited in the community health centers in Changsha, China during November and December 2015. There were five districts in Changsha city from which we randomly selected one community health center from each district, and then 60 patients with chronic diseases were randomly chosen from each health center.
Ethical considerations
Permissions were obtained from the authors and copyright owners of the original scale. The study was approved by the Ethics Committee of Xiangya School of Nursing, Central South University in China. All patients involved in the study provided informed, signed consent prior to their participation.
Translation procedures
The translation and validation of the scale strictly followed the Sousa guideline [25].
Step 1: Forward translation: Two bilingual translators (mother tongue for both was Chinese: one was a nursing doctoral student, the other was a non-medical master’s student) translated the PIH scale and compared the two versions, respectively. Then the two Chinese versions were sent to the translation panel (including two bilingual experts, two Chinese experts, two experts in chronic diseases). They compared the Chinese version with the English version until all (including two bilingual translators) reached agreement.
Step 2: Backward translation: Two different bilingual translators who had not seen the PIH scale (both were studying abroad and fluent in English: one was a master nursing student, the other was a non-medical student) translated the Chinese version back into English. Then they compared the translated English version with the original English version. Step 1 and step 2 were repeated until the translated English version accorded with the original English version.
Step 3: Cultural adaption: The pre-final Chinese version was sent to the expert panel (five chronic disease experts, two chronic disease educational experts) to evaluate the item’s relevance and clarity and scoring criteria. The score for each item was from 1 (not at all related) to 4 (totally related). At the same time, we chose 10 patients with chronic diseases to check the scale’s readability, simplicity and acceptability. Finally, we got the final Chinese version and sent the final translated English version to the original scale developers in Australia, for their final advice, in preparation for the fourth step of pilot testing.
Study setting and sample selection
Inclusion criteria: Patients with diagnosed diabetes mellitus, hypertension or both; those who knew the diagnosis; nonhospitalized patients; those without severe physical or mental diseases; aged>18 y old; those who could communicate in Chinese; those signed the informed consents. The reason why we chose diabetes or hypertension was that these two types of diseases are routinely managed by Chinese community health centers.
Patients visiting the health centers during the research period were identified by the health providers at the health centers on the basis of the inclusion criteria. Then the researchers selected target subjects according to the last number of their patient ID, and provided them with information about the study and invited their participation.
Instruments
Chinese partners in health scale (PIH): There are several PIH editions available, such as a 11-item version a 12-item 2010 version, and a 12-item 2015 version which we chose to adapt [10,24,26]. The 12-item 2015 version has been validated in a representative Australian community survey, and the response categories for items 1-4, 6, 8, 10, 11 and 12 ranged from 0 (very good) to 8 (very poor); and for items 5, 7, and 9 from 0 (always) to 8 (never). Factor analyses revealed four related constructs of chronic disease self-management that were in line with previous PIH research. The four factors were knowledge (items 1 and 2), partnership (items 3, 4, 5 and 6), management (items 7 and 8) and coping (items 9, 10, 11 and 12). We chose this most recent version because of the rigor of its psychometric validation process. The Chinese PIH scale is a 12-item, self-report scale developed to measure chronic disease patient’s self-management knowledge and behaviours, with responses scored on a 9-point Likert scale ranging from 0 to 8 where 0 represents low self-management and 8 represents high self-management. The possible total score was between 0 and 96 across all 12 questions, or between 0 and 8 for each question (average of the total score). A higher total score indicates patients with better self-management knowledge and behaviours.
The Chinese patient activation measure (Chinese PAM): The PAM scale was originally developed by Hibbard with 22 items and a shortened version with 13-items was widely used [27,28]. The PAM scale assesses patient self-reported knowledge, skills and confidence for self-management of one’s health or chronic condition. It has a conceptual purpose to the PIH scale and researches have repeatedly shown that a higher score on the PAM is positively associated with specific selfcare and various health related behaviours. So we choose PAM as the scale to test the criterion validity of PIH scale. The Chinese PAM scale is a 13-item self-report scale, with four- Likert scoring from 1 (strongly disagree) to 4 (strongly agree), 0 (not applicable), the total raw score is between 0 and 52. The Chinese PAM has good reliability and validity, with Cronbach’s alpha of 0.81 [29].
