Research Article - Journal of Public Health Policy and Planning (2022) Volume 6, Issue 1
Time to discontinuation of long acting reversible contraceptive methods among married reproductive age women in Hadiya zone.
Ashenafi Abebe Gaenamo1* and Nebiyu Dereje Abebe2
1Department of Statistics, Wachemo University, Hosaena, Ethiopia
2Department of Public Health, Wachemo University, Hosaena, Ethiopia
- Corresponding Author:
- Ashenafi Abebe Gaenamo
Department of Statistics
Wachemo University Hosaena
Ethiopia
E-mail: ashujajura@gmail.com
Received: 31-Dec-2021, Manuscript No. AAPHPP-22-51838; Editor assigned: 02-Jan -2022, PreQC No. AAPHPP-22-51838(PQ); Reviewed: 16-Jan-2022, QC No. AAPHPP-22-51838; Published: 22-Jan-2022, DOI:10.35841/aaphpp- 6.1.101
Citation: Gaenamo AA, Abebe ND. Time to discontinuation of long acting reversible contraceptive methods among married reproductive age women in Hadiya zone. J Public Health Policy Plann. 2022; 6(1):101.
Abstract
Background: A retrospective cohort study examining the effects of individual characteristics, side effects experienced, and service quality on contraceptive discontinuation was undertaken in six health facilities and one hospital of Hadiya Zone, Southern Ethiopia. The data was taken from the collection of September 2010 to June 2015 follow up forms. The baseline population included 563 women aged 15–49 who were new or continuing users of the injectable, IUD, or oral contraceptive pill.
Methods: The study design employed being a retrospective cohort study, a recent Demographic and Health Surveys (DHS) and Reproductive Health Surveys (RHS) have not collected the necessary data to calculate discontinuation rates and provided that there is densely populated population. A total of 473 women (84%) were re-interviewed after one year. Life tables and Coxproportional hazards models were used to present discontinuation rates and factors associated with contraceptive discontinuation. Among new users, discontinuation of the baseline method at 12 months was high (45%); Especially for users of the injectables (50%).
Results: The prevalence of discontinuation and switching of contraceptive method among women were found to be 38.4% and 15.4%, respectively. The model demonstrated that women in early reproductive years (15–20 and 21–25) significantly more often (odds ratio (OR) = 0.84 and 0.71, respectively) discontinued the use of contraceptives. Significantly higher rates of discontinuation were pronounced among women who used the pill (OR =0.72) and injectables contraception users (OR = 0.60), had small family size (OR =0.49), lived in a rural community (OR = 1.65), and who were less educated (OR = 1.55).
Conclusions: Contraceptive discontinuation may reflect an association among less education, currently married, and smaller family size. Awareness of contraceptive methods can decrease the burden of unplanned pregnancies and thus progresses the family planning program.
Keywords
Prevalence, Contraceptive discontinuation, Switching, EDHS, Odds ratio.
Introduction
An Explanation and Elaboration article discusses each checklist item and gives methodological background and published examples of transparent reporting. The STROBE checklist is best used in conjunction with this article (freely available on the Web sites of PLoS Medicine at http://www.plosmedicine. org/, Annals of Internal Medicine at http://www.annals.org/, and Epidemiology at http://www.epidem.com/). Information on the STROBE Initiative is available at www.strobe-statement. org as explained in Table 1. Contraception is an effective form of family planning (FP), and over three-quarters of women in developing countries have used a form of contraception during their lifetime.1 Contraceptive discontinuation contributes substantially to unplanned pregnancies, unwanted births, and termination of pregnancies. Every year, about one-third of the 182 million pregnancies occurring worldwide are unplanned [1].
