Research Article - Current Trends in Cardiology (2021) Volume 5, Issue 5
Transcatheter aortic valve implantation in Italian women versus men: Single center comparison of baseline characteristics and report of clinical and procedural outcomes
Aleksander Dokollari1,4*, Matteo Cameli1, Giulia Elena Mandoli1, Divya-Shree Patel2, Didar-Karan Kalra2, Marjela Pernoci2, Massimo Bonacchi3
1Division of Cardiology, Le Scotte Hospital, University of Siena, Siena, Italy
2Division of Cardiac Surgery, St. Michael's Hospital, Toronto, ON, Canada
3Department of Experimental and Clinical Medicine, Cardiac Surgery Unit, University of Florence, Firenze, Italy
4Department of Cardiac Surgery, Cardiovascular Research Institute Maastricht (CARIM) Medical University, Maastricht, Netherlands
- Corresponding Author:
- Aleksander Dokollari
Division of Cardiology
Le Scotte Hospital
University of Siena
Siena, Italy
E-mail: aleksanderdokollari2@gmail.com
Accepted date: 03 August, 2021
Citation: Dokollari A, Cameli M, Mandoli GE, et al. Transcatheter aortic valve implantation in Italian women versus men. Single center comparison of baseline characteristics and report of clinical and procedural outcomes. Curr Trend Cardiol. 2021; 5(5):60-67.
Abstract
Objective: To compare the baseline characteristics and outcomes of Transcatheter Aortic Valve Implantation (TAVI) in Italian women and men.
Background: Previous outcomes of TAVI between men and women are contradictory in different patient populations.
Methods: Patients between 75-year old and 87-year old, who underwent TAVI between 2010 and 2016, were retrospectively analyzed.
Results: 256 patients, 114 men and 142 women, were included in the analysis. Baseline characteristics displayed a higher incidence of smoking, myocardial infarction, chronic obstructive pulmonary disease, conduction abnormality, previous percutaneous coronary intervention, and surgery in men (p<0.05). Echocardiographic data evidenced higher transvalvular gradients, higher pulmonary artery pressures, lower aortic valve area and ejection fraction in women (p<0.05). In contrast, men had larger left ventricular outflow tract and aortic dimensions but lower incidence of associated trace-mild aortic valve regurgitation (p<0.05). There was a higher incidence of balloon sheath usage in men (men 21.05% vs. women 9.15%, p<0.05) and lower of perclose device (men 19.3% vs. women 31.6%, p<0.05). Postoperatively, the creatinine level and the indexed effective orifice area were higher in men (p<0.05).
Conclusion: This study reports that although women had a lower Euro Score II, in-hospital outcomes were similar to men in Italian population.
Keywords
Transcatheter Aortic Valve Implantation (TAVI), Women, Patients, Complications, Outcomes
Introduction
Trans catheter Aortic Valve Implantation (TAVI) has been proven to be effective in low-risk patients [1] and Valve-in Valve procedures (ViV) [2,3], becoming a preferred option in selected patients with aortic valve stenosis. The PARTNER 1 trial [4], SCOPE I trial [5] and Evolute Low Risk trial [6], have proven good clinical outcomes with TAVI. However, there is a discrepancy in publication reports regarding the preoperative risk factors between men and women. Many reports have shown similar pre procedural risk between both sex [7-14], while large meta-analysis demonstrate that overall preoperative risk stratification Euro Score II [15] is lower in women presenting for TAVI compared to men. The PARTNER 2 clinical trial reported a lower Euro Score II for women compared to men even though females are considered a risk factor and a score component in the Euro Score II [16]. In addition, the diagnostic echocardiographic features of female patients compared to male are different. These include the left ventricular remodeling in patients with aortic valve stenosis and the reverse remodeling following TAVI. Several studies have evaluated sex differences following TAVI showing similar results in some cases [17,18] and higher survival rate in females in other reports [19,20]. Even in these studies, the data evidenced some discrepancy with respect to sex. Conversely, several meta-analyses have concluded that women have a higher rate of major vascular complications and major bleeding events [21,22]. In addition, the incidence of moderate or greater paravalvular regurgitation is lower in women [23]. The aim of this manuscript is to compare the baseline characteristics and in-hospital outcomes following TAVI in Italian women and men.