Statistical analysis
SPSS software 19.0 was used for statistical analysis. Content validity for the Chinese PIH scale was assessed using an expert panel. Test-retest reliability was evaluated by calculating the intra-class correlation coefficient between pre-test and posttest, with a 10 d interval in a sample of 21 health professionals. To assess internal consistency, Cronbach’s alpha coefficients were calculated for PIH total items. Due to a clear hypothesis regarding PIH factor structure from a statistical and theoretical perspective, structural validity was evaluated by confirmatory factor analysis using Mplus software (version 7.4). Due to skewed item distributions and the Maximum Likelihood (ML) assumption of joint normality of all observed and latent variables, robust standard errors were used for estimation (MPlus estimator=MLR). Post-estimation modification indices were calculated to identify any omitted covariance paths that would otherwise improve model fit. To evaluate how well a 4- factor measurement model fitted the data, a range of postestimation tests were conducted. Likelihood Ratio (LR) test was used to compare each fitted model with degree of freedom versus a saturated model with no degree of freedom. At a practical level, goodness-of-fit indices were calculated to assess for any discrepancies between models implied data and observed data based on recommended criteria. These model fit indices were χ2/df ≤ 2, root mean square error of approximation (RMSEA<0.06), confirmatory fit index (CFI ≥ 0.95), Tucker-Lewis index (TLI ≥ 0.95), and standardized root mean squared residual (SRMR ≤ 0.08) [30]. In addition, criterion-related validity was tested using the correlation between the Chinese PAM and the PIH scale. A P value of less than 0.05 was considered as statistical significance.
Results
Translation and cultural adaptation
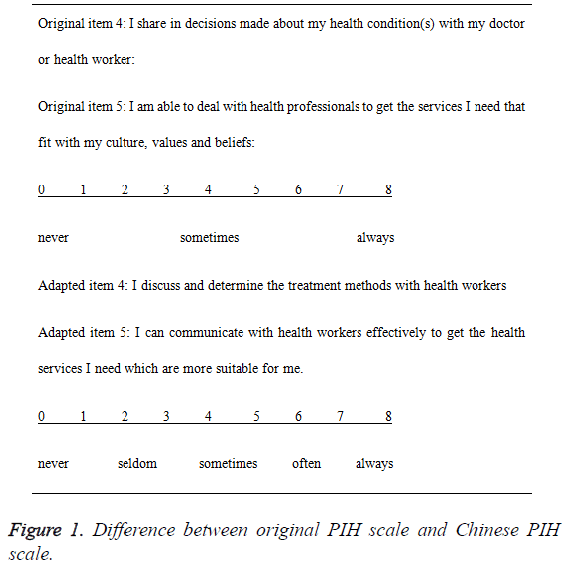
The original item scoring used a 0-8 Likert (nine-point) scale, with 0 indicating low self-management and 8 indicating high self-management. However, Chinese patients, especially elders, are not accustomed to the string scoring without enough annotation. In another words, only using descriptors of the anchor points (0 and 8) are inadequate for Chinese patients. Therefore, we added some annotation by dividing the nine scores into five grades (for example: “not very well, not well, not sure, well, very well”) to the original item scoring (Figure 1). A further concern was that the Chinese patients did not understand the meaning of original item 4 and item 5, so we adapted the two items greatly through subjects ‘feedback and experts’ recommendation then reached an agreement with the original developing group, and the two final items were “I discuss and determine the treatment methods with health workers” and “I can communicate with health workers effectively to get the health services I need which are more suitable for me” (Figure 1).
