Commentary - Journal of Pain Management and Therapy (2017) Volume 1, Issue 2
The surveillance system, diagnosis and treatment challenges of asthma and health policy orientation of main challenges.
Seyyede Masoume Athari1, Faride Afshari2, Asie Eftekhari3, Seyyed Shamsadin Athari4*
1Department of Biology, Faculty of Basic Sciences, Maragheh University, Maragheh, Iran
2Department of Immunology, Faculty of Medical Sciences, Tarbiat Modares University, Tehran, Iran
3Department of Psychology, Zanjan Branch, Islamic Azad University, Zanjan, Iran
4Department of Immunology, Faculty of Medicine, Zanjan University of Medical Sciences, Zanjan, Iran
- Corresponding Author:
- Seyyed Shamsadin Athari
Zanjan University of Medical Sciences
Iran
Tel: + 989120656451
E-mail: SS.Athari@zums.ac.ir
Citation: Athari SM, Afshari F, Eftekhari A, et al. The surveillance system, diagnosis and treatment challenges of asthma and health policy orientation of main challenges. J Pain Manage Ther. 2017;1(2):1-5.
Abstract
Asthma is a chronic inflammation of the airway and has affected 300 million individuals throughout the world which causes 250000 deaths per year. Asthma occurs in all age groups and the produced drugs cannot prevent asthma but also have systemic side effects. Healthcare costs related to asthma in average are more than US$500 per emergency visit and US$2000 per hospitalization. Asthma imposes direct and indirect costs. The objective of this study is focusing on the main challenges of asthma. An observational study was designed in primary care settings in Iran in order to determinate the main challenges of surveillance system, diagnosis, control and treatment of asthma. According to our searches from ministry health database, about 6.5 million people in Iran are asthmatic and more than 3.2 billion US$ is spent on asthmatic patients in Iran. Main challenges, plans and actions for asthma are listed. The direct costs represented about 30% of the total costs and the indirect costs is hidden and is the main part of costs. The high morbidity and mortality rates of asthma should be added to these costs. Health policy should emphasis on improving asthma control which can be beneficial for the patients, their families, even though the economies of countries as reductions in the cost of asthma care and increases in productivity.
Keywords
Challenges, asthma, health policy.
Introduction
Asthma is a complicated chronic inflammation of airway and is widespread in whole of the world, especially in developed countries and 300 million individuals are affected throughout the world which causes 250000 deaths per year. The symptoms of asthma are airway inflammation, bronchoconstriction, and airway remodeling with cough, dyspnea and wheezing that reduces quality of life with the health’s risk for people [1,2]. Parallel of Genetic, epigenetic and environmental factors have important roles in asthma’s pathophysiology. Industrial/ manufacturing living with air pollution, fast food using and overweight/obese, geo-environmental changes, new chemical compounds and other factors lead to increase asthma induction. Asthma occurs in all age groups and the produced drugs cannot prevent asthma but also have systemic side effects. It is one of the causes of substantial mortality and morbidity and is associated with high direct and indirect health costs [3,4].
The main goal of asthma treatment is to control asthma. Asthma’s control was significantly associated with costs and health-related quality of life. Hospitalizations and emergency visits for asthma associated costs were higher in patients and anti-asthmatic drugs were the main driver of direct costs. Healthcare costs related to asthma are average more than US$500 per emergency visit and US$2000 per hospitalization [5]. With indirect costs such as workdays lost, the total cost of poorly controlled asthma is much higher [6]. A study found that in the USA in 2007 the annual direct medical expenditure for asthma treatment was 37.2 billion US dollars [7,8]. Controller medication using and the education of patients, family and school health personnel is very important in asthma control. Cost-saving efforts should be focused on improving asthma control.
Therefore, asthma imposes direct costs (diagnosis, treatment and control) and indirect costs (work power inefficient and ineffectiveness, time losing of patients, their family and health system, using of facilities and equipment etc.) [9,10]. The objective of this study is focusing on the main challenges of asthma that have association with direct and indirect costs. These costs due to the main challenges can give us new vision and applicable program for prevention of damages and disadvantages of this field in Iran.
Study Design
An observational study was designed in primary care settings in Iran in order to determinate the main challenges of surveillance system, diagnosis, control and treatment of asthma. Consultation with allergist, specialist and asthma expert subspecialists, patient and health care personals interview (adults aged 18 or over, diagnosed with asthma for at least 12 months and having received at least one anti-asthmatic drug within the past 12 months), data were collected form database and datasheet of Ministry of Health and Governance and also hospital information databank were used.