| Item No | Recommendation | Page No | |
|---|---|---|---|
| Title and abstract | 1 | (a) A retrospective cohort study was conducted | #1 |
| (b) The prevalence of discontinuation and switching of contraceptive method among women were found to be 38.4% and 15.4%, respectively. The model demonstrated that women in early reproductive years (20–29 years and 30–34 years) significantly more often (odds ratio [OR] = 0.84 and 0.71, respectively) discontinued use of contraceptives. | #2 | ||
| Introduction | |||
| Background/rationale | 2 | Dynamics of contraceptive use; continuation, switching and failure are important markers of how well programs are meeting the FP needs of women and couples. Time-to-discontinuation and Method Switching of LARCs was modeled. Reasons for discontinuation and Method switching have been LARCs identified. | #4 |
| Objectives | 3 | Specifically, to determine the prevalence of the reversible long-acting contraceptive methods discontinuation among married reproductive age women in Hadiya Zone, Southern Ethiopia from September 2010 to June 2015; to identify factors associated with time-to-discontinuation of reversible long-acting contraceptive methods among married reproductive age women in Hadiya Zone, Southern Ethiopia from September 2010 to June 2015; to model different parametric frailty models and make model comparison using different criteria for time-to-event data. | #4 & #5 |
| Methods | |||
| Study design | 4 | The study design for this study was retrospective cohort | #5 |
| Setting | 5 | The study was conducted in the health facilities of Hadiya Zone, Hosanna, Ethiopia. The time for the inclusion of the data was from September 2010 to June 2015. | #5 |
| Participants | 6 | (a) All women who came to use reversible long-acting contraceptives in one of these Health facilities in Hadiya Zone. | #6 |
| Variables | 7 | Time-to-discontinuation of long-acting reversible contraceptive methods was dependent variable in the study. Age of women; Income (wealth index); Educational status of women (literacy level); Occupation; Residence; Current Marital status (Union, In-union); Paternal education status (literacy level); little access/too far from HFs; unavailability of the method; missed appointment; husband/partner doesn't approve; Method failure (being pregnant while using); side effects; health concerns; difficulty to use; need more effective method; Infrequent Sex/partner not present | #6 |
| Data sources/ measurement | 8* | The sampling was made proportionally from the health facilities according to the prevalence and the number of the cases in each health facility. | #6 |
| Bias | 9 | Two-stage stratified random sampling design was applied with the design effect concept to minimize the variability due to the heterogeneity among the health facilities. | #6 |
| Study size | 10 | Sample size was calculated by using sample size for one population proportion formula. The assumption used for sample size calculation is: For two-stage random sampling method, it was appropriate to assume a design effect of 1.5 and the prevalence of discontinuation of long-acting contraceptive methods among married women of reproductive age is 42.5 according to Mini-EDHS 2014 report; detecting a 2.0 times higher prevalence of discontinuation of long-acting contraceptives; at 95% confidence interval and taking default 80% power. A total of 563 participants were included in the study. | #5 |
| Quantitative variables | 11 | Respondents were classified into two groups: the “discontinued use” group (if they had used a contraceptive method in the past 12 months but were not doing so at the time of the survey) and the “contraceptive switched” group (if their current method differed from their previous method used). | #7 |
| Statistical methods | 12 | (a) Graphs and Tables were used as descriptive statistics and An inferential statistical test was used to assess differences between the two groups of married women, by contraceptive discontinuation or switching status. Survival data analysis specially, parametric frailty models were employed. | #7 |
| (b) Describe any methods used to examine subgroups and interactions | #6, #7 | ||
| (c) No missing data notified | NA | ||
| (d) If applicable, describe analytical methods taking account of sampling strategy | #7 | ||
| (e) Not applied | NA | ||
| Results | |||
| Participants | 13* | (a) Report numbers of individuals at each stage of study—eg numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing follow-up, and analyzed. | #8 |
| (b) Give reasons for non-participation at each stage | NA | ||
| (c) Consider use of a flow diagram | NA | ||
| Descriptive data | 14* | (a) Give characteristics of study participants (eg demographic, clinical, social) and information on exposures and potential confounders | #8 |
| (b) Indicate number of participants with missing data for each variable of interest | NA | ||
| Outcome data | 15* | Report numbers of outcome events or summary measures | #8 & #9 |
| Main results | 16 | (a) Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision (eg, 95% confidence interval). Make clear which confounders were adjusted for and why they were included | #16 |
| (b) Report category boundaries when continuous variables were categorized | #16 | ||
| (c) If relevant, consider translating estimates of relative risk into absolute risk for a meaningful time period | NA | ||
| Other analyses | 17 | Report other analyses done—eg analyses of subgroups and interactions, and sensitivity analyses | NA |
| Discussion | |||
| Key results | 18 | The median time to discontinuation of LARCs and the prevalence of discontinuation and switching of LARCs was one of the major findings; the reason of discontinuation was another finding and discontinuation rate by type of contraceptive methods. | #12 |
| Limitations | 19 | The recall bias was the main challenge among the women who have been under the follow-up. | NA |
| Interpretation | 20 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence | #10 |
| Generalizability | 21 | Contraceptive discontinuation may reflect an association among less education, currently married, and smaller family size. Awareness of contraceptive methods can decrease the burden of unplanned pregnancies and thus progresses the family planning program. | #11 |
| Other information | |||
| Funding | 22 | Office of Vice-president for research and development funded the research | #11 |
Table 1. STROBE Statement—Checklist of items that should be included in reports of cross-sectional studies.