Baseline data
Among 300 subjects, a total of 281 subjects completed the survey with a response rate of 93.7%. All 281 patients were aged 61.4 ± 11.9 y, ranging from 22-85 y including 145 male and 136 female. Their baseline data are summarized in Table 1.
| Characteristics | Mean or N | SD or % |
|---|---|---|
| Age (Mean and SD) | 61.4 | 11.9 |
| Sex (N and %) | ||
| Male | 145 | 51.6 |
| Female | 136 | 48.4 |
| Marital status | ||
| Married | 244 | 86.8 |
| Other | 37 | 13.2 |
| Work status | ||
| Employed | 88 | 31.3 |
| Other | 193 | 68.7 |
| Education | ||
| Primary school or below | 84 | 29.9 |
| Junior high school | 91 | 32.4 |
| Senior high school or equivalent | 55 | 19.6 |
| College or above | 51 | 18.2 |
| Disease duration in years (Mean and SD) | 8.86 | 7.17 |
Table 1: Subject’s socio-demographic characteristics (n=281).
As illustrated in Table 2, the mean score of the total PIH scale was 4.62 (SD=1.005), and there were no floor and ceiling effects in the 12 items <20% of the respondents achieved the lowest or highest possible scores.
| n | M | SD | Floor (%) | Ceiling (%) | |
|---|---|---|---|---|---|
| Item 1 | 281 | 4.73 | 1.48 | 0.4 | 4.6 |
| Item 2 | 281 | 4.49 | 1.536 | 0.7 | 3.6 |
| Item 3 | 281 | 5.56 | 1.532 | 0.7 | 16.4 |
| Item 4 | 281 | 3.59 | 1.836 | 6.8 | 2.1 |
| Item 5 | 281 | 3.78 | 1.848 | 5 | 2.5 |
| Item 6 | 281 | 4.74 | 1.68 | 1.8 | 7.5 |
| Item 7 | 281 | 4.4 | 1.696 | 2.1 | 3.6 |
| Item 8 | 281 | 4.85 | 1.644 | 1.8 | 7.5 |
| Item 9 | 281 | 4.85 | 1.631 | 0.4 | 5.7 |
| Item 10 | 281 | 4.74 | 1.386 | 0.7 | 5 |
| Item 11 | 281 | 4.88 | 1.28 | 0.7 | 4.6 |
| Item 12 | 281 | 4.81 | 1.637 | 1.1 | 6.8 |
| Total score | 281 | 4.62 | 1.005 | 0 | 0.4 |
Table 2: Chinese version of the partners in health scale: means, standard deviations, and floor and ceiling effects.
Reliability
Test-retest reliability: Test-retest reliability was evaluated using the correlation coefficient. For the Chinese PIH scale, the correlation coefficient over a 10 d interval in a sample of 21 subjects was 0.832. For this test, a value of >0.61 indicates substantive test-retest reliability [31].
Internal consistency reliability: The inter-item correlations were all positive and between 0.179 and 0.789 (Table 3). The Cronbach’s alpha coefficient for the total PIH scale was 0.865. The Cronbach’s alpha if any item deleted was between 0.847 and 0.861. However, all were below the 0.865, so we retained all 12 items. A Cronbach’s alpha between 0.70 and 0.95 is regarded as a positive rating for instruments used in research which suggested the internal consistency and reliability of the Chinese PIH scale [32].