Finding
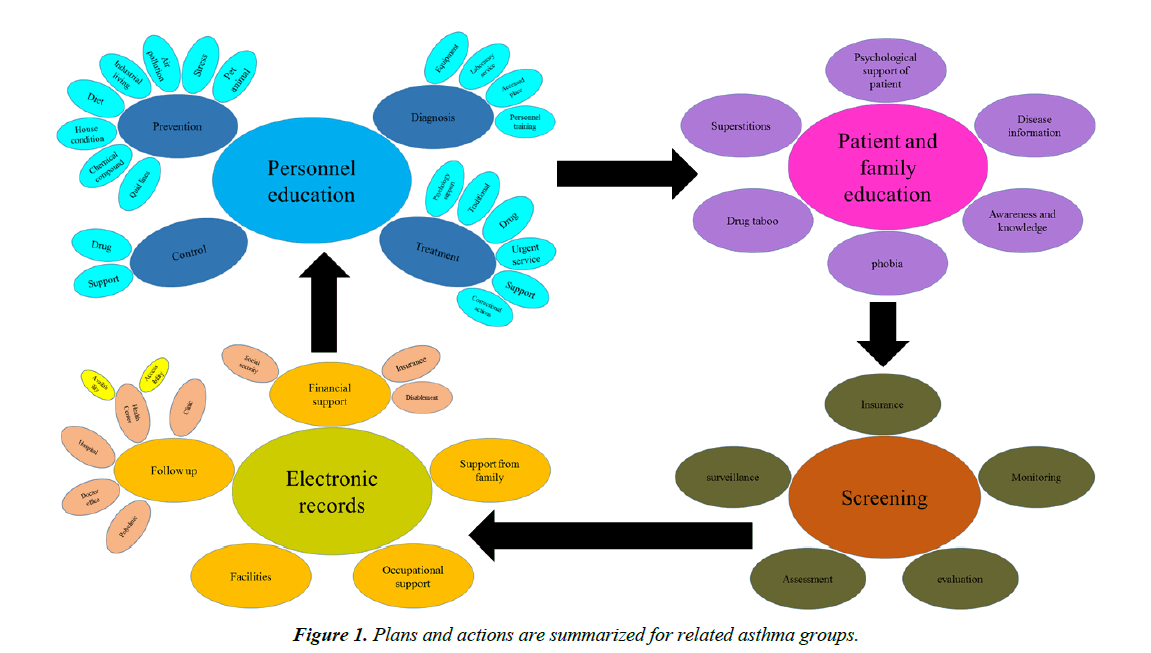
According to our searches from ministry health database, about 6.5 million people in Iran are asthmatic. If only emergency visit healthcare costs related of asthma is considered (average more than US$500 per patient), more than 3.2 billion US$ are spend for asthmatic patients in Iran and other costs are ignored, while the sum rate is very higher. Due to the cultural, political, social and economic condition in Iran, some challenges are important. In the Table 1 main challenges are listed. In the Table 2 some of the steps and plans for resolving the asthma challenges are categorized. In Figure 1 plans and actions for all the groups, who are related to asthma, are summarized.
| Prevention | Patients and Family | Uncorrected house and living place with allergenic condition | With announcing and education of patient's family with updated learning methods. |
| Not attention to food and sport | |||
| Self-care and Personal Health education are not done | |||
| Diseasepreventioneducationneedsfundamentalreform. | |||
| mental health of people is not ready to corporation with health system | |||
| There are no screening programs | |||
| Health care system | Uncontrolled air pollution | ||
| Food safety and necessary food using does not have monitoring | |||
| Diagnosis | Patients and Family | Not returning of patient | |
| Uncooperative patient | |||
| Uncontentious cooperative family | |||
| Health care system | Weakness ofDiagnosis structures(equipment, spaceandfacilities, laboratory services, etc.) | ||
| Rural people lack access to specialist | |||
| Rural people lack access to diagnostic service | |||
| Treatment | Patients and Family | Uncooperative patient | |
| Induced demand for health services in public facilities | |||
| Health care system | Weakness oftreatmentstructures(equipment, spaceandfacilities, drugs, para-clinic services, etc.) | ||
| Rural people lack access to specialist | |||
| Surveillance and Control | Health care system | The lack of electronic files of patients and insufficient records | |
| Experiencedandefficientmanpoweris low | |||
| Surveillance, monitoring and evaluationforthequality, safety, effectiveness, efficiency, productivity and promotionis not perfect | |||
| Psychological and Emotional support of patients by Psychologist is necessary | |||
| Cultural, social and educational of people are incompatible with some programs (such as the use of spray form of drug instead of injection) | |||
| Health Information Technology is not organized | |||
| Financial support and insurance coverage are insufficient. | |||
| Poverty and financial difficulties of people | |||
| Not time spending by patients' families for attention to this disease | |||
| To escape of psychological burden and stress of asthma, people ignore it and deny | |||
| equity, management and responsibility are main challenges from bed to bedside of health system | |||
Table 1. Main challenges of asthma.