Discontinuation of effective methods of contraception is a universal problem, though rates vary widely by population and country [2]. There are many possible reasons for contraceptive discontinuation, including contraception failure, actual or perceived problems with the contraception method, lack of information, or religious reasons. Low incentive to avoid pregnancy may also be an important factor in some communities. Contraceptive discontinuation is a worldwide incident that may be connected with low incentive to avoid pregnancy. Contraceptive discontinuation highly contributes to unplanned pregnancy and unwanted births. High rates of contraceptive discontinuation for reasons other than the desire for pregnancy are a public health concern because of their association with negative reproductive health outcomes. Despite persistent advocacy urging the use of modern contraceptive methods for FP, the fertility rates in most Sub-Saharan African countries still remains unacceptably high, mostly due to poor uptake of contraception because of cultural, economic, sociodemographic and political barriers [3].
Contraceptive use and fertility rates vary substantially among developing countries. A few countries of Asia and Latin America, at least three-fourths of married women use a contraceptive method. In contrast, in some Sub-Saharan African countries fewer than 10% of married women use contraception. Researchers suggest that fertility rates range from just 2.3 children per woman in Vietnam to 7.2 in Niger in developing countries [4]. According to a report of Marie Stops International, in Ethiopia much of the growth in national contraceptive use has come from an expansion of access to short-term methods. We have been able to complement this success by ensuring that long-acting and permanent methods, as well as short term methods, are available to the women that want them. We have estimated that at the time of the most recent Demographic and Health Survey in 2011 we provided one in three of all the longacting and permanent methods in the country as a whole [5].
Ethiopia has made incredible progress over the last 11 years in increasing access to family planning. In 2000 Ethiopia had a modern contraceptive prevalence rate (modern CPR) for all women of less than 5% but just 11 years that figure had quadrupled to nearly 20%, a truly impressive stride forward for the second-most populous nation in sub-Saharan Africa [6].
Among the many sexual and reproductive health problems faced by women in Ethiopia such as gender inequality, sexual coercion, early marriage, polygamy, female genital cutting, closely spaced pregnancies, abortion, sexually transmitted infections and AIDS [7]. In Ethiopia, 34% of married women had an unmet need for family planning, with 20% having an unmet need for spacing and 14% having an unmet need for limiting [8]. In Ethiopia, the contraceptive prevalence rate for married women who are currently using a method of family planning is 15% which almost all using the modern contraceptives methods [9]. The most widely used methods were Injectables (10%) and pill (3%) Lacks of access and quality of family planning service have devastating maternal health consequences [10].
Statement of the Problem
The impact of family planning depends not only on contraceptive prevalence but also on the method mix and duration and effectiveness of the contraception used.
Dynamics of contraceptive use; continuation, switching and failure are important markers of how well programs are meeting the FP needs of women and couples. Studying the dynamics of contraceptive use can reveal problems in the use of contraceptive technologies and the gaps in the provision of services and, therefore, provide guidance essential for improving services is very important. Discontinuation of use that is not followed by prompt recourse to an alternative method carries the possible implication that the range of readily accessible methods may need to be widened. High discontinuation rates due to perceived or real side-effects require that counseling services, informed choice and method mix [8].