| PIH8 | PIH7 | PIH2 | PIH1 | PIH6 | PIH5 | PIH4 | PIH3 | PIH12 | PIH11 | PIH10 | PIH9 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PIH8 | 1 | |||||||||||
| PIH7 | 0.45 | 1 | ||||||||||
| PIH2 | 0.179 | 0.331 | 1 | |||||||||
| PIH1 | 0.199 | 0.288 | 0.765 | 1 | ||||||||
| PIH6 | 0.404 | 0.382 | 0.236 | 0.216 | 1 | |||||||
| PIH5 | 0.31 | 0.446 | 0.474 | 0.4 | 0.406 | 1 | ||||||
| PIH4 | 0.295 | 0.451 | 0.427 | 0.349 | 0.327 | 0.74 | 1 | |||||
| PIH3 | 0.265 | 0.343 | 0.379 | 0.344 | 0.471 | 0.287 | 0.241 | 1 | ||||
| PIH12 | 0.266 | 0.36 | 0.315 | 0.337 | 0.303 | 0.316 | 0.21 | 0.228 | 1 | |||
| PIH11 | 0.2 | 0.265 | 0.355 | 0.369 | 0.242 | 0.321 | 0.223 | 0.187 | 0.475 | 1 | ||
| PIH10 | 0.217 | 0.289 | 0.346 | 0.371 | 0.184 | 0.336 | 0.254 | 0.214 | 0.382 | 0.789 | 1 | |
| PIH9 | 0.298 | 0.403 | 0.428 | 0.401 | 0.217 | 0.393 | 0.259 | 0.27 | 0.51 | 0.719 | 0.689 | 1 |
Table 3: Sample correlations for the 12-item partners in health scale (n=281).
Validity
Content validity: The Content Validity Index (CVI) was used to test the content validity of the Chinese PIH scale. A panel of experts including five clinical experts from university teaching hospitals and two faculty members from university were asked to rate each item of the Chinese PIH scale. They evaluated the item’s relevance to the scale and scored (from 1=not at all relevant to 4=totally relevant). The content validity index for items (I-CVI) was between 0.86 and 1, and the average of the I-CVIs for all items on the scale (S-CVI/Ave) was 0.965 [33,34]. An I-CVI>0.78 and S-CVI/Ave>0.90 are generally considered to have good content validity [35].
Correlation coefficient between the PAM and PIH: The correlation coefficient between the PAM and PIH was 0.505 (p<0.001), which meant they had moderate positive correlations (Rho between 0.3 and 0.6) [36].
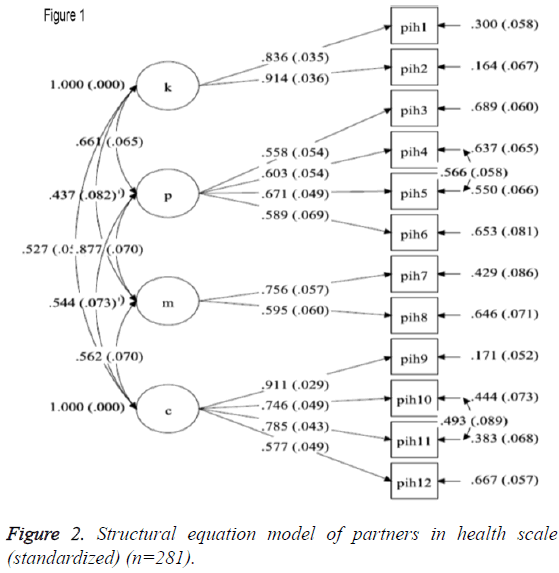
Factor analysis of the Chinese PIH scale: Based on the most recent PIH validation study we tested a 4-factor model for the Chinese PIH, i.e. items 1 and 2-knowledge; items 3, 4, 5 and 6- partnership; items 7 and 8-management; items 9, 10, 11 and 12-coping [24]. The best fitting 4-factor model was a model with error covariance for items 4 and 5 and items 10 and 11. All hypothesized factor loadings were positive and significant when p<0.001 and factor correlation estimates were in the moderate to large range (0.437-0.877) based on conventional standards. Results for this model are presented in Figure 2. The chi-squared results indicated that the model was not a perfect fit (χ2=84.09, df=46, p=0.001) but it failed to provide a good fit of the data based on χ2/df=1.83<2, RMSEA=0.054 (90% CI: 0.035-0.072), CFI=0.965, TLI=0.950 and SRMR=0.046.
Discussion
The Chinese PIH scale has acceptable reliability through testing the internal consistency and test-retest reliability, and satisfactory validity by evaluating content validity and construct validity. The four factors of knowledge, partnership, management and coping reflected the self-management principles.