| Vision | Reducethe increasingincidence ofasthma |
| Improve the quality life ofpatients withasthma | |
| Reducedeathsdue toasthma | |
| Reduce theeconomic burdenofasthma | |
| Strategies | Increasingpublicknowledgeaboutasthmaandrisk factors |
| improvedasthmasurveillancesystem making | |
| PromotionManagement (prevention, early detection, treatmentandfollow-up) of asthma in health care system | |
| increasing of Intersectionalcooperationandstrengthensupport mechanisms (insurance, charitable...)monitoring and control ofrisk factors | |
| Mainactivities | Trainingfocused onspecificpopulation groups |
| Diagnosis, treatmentandcareof patients withasthmabased onfamily physician | |
| Startingrecording and reportingsystembasedfamily physician | |
| Set upregistrationand reportingsysteminhospitals andemergencycenters | |
| Public Informing | |
| Asthmascreening inhigh-riskgroups | |
| Identification ofrisk factors forasthma | |
| Educate and empowerhealthcare workers | |
| Appliedresearches doing | |
| Standardization ofdiagnosis and treatment | |
| Rulesand credit allocation for IT development | |
| Costs management | |
| Improve the quality ofcare | |
| Electronic patientrecords | |
| Respectingthe confidentiality ofpatient information |
Table 2. Steps and plans for resolve of asthma challenges.
Discussion
According to WHO report, the world in each year, loses 15 million people/ life years for asthma. Asthma is the most common diseases in the world and is ranked 25th terms of years lost (disability caused by the disease). Since asthma is very highly prevalent in all population of the world, numerous studies have addressed the economic burdens of the disease in different countries [11,12]. The direct costs represented about 30% of the total costs and therefore indirect costs are hidden and have main part of costs. Both direct and indirect asthma related costs are increasing [13,14]. These costs increase dramatically with the disease severity and according to Batlles et al study, both costs ranging from $1336 per year in mild asthma to $6393 per year in patients with severe asthma and they estimated that the mean annual total cost of asthma per patient is $2879 [15]. Their study was in 1998 and now these costs should be raised in parallel with the life condition changing.
The direct costs include medications, clinic and emergency visits, admissions to hospital, diagnostic and laboratory tests and transportation costs. Indirect costs are calculated only for workdays lost due to visits to health care facilities [16,17]. In indirect costs, Psychological burden, family time lost, health personnel time lost, depreciation of equipment, hospital space occupancy and etc. are not calculated.
Workdays lost of patients includes three aspects, work missed days due to asthma symptoms (approximately 1.5 days in a month on average), work attended days with asthma symptoms (approximately 5 days in a month on average), decreased productivity level in work (approximately 3.4 days in a month on average) which represents an average monthly labor cost of €285.81 per patient [16-18]. The high morbidity and mortality rates of asthma should be added to these costs. Economic impact is correlated with disease severity. Low income in poor families leads to weak managing and low control of asthma which is correlated with increased severity of the disease, making vicious cycle in applying for economic and societal support with low income.
Family have the main role in management of asthma especially in children. In state of children's severe asthma informed family can control children's asthma better and have more attention to children.
The Global Initiative for Asthma (GINA) and the United States National Asthma Education Prevention Program (NAEPP) revised the guidelines, they suggest to prevent and control asthma symptoms normal daily activity levels should be kept [19-21]. Many parts of these orders have been mentioned but some of others are important in Iran and should be given more attention. Health policy should emphasis on improving asthma control which can be beneficial not only for the patients and their families but also the economies of countries as a whole as reduction in the cost of asthma care and increase in productivity. The personal asthma action plan should be consisted of instructions for medication, a list of asthma triggers, responses to worsening symptoms, and benchmarks to indicate the level of asthma control. Typical plans also include instructions to deal with emergencies such as asthma attacks. Learning as much as possible about asthma will help to manage the condition properly. People should know about the symptoms causes’, how to prevent them, and how to use medicines correctly. Information gathered over time can be used to track changes and progress.
