Research Article - Biomedical Research (2017) Volume 28, Issue 3
To compare the healing of pressure sores by the use of combination therapy with platelet rich plasma and gelatin hydrogel versus platelet rich plasma and collagen
Qian Yu1, Fang-Jing Han1 and De-Sheng Lv2*1Wound Care Center, the Second Affiliated Hospital of Dalian Medical University, China
2Department of Thoracic Surgery, the Second Affiliated Hospital of Dalian Medical University, China
- *Corresponding Author:
- De-Sheng LV
Department of Thoracic Surgery
The Second Affiliated Hospital of Dalian Medical University, PR. China
Accepted date: August 2, 2016
Abstract
Aim and objective: To compare the healing of Pressure sores by combination therapy with platelet rich plasma and gelatin hydrogel versus combination therapy with a platelet rich plasma and collagen.
Material and method: The total sample size was comprised of 320 subjects. The sample was divided into two subgroups. First group received treatment with platelet rich plasma application with a gelatin sheet and second group received platelet rich plasma treatment with collagen ointment. Treatment with platelet rich plasma involves five steps starting from blood collection, centrifugation, separation of Platelet rich plasma, activation of coagulation process, placement of platelet rich plasma and covering with secondary dressing of either gelatin or collagen. The wound was dressed with this combination was review after 7 days, 4 weeks and 7 weeks.
Results: Primary outcome was reduction of ulcer at 7th day, 4th week and at 7th week interval. The depth, time of the depth of sore, closure of wound, CVIQ score, area of ulcer, and adverse effects/ complications were evaluated. Complete healing rates were almost same at 7th week between the PRP with gelatin hydrogel and PRP with Collagen. The results showed non-significant results for the complete healing of pressure sores between both the modalities. In the model, except ulcer depth, no one showed the significant prediction of complete healing within 7 weeks.
Conclusion: Both the combined modalities proved to be very successful in the healing of pressures sores. However, our research study found no difference in the healing outcome of pressures sores between the PRP with gelatin hydrogel and PRP with Collagen.
Keywords
Pressure sores, Platelet rich plasma, Gelatin hydrogel, Collagen, Healing.
Introduction
The pressure sores are the results of injury localized to the skin and its underlying tissues. Localized injury in pressure sores usually present on the bony prominences as the result of pressure or pressure with shear [1]. The injury from the pressure sores shows various effects starting from non blanchable erythema of superfacial skin to the very deep ulcers limiting the bony areas. The pressure sores causes a severe affect not limited to the patient but on the entire health system [2]. As the patient safety is of prime concern of our healthcare system thus the main aim of the healthcare system to reduce the frequency of pressure sores.
An estimated 2.5 million pressure ulcers are treated each year in acute care facilities in the United States alone [3]. Pressure sores considered to be the one of the most common conditions encountering in the patients who is acutely hospitalized or patients having long term treatment in the medical hospitals or nursing homes.
Pressure sores imposes a detrimental problem for the older age group patients because majority of them associated with pain, osteomyelitis and mortality [4,5]. The prevalence of pressure ulcers reaches 24% of residents in nursing homes [6,7]. As per the National Pressure Ulcer Advisory report, in the United States of America, each year, approximately 3,000,000 people develop pressure sores. Out of these, approximately 60 thousand patient develop severe complication which further leads to death [3,8].
As the incidence of pressure wound is increasing day by day, various councils, academic bodies and advisory panels have made a conclusive report on this and made the elaborated the clinical guidelines in the prevention and treatment of pressures sores [8]. The guidelines indicate that the hydrocolloids is one of the best approaches for the treatment of pressure sores [8,9].
As per the literature, the chronic wound takes around seven to eight week to heal. Chronic wounds affect around 1% of the population with a prognosis of non-healed ulcer at 20% at 2 years, 8% at 5 years and recurrence of 6-15 % per year [10,11].
Platelet rich plasma is a blood plasma which is enriched with the platelets. Autologous platelet rich plasma is the basis of autologous growth factors such as platelet derived growth factor, transforming growth factor and vascular endothelial growth factor [12,13]. Platelet rich plasma has been used in the various treatment modalities starting from bone defects, tissue injuries and chronic ulcers etc. [12,13].