Materials and Methods
This is an observational cohort single center study and data was collected retrospectively between December 2010 and December 2016 into an institutional database in Siena, Italy. The reason for the delay of the data was related to in-hospital staff reorganization and hospital policies readjustments. Patients undergoing transcatheter aortic valve replacement were included in the study.
Statistical analysis and clinical data
Data was extracted manually from the database and analyzed using statistical software program SPSS version 26 (SAS Institute, Cary, North Carolina). Unpaired t-test analysis was used for continuous variables and Fisher’s exact test analysis was used to test statistical significance for categorical variables. Continued variables are expressed as mean ± standard deviation. Demographic, clinical, and echocardiographic covariates were assessed singularly in the univariate analysis. Data were analyzed anonymously and the need for individual informed consent was waived due to the retrospective nature of the study. Data was collected prospectively for routine care with no breach of privacy or anonymity. In addition, the study was performed according to the ethical standards of the 1964 Declaration of Helsinki and its later amendments. Ethical Committee approval was waived due to the retrospective analysis of the present study according to National Laws regulating observational retrospective studies (Italian law nr.11960, released on 13/07/2004). Creatinine levels were measured on admission and discharge from the hospital.
Definitions
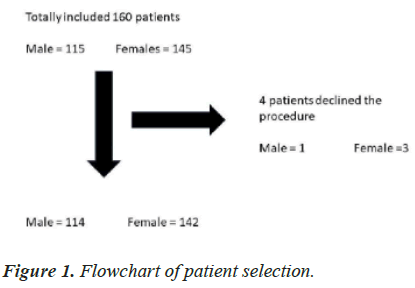
Patient preoperative/postoperative data and complications were based on definitions set forth by the European Society of Cardiology guidelines on valvular heart disease [24]. Clinical endpoints were categorized using the valvular academic research consortium, VARC-2 criteria [25]. The endpoints of in-hospital safety (all-cause mortality, stroke, life-threatening bleeding, acute kidney injury (RIFLE Stage 2 or 3 or renal replacement therapy), coronary artery obstruction requiring intervention, major vascular complication, valve-related dysfunction requiring repeat procedure) were evaluated. The definition of Myocardial Infarction (MI) is based on the STS standard definition. Stroke and Transitory Ischemic Attack (TIA) were defined according to the Stroke Council of the American Heart Association/American Stroke Association [26]. Based on the preoperative data, Euroscore II was calculated to predict the risk of postoperative mortality. Overweight patients were defined if body mass index was higher than thirty. Rehospitalization was defined as every unplanned readmission to the hospital occurring within 30 days after the procedure. Patients that underwent a TAVI procedure in our center with either balloon expandable or self-expandable prosthesis were included in the study (Figure 1). The decision to perform TAVI was made by the heart team. With respect to mortality, we included all deaths after valve implantation regardless of the cause. On the echocardiogram we recorded the Ejection Fraction (EF), the mean (Gmed) and maximum (Gmax) transvalvular gradients, the Aortic Valve Area (AVA), the Left Ventricular Outflow (LVOT), index Effective Orifice Area (iEOA) and ascending aortic diameter. In line with other clinical studies a p-value of <0.05 was considered significant.
Results
In-hospital outcomes
Two hundred sixty patients were included in the analysis (114 male and 142 female patients) between 75 and 87 year old. One male and three female patients who refused the procedure due to personal concerns, the baseline characteristics, i.e., smoking, MI, Chronic Obstructive Pulmonary Disease (COPD), conduction abnormality, previous Percutaneous Coronary Intervention (PCI) and surgery were found to be higher in men (p<0.05) (Table 1). Preoperative echocardiographic data evidenced higher transvalvular gradients, higher pulmonary artery pressures, lower aortic valve area and EF in women (p<0.05) (Table 2). In contrast, men had larger LVOT and aortic dimensions, but lower incidence of associated trace- mild aortic valve regurgitation (p<0.05). Preoperative creatinine clearance was not significantly different between the two groups. For intraoperative outcomes, the only significant differences were the balloon expandable sheath usage of (men 21.05% vs. women 9.15%, p<0.05) and Perclose (Abbott’s ProGlideTM) device usage (men 19.3% vs. women 31.6%, p<0.05) (Table 3). The most preferred surgical access for both groups was the femoral access and there was no difference between the groups. Surgical femoral vessels exposure was higher in the male group (20% vs. 17%) but did not reach statistical significance (p>0.05). There were two periprocedural deaths in the male group and one death in the female group. Postoperative outcomes evidenced a higher creatinine level in men and a higher index Aortic Valve Area (iEOA) (p<0.05) (Table 4). The most used prosthesis in males was the Evolute R while in females was the Edwards Sapien 3. There was one urinary tract infection in the male group. Although PM implantation rate was higher in males compared to females (men 21.32% vs. women 15.6%), this difference did not reach statistical significance (p>0.05). Atrioventricular block type III incidence was greater than two folds in females than males, but this difference did not reach statistical significance (p>0.05). Contrastingly, the incidence of major vascular damage was twice as much in men compared to females (men 5.35% vs. women 2.8%). The hospital length of stay and readmission rate was similar between both groups.