Internal consistency is a measure of the extent to which items in a questionnaire (sub) scale are correlated (homogeneous). Good internal consistency of items shows that they measure the same concept and have a good construct. The Cronbach’s alpha coefficient of the Chinese PIH scale was similar to the original Australian PIH validation study with 0.82, and the Spanish PIH validation study with 0.80 [22,26].
Confirmatory factor analysis (CFA) is one method to test the theoretical constructs or factors represented by a set of items. The approximate fit indexes were all acceptable except chisquare value with p<0.05 which proved the model here was reasonable. Some experts said that the chi-square value was not a sole index of model fit which was easily affected. There are conditions that although differences between the sample and model implied matrices are negligible, the chi-square value is rejected [37]. Similarities in the wording and context of PIH questions may also have led to residual covariance between items 4 and 5, and items 10 and 11. For example, correlating residual terms for item 10 (I manage the effect of my health condition (s) on how I feel) and item 11 (I manage the effect of my health condition (s) on my social life) was credible due to similar word phrasing as well as tapping into a further minor factor e.g., feeling isolated.
The validity of the Chinese mandarin PIH scale structure was commensurate with the previously reported Australian version but different from the Spanish version and Chinese Hong Kong version [22,24,38]. The reason why we chose to compare these versions was that they assessed the same updated 12 items. The Chinese mandarin version and the updated version have four factors: knowledge (items 1 and 2), partnership (items 3, 4, 5 and 6), management (items 7 and 8) and coping (items 9, 10, 11 and 12). The initial evaluation of the Spanish PIH scale used exploratory factor analysis with three dimensions: knowledge (items 1 and 2), adherence (items 3, 4, 5, 6, 7 and 8), and dealing with or managing side effects (items 9, 10, 11 and 12). The Spanish result was similar to our result. The main difference was that our factor divided symptom management into partnership and management, and maybe a further factor analysis can get a more detailed and enriched result. The Chinese Hong Kong version got three factors after removing item 5 (removed because of less relevance with the whole scale): knowledge (items 1 and 2), symptom management and adherence (items 3, 4, 6, 7 and 8), coping (items 9, 10, 11 and 12). After comparing the four versions of PIH scale, we found that the main difference was with the symptom management and adherence factor. The Spanish and Hong Kong version did not separate them further. The reason for this may be that they tried to accord with the structure of original PIH while the concept of 12 items of the 2010 version was different from that of the updated version [26]. And the other two factors of knowledge and coping were unified, which indicated that the two concepts were the same in different countries and cultures. This suggests that analysis with the updated concept was a better choice.
The study has some limitations. The subjects in the study were mainly patients with diabetes mellitus and/or hypertension in community health centers. This may limit, to some extent, the testing of the Chinese PIH scale’s appropriateness with patients with other chronic conditions. However, in fact, subjects in the study were mainly senior age (mean age 61.43) and we did not exclude subjects with co-morbidities. We plan to test the Chinese PIH scale with patients suffering from chronic diseases within the hospital setting and those with complex chronic diseases, which will modify the Chinese PIH scale because of the imperfections in the CFA.
Conclusion
In conclusion, the Chinese PIH scale has been proved to be a valid and reliable instrument for measuring self-management in Chinese patients with chronic diseases and assessing the knowledge and behaviours of chronic diseases patients within community center settings in China. Healthcare providers in community centers can use the Chinese PIH scale to assess self-management knowledge, behaviours, strengths and barriers of patients with chronic diseases, then provide more effective targeted interventions based on those identified selfmanagement capabilities, and review their patient’s progress with self-management over time. Having a reliable tool to assess self-management in patients with different and various diseases may benefit health services in China by increasing the efficiency of assessment of patient’s needs and reduce healthcare costs as China attempts to cope with the increasing burden of chronic diseases.
Acknowledgement
The authors acknowledge the health providers and chronic patients who involved and participated in the study. This work was supported by the Ethic Committee of Xiang Ya Nursing School, Central South University.
Conflict of Interest
None.