Literature and research suggest that if the PRP impregnated with gelatin sheet, the combination of this releases many growth factor like Platelet-Derived Growth Factor (PDGF-BB) and (Transforming Growth Factor) TGF-B that help in improving the wound healing as well as enhancement of angiogenesis [13,14]. The wound healing effect of PRP covered with this sheet is expected to be enhanced by the sustained release of growth factors from the gelatin sheet as a result of its biodegradation after application [13,14].
Now days, collagen can also be used for the treatment of pressure sores. Collagen which is used in wound dressing was extracted from the bovine skin. This type of collagen enriched with majority of type I collagen and small amount of type III and type V fibres [15,16]. Collagen packed with platelet rich plasma may be applied deep in the ulcers to increase the healing [17].
With this in mind, we have planned a Comparative research study to compare the healing of pressure sores between the combination platelet rich plasma and gelatin hydrogel and platelet rich plasma and Collagen.
Aim and Objectives
To compare the healing of pressure sores by the use of combination therapy with platelet rich plasma and gelatin hydrogel versus platelet rich plasma and collagen
Objective: The study was open label, multiple dose and clinical research study to evaluate the efficacy of combination therapy of PRP (Platelet Rich Plasma) and gelatin sheet in assessment of wound healing of pressure sores. Furthermore, to compare the efficacy of this combination therapy versus combination therapy with collagen and platelet rich plasma.
Material and Method
Ethical approval was taken from Institutional ethical board before starting the study. From each and every patient informed consent was also taken. The total sample size was comprised of 320 subjects visiting to Department of Thoracic Surgery, Wound Care Center, The Second Affiliated Hospital of Dalian Medical University, China and other affiliated various nursing homes. Patients that are having chronic bed sores but referred by the other physicians and identified through a number of wound care centers in the centre of Dalian, Liaoning (China) also included the study. The subjects were between the ages of 20-90 years. The sample was divided into two subgroups. First group received treatment with platelet rich plasma application with the sheet of gelatin and second group received PRP treatment with the collagen ointment. Treatment with PRP involves five steps starting from blood collection then centrifugation, collection of PRP, activation of coagulation process by adding calcium chloride, application of PRP and in the end covering of secondary dressing either with collagen or with gelatin hydrogel. All the subjects were selected based on the inclusion and exclusion criteria which are enlisted below.
Inclusion criteria
• Sore which is not healing since 6 months.
• Sore which is not responding to conventional treatment since 2 months.
• Age of patient must be between 20 -90 years.
• One or two ulcers together whose area is equal or less than 20 cm2.
Exclusion criteria
• Those patient that were pregnant or on breast feeding.
• Patients with a bleeding disorder, uncontrolled sugar levels and ulcers with active infection and saphenofemoral incompetency.
• Those patient that were on continues corticosteroid therapy (Prednisolone with dosage of >20 mg/day).
• Patients that were on anticoagulant therapy and antithromobotics.
• Those patients who were not willing to sign the consent form.
• Any patient if developed sign and symptoms of infection that was further assessed by the authors and asked for not continue with the study.
Division of subgroups
In this study, patients will be randomized to either the gelatin sheet subgroup or Collagen dressing subgroup at a ratio of 1:1 without stratification. Randomization will be performed by assigning random numbers from random number tables to the treatment conditions. A randomization-based comparison between these groups is expected to achieve significant improvements in accuracy with a lack of bias. This comparison will provide useful information for designing and conducting future trials.
The total sample size was divided into two subgroups. First group was comprised of 160 subjects out of which 102 were male and 58 were female subjects. The age of subjects in this group was between 20-82 years. These subjects were treated with the combination of gelatin hydrogel and platelet-rich plasma. Group II was comprised of 160 subjects, out of which 120 were male and 40 were female patients. The age of subjects in this group was between 23-90 years. This group was treated with collagen and PRP. Subjects in both the group were reviewed after 7 weeks.