| Male=114 | Female=142 | P-value | |
|---|---|---|---|
| BSA m2 | 1.87 ± 0.26 | 1.65 ± 0.32 | <0.05 |
| Weight kg | 75.38 ± 12.34 | 68.62 ± 13.51 | <0.05 |
| Age (years) | 81.75 ± 5.9 | 83.88 ± 3.7 | <0.05 |
| Hypertension | 87 (76.32%) | 108 (76.06%) | 1 |
| Diabetes | 29 (25.43%) | 28 (19.73%) | 0.29 |
| Insulin-dependent | 14 (12.28%) | 14 (9.85%) | 0.55 |
| NYHA | |||
| Class I | 3 (2.63%) | 3 (2.11%) | 1 |
| Class II | 44 (38.59%) | 45 (31.69%) | 0.29 |
| Class III | 53 (46.49%) | 83 (58.45%) | 0.06 |
| Class IV | 14 (12.28%) | 11 (7.74%) | 0.28 |
| Smoking | 17 (14.91%) | 9 (6.33%) | <0.05 |
| Creatinine level (mg/dL) | 1.35 ± 0.26 | 1.36 ± 1.85 | 0.1 |
| Creatinine clearance ml/min | 104 ± 64 | 102 ± 58 | 0.1 |
| Creatinine clearance | 48.3 ± 11.5 | 46.7 ± 10.8 | 0.07 |
| <60 ml/min | |||
| Dialysis | 5 (4.38%) | 1 (0.70%) | 0.09 |
| MI | 32 (28.07%) | 17 (11.97%) | <0.05 |
| COPD | 35 (30.70%) | 24 (16.90%) | <0.05 |
| Stroke/TIA | 8 (7.01%) | 7 (4.92%) | 0.59 |
| PVD | 32 (28.10%) | 32 (22.53%) | 0.31 |
| Porcellain Aorta | 16 (14.03%) | 32 (22.53%) | 0.1 |
| Sinus rhythm | 83 (72.80 %) | 110 (77.46%) | 0.46 |
| PM | 7 (6.14%) | 4 (2.81%) | 0.22 |
| Chronic Afib | 20 (17.54%) | 26 (18.31%) | 1 |
| Paroxysmal Afib | 3 (2.60%) | 1 (0.70%) | 0.32 |
| Paroxysmal Afib+Left hemi AV-block | 1 (0.80%) | 0 | 0.44 |
| A-V block type I | 3 (2.63%) | 2 (1.40%) | 0.65 |
| RBBB | 2 (1.75%) | 8 (5.63%) | 0.19 |
| LBBB | 5 (4.38%) | 2 (1.40%) | 0.24 |
| Hemi LBBB+RBBB | 4 (3.50%) | 0 | <0.05 |
| Hemi LBBB | 0 | 2 (1.40%) | 0.5 |
| Neoplasia | 19 (16.67%) | 16 (11.26%) | 0.27 |
| Previous surgery | 36 (31.57%) | 29 (20.42%) | <0.05 |
| Previous PCI | 36 (31.57%) | 23 (16.20%) | <0.05 |
| CAD | 47 (41.22%) | 41 (28.87%) | <0.05 |
| EuroScore II | 20.22 ± 12.49 | 19.7 ± 12.56 | 0.96 |
Table 1: Preoperative patient characteristics.