Between 80 and 85 per cent of people who have asthma also have allergies. If we can find out what they’re allergic to and avoid those triggers that can be a good way to control the disease. Identifying and avoiding asthma triggers will help to maintain an active and healthy lifestyle with asthma. The following list discusses common triggers and suggesting ways to handle them: tobacco smoke, air pollution, pollen, animal dander, viral infections, heavy exercise, stress, dry or cold air, dust mites, sulfites in dried food and wine, combustion particles, deodorants, perfumes, air fresheners, and cleaners. One of the most challenging issues is to get good environmental control. Exercise and physical activity are common triggers of symptoms in patients with asthma, although some individuals may have symptoms with exercise alone. Check-ups are usually recommended every 6 to 12 months for mild intermittent or mild persistent asthma that has been well-controlled for at least 3 months. Those with moderate persistent asthma should be checked up every 3 to 6 months, and those with uncontrolled or severe persistent asthma should be checked every 1 to 2 months. [22,23]. Asthma with complicated conditions, has many phenotypes and each phenotype requires specific approaches for control. For many clinicians, it is not practical to differentiate between phenotypes. Well defined phenotype of asthma, lead to a more successful treatment. The example of this determination is the presence of eosinophils in sputum as the marker for targeted treatment, can lead to asthma treatments and control. Another subtype in the asthma category is hyper responsiveness airway (AHR) [24,25].
At the end, patients with asthma have personal challenges. Most people have insurance that only cover a generic medication, but they may need a large number of non-generic medications, too. Most asthma medications are not generics. When someone refers to an allergy and asthma clinic for the first time, the visit averages tales 2-3 hours long, of which testing is going to take approximately 45 minutes long. The rest of the time is spent on teaching patients about their asthma; how to use inhalers, triggers and what to do when they get really short of breath. They especially learn about their new condition. For example, when the controller medication is started, many patients concerns about the side effects of the steroids they have heard about. Many patients will stop their controller medication when they feel better but then they will have a severe flare up and wind up on an oral steroid to manage the exacerbation [26-29].
Operational problems in this study were as follows. Difficult access to the needed information, not getting enough information, low cooperation of some officials, no full compliance available data and information with national and international resources. Higher asthma morbidity and mortality rates have deep association with geographical areas of lower socio-economical standing and changes in life style. Asthma cannot be cured, but it can be controlled. With good management, people with asthma can prevent asthma symptoms and maintain normal daily activity levels. Managing patients with severe asthma is complex and requires a multidisciplinary approach with standardized protocol. Health care of asthma requires a multilevel framework for integrating clinical practice and patient self-management. First step should be focus on saving asthmatic patients’ life then improving quality of Life. In this way, drug potential side-effects such as myelo suppression, hepatotoxicity and etc. should be considered. The asthma guidelines for patients, family and health care system should include daily, weekly and seasonal management. The asthma guidelines with Educational package, should recommend information about asthma at every opportunity in the office, clinic, emergency department, school, home, etc. in this approach, self-monitoring is important and the patients should be able to assess levels of asthma control, recognize signs and symptoms of asthma. Therefore, all patients with asthma should receive a written asthma plan, initial assessment of asthma severity, periodic follow-up visits, recommendations to reduce relevant exposures, basic and accurate foundation of knowledge about asthma, understanding the treatment approach, and having the self-management skills to monitor the disease and take medication effectively. Population health strategies should be applied to improve asthma that include: assure guidelines-based medical management, educate for self-management, facilitate home visits, establish linkages across health sectors, long-term support through evaluation and monitoring, regular controller treatment, a stepwise approach to treatment.
References
- Athari SS, Omidi R. Report of a patient with complex composites of hepatitis B virus, allergic asthma and diabetes. Asian Pac J Trop Biomed. 2014;4(1):S59-61.
- Baïz N, Annesi-Maesano I. Is the asthma epidemic still ascending? Clin Chest Med. 2012 ;33(3):419-29.
- Athari SS, Athari SM. The importance of eosinophil, platelet and dendritic cell in asthma. Asian Pac J Trop Dis. 2014; 4(1):41-7.