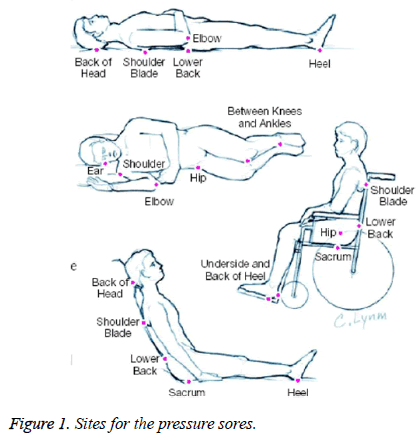
Study treatment involved only one ulcer per patient. The sacrum and heel found to be the commonest location of pressure sores in our study. The other locations of pressure sores in our study encountered are the back of the head and ears, the shoulder blade, the elbows, the lower back, buttock, the hips and the inner knees as shown in Figure 1.
The PRP gel was prepared by incorporation of platelet rich plasma, i.e. obtained from the autologous whole blood, with the calcium chloride and thrombin. Basically, the purpose behind the addition of thrombin and calcium chloride to PRP was to activate the alpha granules, so that they can release various growth factors like platelet derived growth factor, vascular endothelial derived growth factor etc.
Obtaining the PRP
1 ml of 3.8 w/v% sodium citrate solution was allowed to get in the 10 ml vacuumed tube through the side valve. Then the 9 ml of blood was withdrawn. An 18 gauge needle was used to collect the sample. Samples were gently agitated to thoroughly mix the anticoagulant with the blood. Since free calcium ions are required for blood clotting, sodium citrate, an effective anticoagulant was used to bind free calcium ions. Since both sodium and citrate are found in the body, it was recommend as safe to use as PRP samples. The sample was centrifuged at 400 G at 1500 RPM for 15 minutes at room temperature. Around 1.2 ml of supernatant plasma is collected per tube. Mixture of 5 ml of calcium chloride at 0.025 mol/l and autologous thrombin is prepared in the ration of 1:1, which is further act as activator for the solution. With 10:1 by volume, a mixture of centrifuged platelet rich plasma and activator was incubated for 5 minutes. Platelets of obtained PRP were counted and further the accurate concentration of various growth factors in the activated PRP was also quantified.
Obtaining of gelatin sheet
Hokugo et al. determined that the PRP growth factors are immobilized via physicochemical interactions with the gelatin molecules within the hydrogel. This causes a release of growth factors correlating with hydrogel degradation. Gelatin hydrogels/sponges not only have the ability to incorporate proteins and growth factors, but can also incorporate nanofillers such as inorganic minerals or other nanofillers [18].
Gelatin hydrocolloid sheets were prepared at the department of tissue engineering. 40 gm of aqueous solution was mixed 100 ul of aqueous gluteraldehyde. The resultant solution was poured into polystyrene dishes. After 12 hours at 2°c temperature, cross linking of gelatin take place. To inactivate the residual gluteraldehyde the sheets were placed in 100 mm glycine aqueous solution. Then the sheets were washed away double distilled water and sterilized with ethylene oxide gas.
Application of combination of platelet rich plasma and gelatin hydrogel dressing
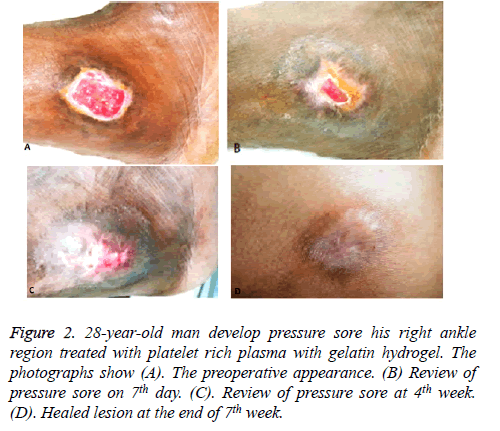
This application was done on the Group I patients. After the complete debridement of pressure sores, the activated PRP was applied covering the pressure sore. After application of platelet rich plasma, the wound was totally occluded with gelatin hydrogen. The wound was reviewed at 7th day, 4th week and at the end of 7th week. At every review appointment, new dressing was prepared as shown in Figure 2.
Figure 2. 28-year-old man develop pressure sore his right ankle region treated with platelet rich plasma with gelatin hydrogel. The photographs show (A). The preoperative appearance. (B) Review of pressure sore on 7th day. (C). Review of pressure sore at 4th week. (D). Healed lesion at the end of 7th week.