Though we had plenty of researches conducted in the area where we can estimate the prevalence of long acting contraceptive methods; attitudes of females or males towards such practice and even contributing factors for the better performance of such methods, little is investigated about the discontinuation and factors for the failure and switching patterns of contraceptives.
Objectives of the Study
This study is therefore conducted to study factors for discontinuation of such long-acting contraceptive methods in Hadiya Zone, Southern Ethiopia from September 2010 to June 2015. The overall objective of this research was to model time-to-discontinuation of reversible long-acting contraceptive methods among married reproductive age women in Hadiya Zone, Southern Ethiopia from September 2010 to June 2015.
Specific objectives
Specifically, to determine the prevalence of the reversible long-acting contraceptive methods discontinuation among married reproductive age women in Hadiya Zone, Southern Ethiopia from September 2010 to June 2015; to identify factors associated with time-to-discontinuation of reversible longacting contraceptive methods among married reproductive age women in Hadiya Zone, Southern Ethiopia from September 2010 to June 2015; to model different parametric frailty models and make model comparison using different criteria for time-toevent data.
Contraceptive discontinuation contributes substantially to unplanned pregnancies, unwanted births, and termination of pregnancies. According to the study by Ruwaida M. et al 2004, every year, about one-third of the 182 million pregnancies occurring worldwide are unplanned and In Ethiopia mother die due to avoidable causes related to pregnancy and birth complications in which maternal mortality was 871/100,000 live births. Birth control methods have significant role on the reduction of maternal health problem and prevention of maternal mortality [11].
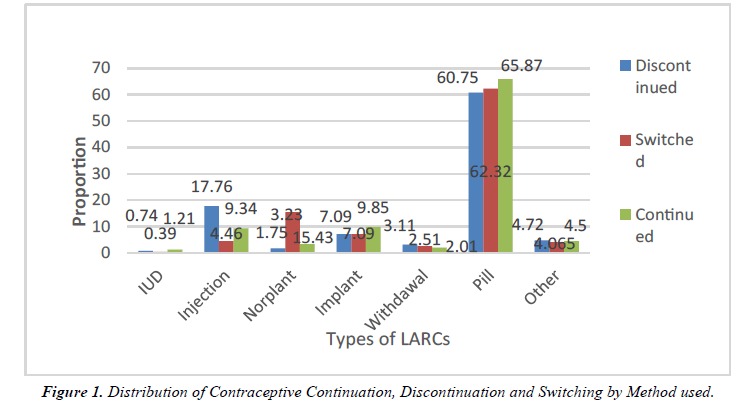
Despite all the commitments and intervention programs being implemented for making situations favorable for the appropriate utilization of family planning methods, still the poor practice of family planning is still a burning issue. This study with overall aim of modeling time-to-discontinuation of long-acting contraceptive methods among married reproductive age women in Hadiya Zone Health Facilities, Southern Ethiopia is expected to find out what factors are determining discontinuation of long acting contraceptive method and will contribute in giving direction for family planning interventions and programs regionally as well as nationally. This methodological study of survival data analysis moreover will help as an input for future work in the area of survival data analysis specially, parametric frailty modeling (Figure 1).
Methodology
Study area and period
The study was conducted in the health facilities of Hadiya Zone, Hosanna, Ethiopia. The time for the inclusion of the data was from September 2010 to June 2015.
Study design
The study design was facility based retrospective cohort study design. Because these mothers/women came for the last 12, 24, or 36 months and were being followed by a physician or health worker at the facility. The subjects included were only married women who came to the facilities for reversible long-acting contraceptive method within the study time interval.
Source population
All women who came to use reversible long-acting contraceptives in one of these Health facilities in Hadiya Zone.