- Jankowska-Pola?ska B, Ple?niak J, Se? M, et al. Importance of education in bronchial asthma treatment—gender differences. Pneumonologia i alergologiapolska. 2015;83(5):341-7.
- Weiss KB, Sullivan SD. The health economics of asthma and rhinitis. I. Assessing the economic impact. J Allergy ClinImmunol. 2001;107:3-8.
- Birnbaum HG, Berger WE, Greenberg PE, et al. Direct and indirect costs of asthma to an employer. J Allergy ClinImmunol. 2002;109:264-270.
- Kamble S, Bharmal M. Incremental direct expenditure of treating asthma in the United States. J Asthma. 2009;46:73-80.
- Al-Rawas OA, Al-Riyami BM, Al-Kindy H, et al. Regional variation in the prevalence of asthma symptoms among Omani school children: Comparisons from two nationwide cross-sectional surveys six years apart. Sultan Qaboos University Med J. 2008;8:157-64.
- Kroegel C, Wirtz H: History of guidelines for the diagnosis and management of asthma: from opinion to control. Drugs 2009, 69(9):1189-1204.
- Cisternas MG, Blanc PD, Yen IH, et al. A comprehensive study of the direct and indirect costs of adult asthma.J Allergy ClinImmunol. 2003;111:1212-18.
- Movahedi M, Haghdoost AA, Pournik O, et al. Temporal variations of health indicators in Iran comparing with other Eastern Mediterranean Region countries in the last two decades. J Public Health (Oxf).2008; 30(4):499-504.
- Bahadori K, Doyle-Waters MM, Marra C, et al. Economic burden of asthma: a systematic review. BMC Pulm Med. 2009;9:24.
- Serra-Batlles J, Plaza V, Morejon E, et al. Costs of asthma according to the degree of severity. EurRespir J. 1998;12:1322-6.
- Ungar WJ, Coyte PC. Measuring productivity loss days in asthma patients.The Pharmacy Medication Monitoring Program and Advisory Board.Health Econ. 2000;9:37-46.
- Serra-Batlles J, Plaza V, Morejón E, et al. Costs of asthma according to the degree of severity. EurRespir J. 1998;12(6):1322-6
- Weiss KB, Gergen PJ, Hodgon TA. An economic evaluation of asthma in the United States. N Engl J Med. 1992;326:862-6.
- Stewart WF, Lipton RB, Simon D. Work-related disability: results from the American migraine study. Cephalgia.1996;16(4):231-8.
- Gisbert R, Brosa M. eSalud Sanitary costs database. Barcelona: Oblikue Consulting, S L; 2011.
- Revised 2010 Global strategy for asthma management and prevention.
- Busse WW, Boushey HA, Camargo CA, et al. Expert panel report 3: Guidelines for the diagnosis and management of asthma. Washington, DC: US Department of Health and Human Services, National Heart Lung and Blood Institute. 2007:1-417.
- Masoli M, Fabian D, Holt S, et al. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy. 2004;59:469e78.
- Christopher CJ. Current challenges in asthma.Br J Gen Pract. 2007; 57(536):179- 80.
- LødrupCarlsen KC, Haahtela T, Carlsen KH, et al. Integrated Allergy and Asthma Prevention and Care: Report of the MeDALL/AIRWAYS ICPs Meeting at the Ministry of Health and Care Services, Oslo, Norway. Int Arch Allergy Immunol. 2015;167(1):57-64.
- Lötvall J, Akdis CA, Bacharier LB, et al. Asthma endotypes: a new approach to classification of disease entities within the asthma syndrome. J Allergy ClinImmunol. 2011;127(2):355-60.
- McGrath KW, Icitovic N, Boushey HA, et al. A large subgroup of mild-to-moderate asthma is persistently noneosinophilic. Am J RespirCrit Care Med. 2012;185:612-19.
- Sagar S, Akbarshahi H, Uller L. Translational value of animal models of asthma: Challenges and promises. Eur J Pharmacol. 2015;759:272-77.
- PavordIan D, BushA, Holgate S. Asthma diagnosis: addressing the challenges. Lancet Respir Med. 2015;3(5):339-41.
- ButzAM, KubJ, Bellin MH, et al. Challenges in Providing Preventive Care To Inner-City Children with Asthma. NursClin North Am. 2013;48(2): 241-57.
- Baptist AP, Hamad A, Patel MR. Special challenges in treatment and self-management of older women with asthma. Annals of Allergy, Asthma and Immunology 2014;113(2):125-30.