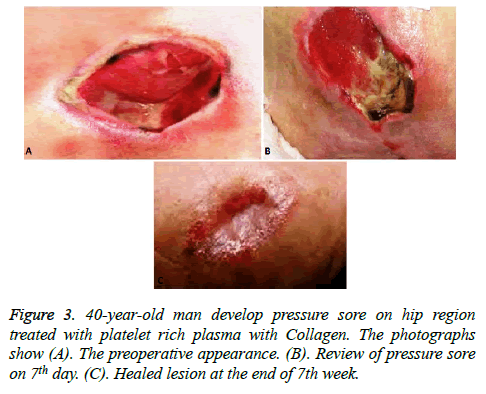
Application of combination of Platelet rich plasma and collagen
This Application was done on the Group II patients. Topical Ointment which is the combination of Hyaluronic acid sodium salt by fermentation and bacterial collagenase from nonpathogenic Vibro alginolitycus (>2.0 nkat/g), available on OTC was used for these patients. After the debridement of pressure sores, the activated PRP was applied on pressure sores. After application of platelet rich plasma, the wound was covered with a layer of 2 mm thickness with OTC available collagen. To ensure the complete occlusion of collagen with the wound, a firm compression bandage or elastic medical compression stocking to the wound was applied. The wound was dressed with this combination was review after 7 days, 4 weeks and 7 weeks. At every review appointment, new dressing was prepared as shown in Figure 3.
Outcome measures
Sore depth: The sore depth was noted with the help of probe and recorded in the every visit of the patient at 7th day, 4th week and 7th week of the treatment compared to baseline. Sore depth was recorded in the units of millimetre.
Time of wound closure: This variable was used for the total number of days taken to complete closure of the wound with the baseline from the administration of PRP with the combination of gelatin hydrogel or collagen. This was evaluated by the three expert physicians differently to ensure the objectivity and reproducibility of the evaluations.
Area/size of the sore: The surface area of pressure sore was depicted in the square centimeter. The area of the sore was measured at the baseline and then at the 7th day, after 4 weeks and after 7 weeks.
CIVIQ score
This CIVIQ score was used for analysing the effect of pressure sore on quality of life. Basically, it includes 4 components, physical, psychological, social and pain. It was measured by using questionnaire, 20 score corresponds to the bad/lowest quality of life and for the best quality of life, the score was given 100.
Complications/adverse effects
During the each and every visit of study, authors have recorded if the patient had experienced any adverse effects or the complications. Complying with the current legislations, at any point of time, if the patient reported any serious adverse reaction and unexpected reaction will be informed to higher authorities within next 24 hours.
Statistical analysis
The principle behind the result was to analyse the effectiveness in intention to treat and treatment completers. The primary outcome was reduction of area/size of ulcer at 7th day, 4th week and at 7th week interval. The depth, time of the depth of sore, closure of wound, CVIQ score, area of ulcer, and adverse effects/complications were evaluated.
For the categorical variables, the comparison was done by using chi square test/F test (Fisher Exact Test). For the analysis of continuous variables, student t-test was used. The p-value less than 0.05 were considered as the significant result. Bonferroni inequality was used for multiple comparisons adjustment. Kaplan-Meier method was used for pair wise comparison between the groups.
Results
The result showed that, entire healing process were almost the same at 7th week between the PRP with gelatin hydrogel and PRP with Collagen as shown in Table 1. At the earlier point of time, between the two groups healing rate were comparable to each other: PRP with Collagen healed 25% pressure sores (40/160) within 1 week and 40% (64/160) within 4 weeks. PRP with Gelatin hydrogel healed 20% pressure sores (32/160) within 1 week and 30% (48/160) within 4 weeks. While the results of statically analysis of Kaplan-Meier method showed no significant difference with the log of 0.69 and p-value of 0.510 in complete healing of the pressure sores between the two subgroups. For the PRP with collagen treated subgroups, the mean healing time was 5 weeks with the Confidence Interval (CI) of 96%. PRP with gelatin hydrogel treated patients had mean time of healing was 6 weeks with a confidence interval of 96%. The results showed non-significant results for the complete healing of pressure sores as shown in Table 1. Baselines measures of ulcer depth, area and duration were the covariates associated with complete healing within 7 weeks. In the model, except ulcer depth, no one showed the significant prediction of complete healing within 7 weeks.