Author’s Contribution
Tang Siyuan, Zhang Xiaofei and Feng Hui contributed to the study design and conception. Zhang Xiaofei was responsible for data analysis and drafting the manuscript. Ren Lu, Wang Jingxia and Chen Jiarui were responsible for data collection. Sharon Lawn was responsible for information about the PIH history, use and prior validation process, and critical revision of the manuscript. David Smith was responsible for providing statistical advice.
References
- National Health and Family Planning Commission of China. Chinese resident’s nutrition and chronic disease status report, 2015. 2016.
- Barr VJ, Robinson S, Marin-Link B, Underhill L, Dotts A, Ravensdale D. The expanded Chronic Care Model: an integration of concepts and strategies from population health promotion and the Chronic Care Model. Healthcare Quarterly 2003; 7.
- Wagner EH, Davis C, Schaefer J, Von Korff M, Austin B. A survey of leading chronic disease management programs: are they consistent with the literature? J Nurs Care Quality 2002; 16: 67-80.
- Franek J. Self-management support interventions for persons with chronic disease: An evidence-based analysis. Ont Health Technol Assess Ser 2013; 13: 1-60.
- Du S, Yuan C. Evaluation of patient self-management outcomes in health care: a systematic review. Int Nurs Rev 2010; 57: 159-167.
- Kralik D, Koch T, Price K, Howard N. Chronic illness self-management: taking action to create order. J Clin Nurs 2004; 13: 259-267.
- Lawn S, McMillan J, Pulvirenti M. Chronic condition self-management: expectations of responsibility. Patient Edu Couns 2011; 84: 5-8.
- Liu X, Wu Y, Li J, Zhao Q. Chronic disease self-management tools in china and abroad: a review. J Nurs 2011; 18: 20-23.
- Ausili D, Masotto M, Dall'Ora C, Salvini L, Di Mauro S. A literature review on self-care of chronic illness: definition, assessment and related outcomes. Prof Inferm 2014; 67: 180-189.
- Battersby MW, Ask A, Reece MM, Markwick MJ, Collins JP. The Partners in Health scale: The development and psychometric properties of a generic assessment scale for chronic condition self-management. Aus J Primary Health 2003; 9: 41-52.
- Lawn S, Battersby M. Capabilities for supporting prevention and chronic condition self-management: a resource for educators of primary health care professionals. Australian Government Department of Health and Ageing: Flinders University, Adelaide, Australia. 2009.
- Walters J, Cameron-Tucker H, Wills K, Schüz N, Scott J, Robinson A. Effects of telephone health mentoring in community-recruited chronic obstructive pulmonary disease on self-management capacity, quality of life and psychological morbidity: a randomised controlled trial. BMJ Open 2013; 3: e003097.
- Clayton C, Feehan L, Goldsmith CH, Miller WC, Grewal N, Ye J. Feasibility and preliminary efficacy of a physical activity counselling intervention using Fitbit in people with knee osteoarthritis: the TRACK-OA study protocol. Pilot Feasibility Studies 2015; 1: 1.
- Ghahari S, Khoshbin LS, Forwell SJ. The multiple sclerosis self-management scale: Clinicometric testing. Int J MS Care 2014; 16: 61-67.
- Versnel J. You’re in Charge: an innovative intervention program for families with adolescents with chronic illnesses. World Feder Occup Therap Bulletin 2013; 67: 41-48.
- Horsburgh MP, Bycroft JJ, Mahony F, Roy D, Miller D, Goodyear-Smith F. The feasibility of assessing the Flinders program TM of patient self-management in New Zealand primary care settings. J Prim Health Care 2010; 2: 294-302.
- Roy DE, Mahony F, Horsburgh M, Bycroft J. Partnering in primary care in New Zealand: ‘clients and nurses’ experience of the Flinders ProgramTM in the management of long-term conditions. J Nurs Healthcare Chronic Illness 2011; 3: 140-149.
- Walker R, Marshall M, Polaschek N. Improving self-management in chronic kidney disease: a pilot study. Renal Soc Aus J 2013; 9: 116-125.