| Males=114 | Females=142 | p-value | |
|---|---|---|---|
| AVA cm2 | 0.65+0.14 | 0.57+0.1 | <0.05 |
| G max mmHg | 80 ± 17 | 89.16 ± 24.18 | <0.05 |
| G med mmHg | 48.1 ± 13.15 | 55.96 ± 16 | <0.05 |
| Associated AR | |||
| None | 13 (11.4%) | 17 (11.97%) | 1 |
| Trace | 41 (35.96%) | 96 (67.60%) | <0.05 |
| Mild | 50 (26.31%) | 22 (15.49%) | <0.05 |
| Moderate | 6 (5.26%) | 6 (4.22%) | 0.77 |
| Severe | 4 (3.50%) | 1 (0.70%) | 0.17 |
| PAPs mmHg | 37.87 ± 9.01 | 41 ± 13.31 | <0.05 |
| EF % | 48.4 ± 10.68 | 53.26 ± 8.99 | <0.05 |
| Aorta dimensions cm | 35.88 ± 5.46 | 33.79 ± 3.99 | <0.05 |
| LVOT cm | 2.4 ± 0.17 | 2.01 ± 1.63 | <0.05 |
Table 2. Preoperative echocardiographic data.
| Males=114 | Females=142 | p-value | |
|---|---|---|---|
| Device type | |||
| CV | 20 (17.54%) | 34 (23.94%) | 0.22 |
| XT | 31 (27.19%) | 31 (21.83%) | 0.37 |
| S3 | 30 (26.31%) | 49 (34.50%) | 0.17 |
| EVR | 33 (28.94%) | 28 (19.72%) | 0.1 |
| Surgical Access | |||
| Femoral | 103 (90.35%) | 128 (90.14%) | 1 |
| Subclavian | 7 (6.14%) | 11 (7.74%) | 0.8 |
| Transapical | 4 (3.50%) | 3 (2.11%) | 0.7 |
| Access closure device | |||
| Perclose | 22 (19.30%) | 45 (31.69%) | <0.05 |
| Prostar | 69 (60.52%) | 73 (51.40%) | 0.16 |
| Femoral artery surgical exposure | 23 (20.17%) | 24 (16.90%) | 0.52 |
| Balloon expandable sheath SoloPath | 24 (21.05%) | 13 (9.15%) | <0.05 |
| Percutaneous transluminal coronary angioplasty | |||
| 24 (21.05%) | 41 (28.87%) | 0.19 | |
| Procedural time min | 128.71 ± 38.6 | 120.12 ± 54.91 | 0.76 |
| Peri TAVI death | 2 (1.75%) | 1 (0.70%) | 0.58 |
| Additional TAVI ViV | 0 | 1 (0.70%) | 1 |
Table 3: Intraoperative outcomes.
| Males=112 | Females=141 | P-value | |
|---|---|---|---|
| Infection | 1 (Urinary tract) | 0 | 0.44 |
| PM | 25 (21.32%) | 22 (15.60%) | 0.19 |
| MI | 0 | 0 | - |
| Cardiac tamponade | 1 (0.89%) | 1 (0.71%) | 1 |
| Creatinine level (mg/dL) | 1.17 ± 0.22 | 1.11 ± 0.44 | <0.05 |
| Residual AR post- procedure | |||
| None | 38 (33.9%) | 43 (30.49%) | 0.58 |
| Trace | 53 (47.32%) | 80 (56.73%) | 0.16 |
| Mild | 16 (14.3%) | 16 (11.34%) | 0.56 |
| Moderate | 5 (4.46%) | 2 (1.41%) | 0.24 |
| Conversion to sternotomy | 0 | 0 | - |
| Index Effective Orifice Area (iEOA) | 1.05 ± 0.12 | 0.84 ± 0.19 | <0.05 |
| iEOA ≤ 0.65 | 0.62 ± 0.06 | 0.60 ± 0.06 | 0.62 |
| Stroke | 1 (0.89%) | 2 (1.41%) | 1 |
| Major Vascular Damages | 6 (5.35%) | 4 (2.83%) | 0.34 |
| Partial rupture of the aortic annulus | 0 | 1 (0.71%) | 1 |
| Left coronary sinus aneurysm | 0 | 1 (0.71%) | 1 |
| PCI post TAVI | 0 | 1 (0.71%) | 1 |
| Retroperitoneal hemorrhage not requiring surgery | |||
| 0 | 2 (1.41%) | 0.5 | |
| New LBBB | 17 (15.17%) | 26 (18.44%) | 0.5 |
| New RBBB | 4 (3.57%) | 3 (2.12%) | 0.7 |
| AV block type 1 | 2 (1.78%) | 5 (3.54%) | 0.46 |
| AV block type 2 | 1 (0.89%) | 0 | 0.44 |
| AV block type 3 | 4 (3.57%) | 10 (7.09%) | 0.27 |
| Total hospital length of stay | 9.93 ± 5.69 | 9.62 ± 4.47 | 0.28 |
| Re-hospitalization | 8 (7.10%) | 8 (5.67%) | 0.79 |
Table 4: In-hospital postoperative outcomes.