| End point | PRP with gelatin hydrogel | PRP with Collagen | Difference (96% CI) | P-value |
|---|---|---|---|---|
| Primary complete healing within 7 weeks | 83 | 86 | 1% (26-29%) | 0.786 |
| Area healed per day, mm2/day, mean ± SD | 7 ± 20 | 6 ± 18 | 0 | 0.111 |
Table 1. Comparison of healing rates for PRP with gelatin hydrogel and PRP with Collagen.
In a Post Hoc analysis, baseline sore depth was dichotomized at the mean value and analysed. The healing rate for pressure sores of 2-20 mm deep sore was 40% for PRP with collagen recipients and 10% for PRP with gelatin hydrogel recipients with a p-value of 0.111. The pressure sores having the depth of 0 to 1 mm had a mean time of healing been 4 weeks with confidence interval of 96%. For the pressures sores deeper than 2 mm, the mean healing time was 7 weeks with confidence interval of 96% as shown in Table 2.
| Total patients | Healed | Not healed | OR (CI 96%) | |
|---|---|---|---|---|
| Ulcer duration, weeks, 9=75th percentile | ||||
| 0.1-7 | 240 | 144 | 96 | 4.98 |
| 8-144 | 80 | 20 | 60 | 0.2 |
| Ulcer area, median=120 mm | ||||
| 13-120 mm2 | 119 | 78 | 41 | 3.39 |
| 120-123, 299 mm2 | 121 | 44 | 77 | 0.7 |
| Ulcer depth, mean=2 mm | ||||
| 0-1 mm | 192 | 116 | 76 | 8 |
| 2-20 mm | 128 | 30 | 98 | 0.11 |
Table 2. Complete ulcer healing within 7 Weeks according to baseline characteristics.
The results showed non-significant difference in the mean healing time between the PRP with collagen and PRP with gelatin hydrogel with non-significant p-value of 0.230.
A post hoc analysis was done to calculate the mean healing time of pressure sores as shown in Table 2. If the duration of pressure sore was 7 weeks than the mean time healing was 4 weeks (96% confidence interval), if the healing time ulcer extend more than 7 weeks the mean time healing was 6 weeks (96% confidence interval). After the adjustment of the sore duration, the results showed non-significant difference in the healing time between the both subgroups with a non-significant p-value of 0.702.
The pressure sores having the surface area less than 120 mm, the mean time of healing was 4 weeks with the confidence interval of 96%. Pressure sores having the surface area of more than 120 mm had a mean time of healing was 5 weeks as shown in Table 2. After the adjustment of baseline area of sore, there was no significant difference between the PRP with collagen and PRP with gelatin hydrogel with a non-significant p-value of 0.508.
There were significant improvements in CIVIQ (Health- Related Quality Of Life) scores after both the application of PRP with gelatin hydrogel and PRP with collagen. The CIVIQ score was compared between the baseline and at the end of 7th week. However, there was not a significant difference between the CIVIQ score between the hydrogel and collagen.
The most common location of pressure sores was found to be on the region of sacrum. Out of 320 patients, 108 (33.7%) patients had pressure sores in the sacrum region, 90 (28.12%) had in the heel region, 40 (12.5%) had in buttock region, 24 (7.5%) had in lower back, 20 (6.2%) had in back of head and ear, 18 (5.6%) had on shoulder region, 15 (4.6%) had on the elbow and 5 (1.5%) had in the inner knee.
In our study, no adverse effects have been reported after the application of PRP with gelatin hydrogel or PRP with Collagen. The authors, clinicians, healthcare workers had closely monitored the unintended effect of the study and till now, no such case has been reported.
Discussion
The research study was designed to compare the healing pattern of pressure sores between the PRP with gelatin hydrogel versus PRP with collagen. According to our knowledge, this is first ever clinical study conducted on these materials. After enrolling 320 patients, a non-significant difference in healing rates between the PRP with gelatin hydrogel treated patients and PRP with collagen treated patients was observed. Sore depth was the only significant covariate variable that showed significant sore healing at the 7th week.