Sampling and sample size determination
Sample size was calculated by using sample size for one population proportion formula. The assumption used for sample size calculation is: For two-stage random sampling method, it was appropriate to assume a design effect of 1.5 and the prevalence of discontinuation of long-acting contraceptive methods among married women of reproductive age is 42.5 according to Mini- EDHS 2014 report; detecting a 2.0 times higher prevalence of discontinuation of long-acting contraceptives; at 95% confidence interval and taking default 80% power:
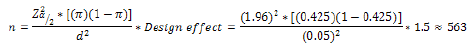
Therefore, the required sample size was estimated to be 563. Based on the nature of study stratified two-stage random sampling became appropriate for this research. The stratification is for the purpose of analysis; we stratify the health facilities of Hadiya Zone as Urban/Hosanna Town and Rural/Woreda Health Facilities. The first stage is when we sample 3 random woredas out of the total. The second stage is selection health centers under the randomly selected woredas. Under urban there are 3 Health Centers and 1 Hospital among these, Hosanna Town Health Center and 1 Hospital which is NEMMH are randomly selected using simple random sampling; under Rural (Health facilities of the 10 woreda, 3 woredas are randomly selected using simple random sampling then, 3 Health Centers under each woreda are selected) and the final study subjects were addressed at each health facility. Accordingly, assuming there is a sort of homogeneity within each health facility we used stratified two-stage random sampling method. Using such method we can estimate proportional number of samples under each stratum. Using proportional allocation on stratified random sampling the following samples are determined under each health facility.
Variables in the study
Time-to-discontinuation of long-acting reversible contraceptive methods was dependent variable in the study.
Here, the event in interest is any form of discontinuation which consists of method switching and the like. Any event other than discontinuation of methods that is censored in this case.
Explanatory variables
Socio demographic factors: Age of women; Income (wealth index); Educational status of women (literacy level); Occupation; Residence; Current Marital status (Union, Inunion); Paternal education status (literacy level).
Service /quality related factors: Little access/too far from HFs; unavailability of the method; missed appointment; husband/ partner doesn't approve.
Method related factors: Method failure (being pregnant while using); side effects; health concerns; difficulty to use; need more effective method; Infrequent Sex/partner not present.
Obstetric factors: Number of living children/parity; previous miscarriage/abortion; sex preference Data processing and analysis
In analyzing the data, both descriptive and inferential statistics were employed. Among the descriptive data analysis tools, frequencies and summary measures were utilized while in inferential part survival data analysis specially, parametric frailty models were employed.
Respondents were classified into two groups: the “discontinued use” group (if they had used a contraceptive method in the past 12 months but were not doing so at the time of the survey) and the “contraceptive switched” group (if their current method differed from their previous method used). An inferential statistical test was used to assess differences between the two groups of married women, by contraceptive discontinuation or switching status. Logistic regression was used to investigate associations between user status and factors that had been previously identified as significantly associated in bivariate analysis, in the literature. The models controlled for married woman’s 5-years age group were analyzed according to the reproductive period (15–49), number of living children (parity), fertility preferences, history of a terminated pregnancy, place of residence, religion, highest education grade completed, and wealth index. Assessment of the strength of these factors as predictors was done using odds ratios (OR) and their 95% confidence intervals (CI) for comparisons of their effect on discontinued use and switching. In the case of multivariate model, Cox proportional Hazards models are performed on the full sample to assess simultaneously the association of individual characteristics, fertility motivation and partner engagement, experience of side effects, service quality indicators, and method characteristics, with the likelihood of discontinuation. Separate models are run for discontinuation of the baseline method and first episode of non-use of any method. In the Cox proportional hazards model, the baseline hazard ratio when all covariates are set to zero equals the odds of an event occurring; the event may occur sooner or later with the addition of covariates. A hazard ratio (HR) below 1.0 means that increases in the covariate reduce the hazard (“risk” or “likelihood”) of the event occurring, while a HR above 1.0 increase the likelihood of the event occurring.
Result
Among a total of 563 women who were enrolled at baseline and 473 of these women (84%) were interviewed at follow-up. No significant differences were found in terms of baseline age, marital status, residence, and method use at baseline between the women interviewed at follow-up and the full sample of women interviewed at baseline.