Discussion
This manuscript focuses on data from a single center and compares post-TAVI outcomes between the sexes. In line with other clinical studies, our Italian male population had a significantly higher incidence of smoking, Coronary Artery Disease (CAD), PCI, AVA and transvalvular gradients [27]. As expected, the lower BSA in the female group led to a lower AVA and to higher transvalvular gradients. In addition, the Euro Score II for males was higher than females but the difference was not statistically significant [28]. Postoperative outcomes evidenced a higher iEOA in male but the severe iEOA (≤ 0.65) was not statistically different among the groups. This may be related to the smaller aortic annulus in females and the type of prosthesis used. Previous groups tend to use less Medtronic Core valve (ReValving System) prostheses in women than men [29,30]. When those studies were conducted the Edwards company had smaller valve types. However, this was not the case in our study. The PARTNER trial observed a significantly increased risk of peri-procedural stroke (6.7%) compared to medical therapy (1.7%). Subsequent meta-analyses demonstrated thirty-days stroke incidence of 3.1-3.3% and that it confers a 3.5-fold increase in mortality at one-year. In addition, reduce in stroke rate post TAVI procedure has been reported with the introduction of cerebral embolic protection devices. These are filters designed to capture or deflect emboli traveling to the brain during TAVR procedures in order to protect the supra-aortic vessels from embolic debris. In our study, we did not experience a higher rate of stroke and major bleeding in our women population compared to other studies [29]. This may be attributed to the intra procedural operator experience, accurate and precocious treatment of new onset of arrhythmias and technological improvements. It is tempting to speculate that technical improvement in TAVI devices, such as the reduction of the sheath, leads to a lower rate of stroke and vascular complications.
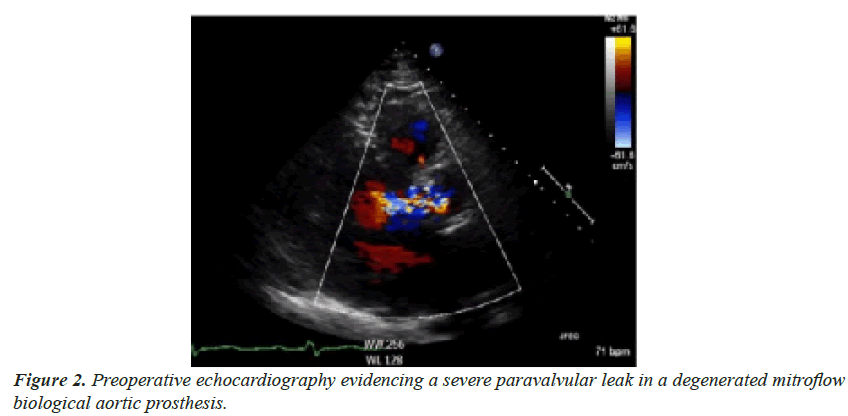
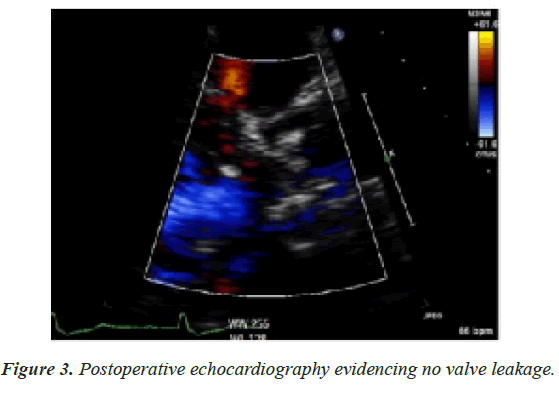
In-hospital survival was not different between the two genders. There were two deaths in the male group and only one in the female group. The low incidence of periprocedural deaths in these groups is related to several factors. First, when we newly introduced the TAVI procedure in our practice, patients were carefully selected to ensure their positive outcomes while also providing us with a good learning curve to improve TAVI results. Second, to decrease the probability of periprocedural complications, the first twenty procedures were mentored by a proctor. The proctor organized regular team rounds to discuss singularly every procedure and technicalities. Altogether, these steps proved to be effective in leading to a low incidence of periprocedural complications. Another postoperative outcome that was different between the sexes was the creatinine level. The CHOICE trial reported a higher incidence of Acute Kidney Injury (AKI) in self-expandable prosthesis compared to balloon-expandable prosthesis (9.4% vs. 4.1%). The Evolute low risk trial reported a higher incidence of AKI post-surgery compared to TAVI (0.9% versus 2.8%) [6]. However, these trials did not perform an ad hoc analysis of AKI incidence post TAVI based on sex. In our analyses, the higher preoperative creatinine clearance level and a higher number of preoperative patients on dialysis in the male group lead to an increased postoperative creatinine level post TAVI. Many studies have outlined the higher incidence of paravalvular leakage in the male population [31]. A subgroup analyses of the CHOICE trial comparing the device success based on the type of device (self-expandable prosthesis versus balloon-expandable prosthesis) reported a higher success rate in women compared to men (83.7% vs. 61.8%) with respect to the balloon-expandable prosthesis while the success rate for self-expandable prosthesis were similar. Our results confirm these outcomes as 4.46% of the males experienced moderate paravalvular regurgitation compared to 1.41% in females. In addition, we performed an outcome analysis comparing