- Jarl J, Tolentino JC, James K, Clark MJ, Ryan M. Supporting cardiovascular risk reduction in overweight and obese hypertensive patients through DASH diet and lifestyle education by primary care nurse practitioners. J Am Assoc Nurs Pract 2014; 26: 498-503.
- Heijmans M, Waverijn G, Rademakers J, van der Vaart R, Rijken M. Functional, communicative and critical health literacy of chronic disease patients and their importance for self-management. Patient Edu Couns 2015; 98: 41-48.
- Spoorenberg SL, Uittenbroek RJ, Middel B, Kremer BP, Reijneveld SA, Wynia K. Embrace, a model for integrated elderly care: study protocol of a randomized controlled trial on the effectiveness regarding patient outcomes, service use, costs, and quality of care. BMC Geriatr 2013; 13: 62.
- Córdova IP-d, Barrios FF, Gutierrez-Gomes T, Piñonez-Martinez MdS, Quintero-Valle LM, Castañeda-Hidalgo H. Self-management in chronic conditions: partners in health scale instrument validation. Nurs Manag 2014; 20: 32-37.
- Lenferink A, Frith P, van der Valk P, Buckman J, Sladek R, Cafarella P. A self-management approach using self-initiated action plans for symptoms with on-going nurse support in patients with chronic obstructive pulmonary disease (COPD) and comorbidities: the COPE-III study protocol. Contemp Clin Trials 2013; 36: 81-89.
- Smith D, Harvey P, Lawn S, Harris M, Battersby M. Measuring chronic condition self-management in an Australian community: factor structure of the revised Partners in Health (PIH) scale. Qual Life Res 2016; 1-11.
- Sousa VD, Zauszniewski JA, Bergquist-Beringer S, Musil CM, Neese JB, Jaber AF. Reliability, validity and factor structure of the Appraisal of Self-Care Agency Scale-Revised (ASAS-R). J Eval Clin Pract 2010; 16: 1031-1040.
- Petkov J, Harvey P, Battersby M. The internal consistency and construct validity of the partners in health scale: validation of a patient rated chronic condition self-management measure. Qual Life Res 2010; 19: 1079-1085.
- Hibbard JH, Stockard J, Mahoney ER, Tusler M. Development of the Patient Activation Measure (PAM): conceptualizing and measuring activation in patients and consumers. Health Serv Res 2004; 39: 1005-1026.
- Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and testing of a short form of the patient activation measure. Health Serv Res 2005; 40: 1918-1930.
- Shi L, Wu Y, Zhang L. Relationship between activation and self-management behavior for the patients with type 2 diabetes. J Nurs Sci 2010; 25: 10-12.
- Schreiber JB, Nora A, Stage FK, Barlow EA, King J. Reporting structural equation modeling and confirmatory factor analysis results: A review. J Edu Res 2006; 99: 323-338.
- Streiner DL, Norman GR. Health Measurement Scales: A Practical Guide to Their Development and Use (3rd edn). Oxford University Press, New York, USA 2008.
- Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007; 60: 34-42.
- Polit DF, Beck CT. The content validity index: are you sure you know what's being reported? Critique and recommendations. Res Nurs Health 2006; 29: 489-497.
- Jingcheng S, Xiankun M, Zhenqiu S. Content validity index in scale development. J Cent South Univ (Med Sci) 2012; 37: 152-155. 21">
- Lynn MR. Determination and quantification of content validity. Nurs Res 1986; 35: 382-386.
- van der Vaart R, Drossaert CH, Taal E, Peter M, Hilderink-Koertshuis RT, Klaase JM, van de Laar MA. Validation of the Dutch functional, communicative and critical health literacy scales. Patient Edu Couns 2012; 89: 82-88.
- Wang M. Latent variable modeling and Mplus application: elementary. Chongqing University Press. BMJ Open 2014; 3: e003097.
- Chiu TML, Tam KTW, Siu CF, Chau PWP, Battersby M. Validation study of a Chinese version of Partners in Health in Hong Kong (C-PIH HK). Qual Life Res 2016; 1-5.