A profile of the 473 women interviewed at baseline and followup is presented in Table 2. The table shows that the study population is young; the vast majority (94%) is under the age of 35. Most women have had at least some education (94%), with almost 30% having reached a secondary or higher level of education.
| No Discontinuation (59% | One Discontinuation (37%) | Two Discontinuations* (4%) | |
|---|---|---|---|
| -59% | -37% | -4% | |
| Injectable | 56.40% | 39.90% | 3.70% |
| Pills | 51.10% | 44.40% | 4.40% |
| IUD | 72.10% | 23.60% | 4.30% |
| New User | 55.30% | 38.60% | 6.20% |
| =1year use | 61.00% | 38.60% | 2.20% |
| >1 year use | 64.50% | 34.10% | 1.40% |
Table 2. Number of discontinuations during twelve month study period, by method and length of use at baseline, n=563.
Only 3% of the women did not have any children at baseline, while 83% had between one and three children. Being married or in union was common, 89% at baseline (at follow-up, 94 percent were in union).
Approximately 23% of women who were interviewed in the city for the baseline clinic appointment currently resided in a rural area; these rural women may have been in the city for other reasons as well, including attending work or visiting the market. Table 2 indicates that nearly 50% of the women in the panel sample who were using an effective female reversible method of family planning at baseline wanted to space a future birth by two or more years at the time of the baseline interview. Another third of these women wanted no more children. Notably, about 18 percent of women wanted a child soon (within two years) or were undecided about future fertility desires. At follow up, onefifth of the women in this analysis reported that their husband wants more children than they do. The remaining women reported that their husband wants fewer children, the same number, or that they don’t know their husband’s fertility desires.
In this sample, discussion of family planning with partners is common. At the follow-up interview, nearly half of the women reported discussing family planning with their partner three or more times in the last year. Another one-third of the women reported that they discussed family planning one or two times in the last 12 months.
Overall, method-switching occurred for almost one-fifth (18%) of the total study sample. A small percent of women who switched methods went on to discontinue again (4%). Switching occurred more often among new users (22%) and users of less than or equal to one year (19%) as compared to users of more than one year (10%). Method switching was almost equally frequent by baseline method (17% to 19%). Switching to another method included in the study accounted for 72% of switches, with the pill being the most common method switched to (37%), followed by injectable (21%) and the IUD (14%). Compared with the discontinued group, more than 30% women who had switched contraceptive methods were aged 20–24 years, followed by 24.5% in the age range 25–29 years; 46.3% were secondary-level educated; 59.1% had 1–2 children; and 79.9% of women had a pregnancy termination. This group was predominantly “spacers” who wanted to have another child (73.5%). Approximately 61.81% of women who were case response the contraceptive discontinued by former pill users, followed by 18% of injectable contraception users. On the contrary, 66.32% of women who were switched by pill followed by injection users (17.43%). The regression model suggested that place of residence, age, parity, fertility preference, and wealth quintile were shown to be the significant factors for contraceptive discontinuation. The analysis suggested that respondents from the rural community were about two times more likely to discontinue use relative to respondents from the urban community. However, respondents aged 25–34 years old were more likely to have discontinued compared with respondents aged less than 20 years.
The analysis also suggested that respondents with no formal education or illiterate were 1.5 times more likely to have discontinued to use relative to those who had completed higher education. Women who did not intend to have other children were less likely to have discontinued contraceptive use. Previous use of the pill, intrauterine device (IUD), and injection were found to be associated with approximately less than one time the discontinuation which was even higher than that recorded by other acting methods.
Conversely, education, age, parity, fertility preference, place of residence, and wealth quintile were also shown to be the significant predictors for switching of contraceptive method. The analysis suggested that respondents aged 25–34 years old were more likely to have switched compared with respondents aged less than 20 years. Respondents who were secondary level–educated were more likely to have switched contraceptive methods relative to those who had less education. As for fertility preference, respondents who did not intend to have children were more likely to have switched contraceptive methods compared with those who wanted another child. However, the respondents who lived in a rural community were more than 1.6 times more likely to have switched the method compared with those living in an urban community. The respondents of pill, IUD, and injection users were more likely to have switched the contraceptive method as compared with those using other methods.