the type of the aortic prosthesis between the genders and we did not find differences [32]. Moreover, in our population only one female had to have a ViV-TAVI during the same procedure due to severe paravalvular leakage. The OBSERVANT registry evidenced a higher trend of conduction abnormalities in men. Conversely, the outcomes from our study evidenced that atrio-ventricular block type III incidence was higher in the female group. This is expected as the female annulus is smaller compared to the counterpart. We can speculate that ballooning of the valve may disrupt the annular calcification causing conduction abnormalities. Therefore, small annuli may benefit from self-expandable valves instead of the balloon expandable. Interestingly, the PM implantation rate was higher in the male group and that may be related to the intra/ post-procedural hematoma on the aortic annulus or the severe annular calcification leading to conduction abnormalities. Due to limited experience at the beginning of the TAVI program, we were surgically exposing the femoral vessels. After 47 patients we changed our practice by switching to the percutaneous TAVI procedure and found the results improved (Videos 1 and 2). However, these findings raise the question; does the TAVI procedure have a greater procedural feasibility leading to good outcomes that may be particularly beneficial for the female population, compared to men? To answer this requires specifically designed clinical trials. There is no consistent literature that supports TAVR having a higher rate of any individual complication compared with SAVR, though this may reflect the natural evolution of TAVI technique regarding procedural protocol, postprocedural care, and operator skill (Figures 2 and 3). This maybe related even to the inaccuracy of EuroScore II and STS score in predicting the preoperative risk of TAVI patients. Dokollari et al. [33] have previously described the inability of these risk scores to predict accurately the risk of octogenarians undergoing the TAVI procedure. Therefore, a new dedicated risk score is warranted for TAVI patients. This is one of the few clinical studies that compare the outcomes of Italian patients undergoing TAVI based on gender. Moreover, our data outlined the small differences of in-hospital outcomes compared to other clinical studies. Our findings of non-inferiority of female versus male, in a single center of solely the Italian population are robust and align with other studies. The outcomes of the study could potentially help identify which patients may benefit from experienced TAVI centers. A limiting factor of this study is the lack of a propensity match analysis between the two groups leading to unequal groups. However, the application of this analysis would have led to a lower number of patients with limiting outcomes [34- 36].
Limitations
This is an observational retrospective clinical study and possesses an inherent bias associated with its design. The STS score includes multiple cofactors such as the illicit drug use, alcohol use, severity of carotid stenosis etc. that are not present in our database. Therefore, we used the Euro Score II as a predictive risk score. We did not report a patient frailty index because it was not recorded in our data. Confounding variables such as patient ethnicity (which was not recorded in our data) may have impacted patient complications and survival rates. The size of the patient population also poses an additional limitation as the study only consisted of 256 patients. In addition, the data collected from the study were collected five years ago. As a result, the extent to which the findings can be generalized is hindered. Moreover, patients’ follow-ups were not conducted following hospital discharge. The preprocedural differences among the two groups may have affected the outcomes. However, a propensity match of the two groups would have resulted in a significantly lower number of patients, therefore, reducing the power of the study. Multi-institutional studies which are performed over a long postoperative period on a larger patient population should be conducted to further validate the findings from this investigation.