Due to the advancement of various skin substitutes that were derived from bioengineering resources, the various growth factors released by cells have been further used an effective treatment for pressure sores. But due to the cost, storage problems and non-availability in all the rural areas, the use of this substitute is limited [19].
Literature suggests that the growth factor released by platelets contained in PRP promoted vascular regeneration and cell growth, leading to wound healing. We have also found that PRP application promote the fibroblast growth and induced epithelialization and neovascularization, as in accordance with the other studies. Our study favours the factor that the PRP trigger the healing of pressure sores when the degree of healing appears to have stalled.
In all cases of pressure sores in our study, showed that the appearance of sore bed bleeding during dressing changes and sore palpation was noted and is seen as a positive indicator for wound healing. Once the pressure sore base had in-filled with gelatin hydrogel and collagen along with the PRP present more conservatively treatment option.
The gelatin sheet which has been used in the study is freeze dried and can be stored at room temperature for many months. Therefore, it is possible to use this combination therapy consisting of PRP and a gelatin sheet anywhere when needed, and its efficacy might be superior to that of bioengineered skin substitutes, as these treatments have a similar mechanism of action in secreting growth factors in a sustained manner. So, we can use this treatment approach at very low cost and easily available.
Collagen which is used in wound dressing was extracted from the bovine skin. This type of collagen enriched with majority of type I collagen and small amount of type III and type V fibers. Collagen is available in various forms like sheets, pads, gets etc.[15].
According to Pott et al. in 2014, 29 clinical trials had been conducted that shows that hydrocolloids are superior in relation to gauze. Majority of the trails concluded that the hydrocolloids proved to be the best wound healing dressing than the other simple dressing used in the treatment of chronic wounds [8]. Burgos et al. revealed that there was nonsignificant difference in healing of ulcer between the hydrocolloid and collagens dressing [20]. The results of our study are quite consistent with the results of above mentioned studies.
Darkovich et al. compared BioFilm® hydrogel dressing with the DuoDERM® hydrocolloid dressing in the healing of grade 1 (ulceration or skin breakdown limited to superficial epidermis and dermal layer) and 2 ulcers (ulceration extending through the dermis but not through adipose tissue) based on the Enis and Sarmienti classification system (equivalent to stage II and III in the NPUAP system). After 60 days treatment, a significantly higher proportion of pressure ulcers healed in the hydrogel group compared with the hydrocolloid group (RR 1.82 (95% CI, 1.09-3.05), P=0.02). The results of this study contradict the results of our study [21].
The analysis of our study supports the major previous studies and guidelines that emphasize assessment of sore depth, area and duration. Our study outcome showed that the sore depth was the single predictor for the outcome of the healing. The heterogeneity of the results occurs due to the use of different techniques for assessing the ulcer depth. The results of our study are quite in consistence with results of the study conducted by Graumlich et al. [22].
With these results and findings, we can say that the new treatment combination modalities in the treatment of pressures sores are emerging and they are proved to be successful. Combination modalities are proved to be more superior to the other bioengineered skin substitutes.
Regarding the limitation of the study, here the study was conducted in different hospital and nursing homes. Therefore the results of study might not apply in patient management with different protocols. There was heterogeneity in the healing outcome among different nursing homes.
Conclusion
Both combined modalities proved to be very successful in the healing of pressures sores. However, our research study found no difference in the healing outcome of pressures sores between the PRP with gelatin hydrogel and PRP with Collagen. Further longitudinal studies need to be conducted on these materials specifically in the healing of deep seated pressure sores. To our knowledge this was the first ever conducted study on this.
References
- Steven A, David B, Nancy B, Laura H, Susan L, Jeanine M, Kathy S, Maranda V, Jennifer VR, Aamir S. Friction iunduced skin injuries-are they pressure ulcers. Nat Pres Ulc Adv Pan Wh Pr 2012; 1.
- European Pressure Ulcer Advisory Panel. The EPUAP guide to pressure ulcer grading 2007.