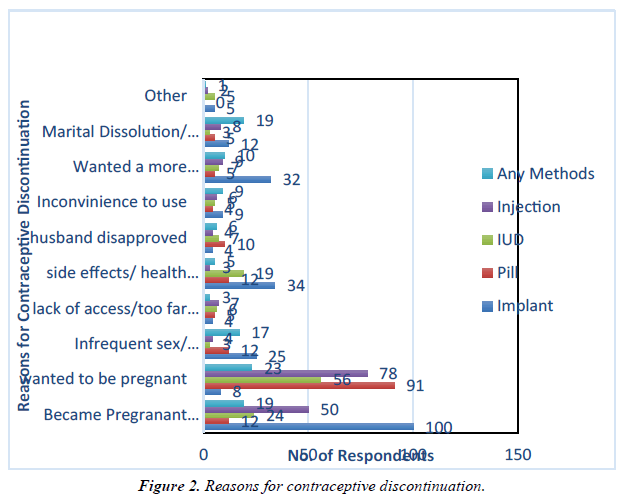
The most common reasons given for discontinuing contraceptive method, regardless of the method currently in use, were desire to conceive, unexpected conception, and side effect or health concern. About one-third (32.87%) of women stopped practicing contraception because they wanted to become pregnant, while about one-quarter (26.69%) were concerned about the side effects (this was especially important for those using the injection method, among whom 50.21% of the discontinuation was attributed to concern of side effects) (Figure 2).
Discussion
The result of the survey revealed that there is no significant difference found in terms of baseline age, marital status, residence, and method use at baseline between the women interviewed at follow-up and the full sample of women interviewed at baseline and supported by results [5].
A profile of the 473 women interviewed at baseline and followup is presented in Table 2. The table 3 shows that the study population is young; the vast majority (94%) is under the age of 35. Most women have had at least some education (94%), with almost 30% having reached a secondary or higher level of education. Only 3 percent of the women did not have any children at baseline, while 83% had between one and three children. Being married or in union was common, 89% at baseline (at follow-up, 94% were in union). Approximately 23 percent of women who were interviewed in the city for the baseline clinic appointment currently resided in a rural area; these rural women may have been in the city for other reasons as well, including attending work or visiting the market where researchers by [11,12]. Notably, about 18% of women wanted a child soon (within two years) or were undecided about future fertility desires which goes in line with the result by (Table 3) [4].
| Background variables | Categories | Discontinuation Adjusted OR (95% CI) | Switching Adjusted OR (95% CI) |
|---|---|---|---|
| Age | 15 -- 20 (Ref) | ||
| 21 -- 25 | 0.81 (0.56 – 1.02) | 1.47 (1.11 – 2.13) | |
| 26 -- 30 | 0.65*** (0.71 – 1.55) | 1.78* (0.14 – 3.56) | |
| 31 – 35 | 0.64** (0.54 – 0.78) | 0.94** (0.54 – 1.76) | |
| 36 – 40 | 0.67 (0.45 – 0.79) | 1.15 (1.12 – 7.96) | |
| 41 – 45 | 0.88** (0.56 – 1.02) | 0.78 (0.54 – 3.56) | |
| 46 – 49 | 0.84 (0.75 – 1.25) | 1.55 (0.94 – 4.76) | |
| Education Status | Illiterate (Ref) | ||
| Primary | 1.23* (0.34 – 1.56) | 0.78 (0.54 – 1.56) | |
| Secondary | 1.04** (0.94 – 1.26) | 1.50** (0.94 – 1.76) | |
| College and Higher | 0.45* (0.42 – 0.96) | 0.44***(0.12 – 0.96) | |
| Place of Residence | Urban (Ref) | ||
| Rural | 1.47*** (1.11 – 2.13) | 0.97** (0.64 – 1.73) | |
| Religion | Orthodox | 1.78 (0.14 – 3.56) | 0.78 (0.25 – 3.56) |
| Catholic | 1.94 (0.94 – 4.76) | 1.04 (0.94 – 1.66) | |
| Protestant | 0.15 (0.12 – 7.96) | 1.15 (0.62 – 4.96) | |
| Islam (Ref) | |||
| Socio-Economic Status | Poorest (Ref) | ||
| Poor | 0.78** (0.54 – 1.56) | 1.08 (0.84 – 1.56) | |
| Rich | 1.53 (0.94 – 4.76) | 0.43 (0.04 – 0.76) | |
| Richest | 0.54 (0.12 – 2.96) | 1.05 (0.12 – 2.96) | |
| Live Birth/ Parity | None (Ref) | ||
| 1 – 2 | 0.98** (0.54 – 1.06) | 1.18* (1.0 – 2.66) | |
| 3 – 4 | 0.53 (0.94 – 4.76) | 0.13 (0.10 – 0.76) | |
| 5 and more | 2.54 (1.12 – 2.96) | 1.04 (0.13 – 2.06) | |
| Notes: *P<0.10; **P<0.05; ***P<0.01 | |||
Table 3. Factor association for discontinued contraceptive use and switching, by selected socio-demographic characteristics.