Conclusion
This study outlines that although women had a lower Euro Score II, the in-hospital outcomes were similar to men. Stroke, severe paravalvular leak and AKI remain important outcomes that influence the in-hospital survival. Further device technological developments will reduce the incidence of such complications.
Impact on daily practice
The learning points from this manuscript are:
• Italian men and women have similar outcomes post TAVI.
• Only the indexed orifice area and creatinine level were higher in male.
Acknowledgment
All the authors contributed equally to this manuscript.
References
- Mack MJ, Leon MB, Thourani VH, et al. Transcatheter aortic-valve replacement with a balloon-expandable valve in low-risk patients. N Engl J Med. 2019;380(18):1695-705.
- Edelman JJ, Khan JM, Rogers T, et al. Valve-in-valve TAVR: State-of-the-art review. Innovat. 2019;14(4):299-310.
- Raschpichler MC, Woitek F, Chakravarty T, et al. Valve-in-valve for degenerated transcatheter aortic valve replacement versus valve-in-valve for degenerated surgical aortic bio prostheses: a 3-center comparison of hemodynamic and 1-year outcome. J Am Heart Assoc. 2020;9(14):013973.
- Smith CR, Leon MB, Mack MJ, et al. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364(23):2187-98.
- Lanz J, Kim WK, Walther T, et al. Safety and efficacy of a self-expanding versus a balloon-expandable bioprosthesis for transcatheter aortic valve replacement in patients with symptomatic severe aortic stenosis: a randomised non-inferiority trial. The Lancet. 2019;394(10209):1619-28.
- Pompa JJ, Deeb M, Yakubov SJ, et al. Transcatheter aortic-valve replacement, with a self-expanding valve in low-risk patients. N Engl J Med. 2019;380(18):1706-15.
- Humphries KH, Toggweiler S, Rodes-Cabau J, et al. Sex differences in mortality after transcatheter aortic valve replacement for severe aortic stenosis. J Am Coll Cardiol. 2012;60(1):882–6.
- D’Ascenzo F, Gonella A, Moretti C, et al. Gender differences in patients undergoing TAVI: a multicentre study. Euro Interven. 2013;9(3):367-72.
- Buchanan GL, Chieffo A, Montorfano M, et al. The role of sex on VARC outcomes following transcatheter aortic valve implantation with both edwards sapien and medtronic core valve re valving system(R) devices: the milan registry. Euro Interven. 2011;7(5):556-63.
- Buja P, Napodano M, Tamburino C, et al. Comparison of variables in men versus women undergoing transcatheter aortic valve implantation for severe aortic stenosis (from Italian multicenter core valve registry). Am J Cardiol. 2013;111(1):88-93.
- Erez A, Segev A, Medvedofsky D, et al. Factors affecting survival in men versus women following transcatheter aortic valve implantation. Am J Cardiol. 2014;113(4):701-5.
- Ferrante G, Pagnotta P, Petronio AS, et al. Sex differences in post procedural aortic regurgitation and mid-term mortality after transcatheter aortic valve implantation. Catheter Cardiovasc Interv. 2014;84(2):264-71.
- Onorati F, D’Errigo P, Barbanti M, et al. Different impact of sex on baseline characteristics and major periprocedural outcomes of transcatheter and surgical aortic valve interventions: results of the multicenter Italian observant registry. J Thorac Cardiovasc Surg. 2014;147(5):1529-39.
- Stangl V, Baldenhofer G, Knebel F, et al. Impact of gender on three-month outcome and left ventricular remodeling after transfemoral transcatheter aortic valve implantation. Am J Cardiol. 2012;110(6):884-90.
- O’Connor SA, Morice MC, Gilard M, et al. Revisiting sex equality with transcatheter aortic valve replacement outcomes: a collaborative, patient-level meta-analysis of 11,310 patients. J Am Coll Cardiol 2015;66:221-8.
- Leon MB, Smith CR, Mack MJ, et al. Transcatheter or surgical aortic-valve replacement in intermediate-risk patients. N Engl J Med. 2016;374(17):1609-20.