- Dorner B, Posthauer ME, Thomas D. The role of nutrition in pressure ulcer prevention and treatment. Nat Pres Ulc Adv Pan 2009.
- Bates-Jensen BM. Quality indicators for prevention and management of pressure ulcers in vulnerable elders. Ann Intern Med 2001; 135: 744-751.
- Berlowitz DR, Brandeis GH, Anderson J, Du W, Brand H. Effect of pressure ulcers on the survival of long-term care residents. J Gerontol A Biol Sci Med Sci 1997; 52: M106-110.
- Langemo DK, Olson B, Hunter S. Incidence of pressure sores in acute care, rehabilitation, extended care, home health, and hospice in one locale. Decubitus 1989; 2: 42.
- Young L. Pressure ulcer prevalence and associated patient characteristics in one long-term care facility. Decubitus 1989; 2: 52.
- Pott FS, Meie MJ, Dorociak Stocco JS, Crozeta K. The effectiveness of hydrocolloid dressings versus other dressings in the healing of pressure ulcers in adults and older adults: a systematic review and meta-analysis1 Rev. Latino Am Enfermagem 2014; 22: 511-520.
- European Pressure Ulcer Advisory Panel (EPUAP) and National Pressure Ulcer Advisory Panel (NPUAP). Prevention and treatment of pressure ulcers: quick reference guide 2009.
- Laureano A, Rodrigues A. Cicatrizacao de feridas. Rev Soc Port Dermatol 2011; 69: 355-365.
- Lacci KM, Dardik A. Platelet-rich plasma: support for its use in wound healing. Yale J Biol Med 2010; 83: 1-9.
- Kakudo N, Minakata T, Mitsui T, Kushida S, Notodihardjo FZ. Proliferation-promoting effect of platelet-rich plasma on human adipose-derived stem cells and human dermal fibroblasts. Plast Reconstr Surg 2008; 122: 1352-1360.
- Kushida S, Kakudo N, Morimoto N. Platelet and growth factor concentrations in activated platelet-rich plasma: a comparison of seven commercial separation systems. J Artif Organs 2014; 17: 186-192
- Matsui M, Tabata Y. Enhanced angiogenesis by multiple releases of platelet-rich plasma contents and basic fibroblast growth factor from gelatin hydrogels. Acta Biomater 2012; 8: 1792-1801.
- Resources in wound care: 1999 directory. Adv Wound Care 1999; 12: 155-160, 163-166.
- Griswold JA, Cepica T, Rossi L, Wimmer JS, Merrifield HH. A comparison of Xeroform and SkinTemp dressings in the healing of skin graft donor sites. J Burn Care Rehabil 1995; 16: 136-140.
- Spenceri EA, Nahass GT. Topically applied bovine collagen in the treatment of ulcerative necrobiosis lipoidica diabeticorum. Arch Dermatol 1997; 133: 817-818.
- Hokugo A, Ozeki M, Kawakami O, Sugimoto K, Mushimoto K, Morita S, Tabata Y. Augmented bone regeneration activity of platelet-rich plasma by biodegradable gelatin hydrogel. Tissue Eng 2005; 11: 1224-1233.
- Naoki M, Natsuko K, Makoto M, Tsunetaka O, Tomoya H, Kenji S, Masaya Y, Yasuhiko T, Kenji K. Exploratory clinical trial of combination wound therapy with a gelatin sheet and platelet-rich plasma in patients with chronic skin ulcers: study protocol. BMJ Open 2015; 5: e007733.
- Burgos A, Gimenez J, Moreno E, Lamberto E, Utrera M, Urraca EM. Cost, efficacy, efficiency and tolerability of collagenase ointment versus hydrocolloid occlusive dressing in the treatment of pressure ulcers. Clin Drug Investig 2000; 19: 357-365.
- Darkovich S, Brown-Etris M, Spencer M. Biofilm hydrogel dressing: a clinical evaluation in the treatment of pressure sores. Ostomy Wound Manage 1990; 47-60.
- Graumlich JF, Blough LS, McLaughlin RG, Milbrandt JC, Calderon CL. Healing pressure ulcers with collagen or hydrocolloid: a randomized, controlled trial. J Am Geriatr Soc 2003; 51: 147-154.