Conclusion
Contraceptive discontinuation may reflect an association among less education, currently married, and smaller family size. Awareness of contraceptive methods can decrease the burden of unplanned pregnancies and thus progresses the family planning program.
What is already know on this topic
The median time to discontinuation of long acting reversible contraceptive methods was one of the major findings; the reason of discontinuation was another finding and discontinuation rate by type of contraceptive methods.
What this study adds
This study adds knowledge on the time to discontinuation of long acting reversible contraceptive methods identifying the major reasons of discontinuation and discontinuation rate by type of contraceptive methods.
Competing Interests
The authors declare no competing interest.
Authors’ contributions
AA and ND incepted the concept of the research; they both analyzed and wrote the manuscript.
Acknowledgments
We are grateful to Wachemo University for their unrestricted support in conducting this research. The authors would also like to thank Hadiya Zone and Woreda Health Offices. Last, but not least, we are so grateful for the Research and Development Directorate office.
References
- USAID. (2004). Assessment of Youth Reproductive Health / HIV Programs in Ethiopia. In Usaid (Issue September).
- Belete N, Zemene A, Hagos H, et al. Prevalence and factors associated with modern contraceptive discontinuation among reproductive age group women, a community based cross-sectional study in Humera town, northern Ethiopia. BMC Women's Health. 2018;18(1):1-8.
- Thobani R, Jessani S, Azam I, et al. Factors associated with the discontinuation of modern methods of contraception in the low income areas of Sukh Initiative Karachi: A community-based case control study. PloS One. 2019 ;14(7):e0218952.
- Seiber EE, Bertrand JT, Sullivan TM. Changes in contraceptive method mix in developing countries. International family planning perspectives. 2007:117-23.
- Yifru GT, Haileyesus MT, Regassa BT. Determinants of Modern Contraceptive Methods Discontinuation among Women within Reproductive Age in Dire Dawa City, Eastern Ethiopia. Int J Reprod Med. 2020.
- Macro OR. Central Statistical Agency. Ethiopia demographic and health survey. 2005.
- Asnake M, Walie L, Melkamu Y. Improving the range of contraceptive choices in rural Ethiopia. Ethiop J Health Dev. 2006;20(2):74-8.
- Mekonnen G, Enquselassie F, Tesfaye G, et al. Prevalence and factors affecting use of long acting and permanent contraceptive methods in Jinka town, Southern Ethiopia: a cross sectional study. Pan Afr Med J. 2014;18(1).
- Megabiaw B. Awareness and utilization of modern contraceptives among street women in North-West Ethiopia. BMC Women's Health. 2012;12(1):1-7.
- Kebede Y. Contraceptive prevalence and factors associated with usage of contraceptives around Gondar Town. Ethiop J Health Dev. 2000;14(3).
- Bekele D, Surur F, Nigatu B, et al. Contraceptive prevalence rate and associated factors among reproductive age women in four emerging regions of Ethiopia: a mixed method study. Contracept and Reprod Med. 2021;6(1):1-3.
- Mahumud RA, Hossain MG, Sarker AR, et al. Prevalence and associated factors of contraceptive discontinuation and switching among Bangladeshi married women of reproductive age. Open Access J Contracept. 2015;6:13.
Indexed at Google Scholar Cross Ref
Indexed at Google Scholar Cross Ref
Indexed at Google Scholar Cross Ref
Indexed at Google Scholar Cross Ref
Indexed at Google Scholar Cross Ref
Indexed at Google Scholar Cross Ref
Indexed at Google Scholar Cross Ref