- Al-Lamee R, Broyd C, Parker J, et al. Influence of gender on clinical outcomes following transcatheter aortic valve implantation from the UK transcatheter aortic valve implantation registry and the national institute for cardiovascular outcomes research. Am J Cardiol. 2014;113(3):522-8.
- Diemert P, Seiffert M, Schnabel R, et al. Patient gender does not affect outcome after Transcatheter Aortic Valve Implantation (TAVI). J Heart Valve Dis. 2013;22(6):789-93.
- Stangl V, Baldenhofer G, Laule M, et al. Influence of sex on outcome following Transcatheter Aortic Valve Implantation (TAVI): systematic review and meta-analysis. J Interv Cardiol. 2014;27(6):531-9.
- Ravindran M, Henning KA, Qiu F, et al. Predictors of long-term cardiovascular versus non-cardiovascular mortality and repeat intervention in patients having transcatheter aortic valve implantation. Am J Cardiol. 2020;135:105-12.
- Conrotto F, D’ascenzo F, Presbitero P, et al. Effect of gender after transcatheter aortic valve implantation: a meta-analysis. Ann Thorac Surg. 2015;99(3):809-16.
- Parikh PB, Wang TY, Sharma N, et al. Sex-related differences in early and long-term mortality after transcatheter and surgical aortic valve replacement: a systematic review and meta-analysis. J Invasive Cardiol. 2020;32(8):295-301.
- Kodali SK, Williams MR, Smith CR, et al. Two-year outcomes after transcatheter or surgical aortic-valve replacement. New Engl J Med. 2012;366(18):1686-95.
- Nishimura RA, Otto CM, Bonow RO, et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the american college of cardiology/american heart association task force on clinical practice guidelines. J Am Coll Cardiol. 2017;70(2):252-89.
- Kappetein AP, Head SJ, Généreux P, et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the valve academic research consortium-2 consensus document. J Am Coll Cardiol. 2012;60(15):1438-54.
- Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the american heart association/american stroke association. stroke. 2018;49(3):46-99.
- Hayashida K, Morice MC, Chevalier B, et al. Sex-related differences in clinical presentation and outcome of transcatheter aortic valve implantation for severe aortic stenosis. J Am Coll Cardiol. 2012;59(6):566-71.
- Finkelstein A, Havakuk O, Steinvil A, et al. Gender differences and clinical outcome in patients undergoing trans-femoral aortic valve implantation. Int J Cardiol. 2013;168(5):4854-5.
- Ndrepepa G, Schulz S, Neumann FJ, et al. Bleeding after percutaneous coronary intervention in women and men matched for age, body mass index, and type of antithrombotic therapy. Am Heart J. 2013;166(3):534-40.
- Williams M, Kodali SK, Hahn RT, et al. Sex-related differences in outcomes after transcatheter or surgical aortic valve replacement in patients with severe aortic stenosis: insights from the partner trial (placement of aortic transcatheter valve). J Am Coll Cardiol. 2014;63(15):1522-8.
- Zhao ZG, Liao YB, Peng Y, et al. Sex-related differences in outcomes after transcatheter aortic valve implantation: a systematic review and meta-analysis. Circ Cardiovasc Interv. 2013;6(5):543-51.
- Buchanan GL, Chieffo A, Montorfano M, et al. The role of sex on VARC outcomes following transcatheter aortic valve implantation with both edwards sapien™ and medtronic core valve revalving system devices: the milan registry. Euro Interven. 2011;7(5):556-63.
- Dokollari A, Bisleri G, Patel DS, et al. The jungle of risk scores and their inability to predict long-term survival. The truth behind the mirror. J Cardiac Surg. 2021;36(8):3004-5.
- Eggebrecht H, Schmermund A, Voigtlander T, et al. Risk of stroke after Transcatheter Aortic Valve Implantation (TAVI): a meta-analysis of 10,037 published patients. Euro Intervention. 2012;8(1):129-38.
- Muralidharan A, Thiagarajan K, Van Ham R, et al. Meta-analysis of perioperative stroke and mortality in transcatheter aortic valve implantation. Am J Cardiol. 2016;118(7):1031-45.
- Abdel-Wahab M, Mehilli J, Frerker C, et al. Comparison of balloon-expandable vs self-expandable valves in patients undergoing transcatheter aortic valve replacement: the choice randomized clinical trial. Jama. 2014;311(15):1503-14.