Research Article - Biomedical Research (2017) Volume 28, Issue 18
The relationship of perceived susceptibility and self-efficacy with the decayed, missing, and filled teeth in pregnant women: a study based on the health belief model
Mehri Hosseintalaei1, Hossein Shahnazi2* and Mehrshad Mohammadi3
1Department of Health Education and Promotion, School of Health, Isfahan University of Medical Sciences, Isfahan, Iran
2Department of Health Education and Promotion, School of Health, Isfahan University of Medical Sciences, Isfahan, Iran
3Department of Endodontics, Hamadan University of Medical Sciences Faculty of Dentistry, Hamadan, Iran
- *Corresponding Author:
- Hossein Shahnazi
Department of Health Education and Promotion,
School of Health, Isfahan University of Medical Sciences, Isfahan, Iran
Tel: +983137923243; 9133360148,
E-mail: h_shahnazi@yahoo.com
Accepted on August 27, 2017
Abstract
Background: Oral and dental health is one of the most significant branches of public health and its role in enhancing public health has been so much instrumental. The present study was conducted to explore the association of perceived susceptibility and self-efficacy with the decayed, missing, and filled teeth (DMFT) index in pregnant women.
Methods: The study population of the present cross-sectional descriptive-analytical study included 300 primiparous women in the first trimester of pregnancy. They had referred to private offices in Delfan in 2015. The data-collection tool was a questionnaire with three parts, namely demographic data, a DMFT checklist, and questions concerning knowledge, perceived susceptibility, and perceived self-efficacy, as three constructs of the health belief model (HBM). Data were analyzed using Pearson’s correlation coefficient, Spearman’s correlation coefficient, and the independent t-test (α<0.05).
Results: The mean age of the pregnant women in the study was 23.1 ± 3.9 years and their mean gestational age was 9.7 ± 2.9 weeks. Their mean DMFT index was 7.46 ± 4.59. The means of their decayed, missing, and filled teeth were 4.98 ± 3.38, 1.44 ± 2.39, and 1.07 ± 2.05, respectively.
Conclusion: This study revealed that the three constructs in the pregnant women were related to the DMFT index. Hence, by training pregnant women in oral and dental health based on the HBM constructs, we can increase their susceptibility and self-confidence in order to prevent the increase in the DMFT index and promote oral and dental health care behaviors among them.
Keywords
DMFT index, Pregnancy, Oral health, Self-efficacy.
Introduction
Oral and dental health is among the most important branches of public health. One of the primary goals of Healthy People 2010 was to increase adults’ access to oral health services annually [1]. The World Health Organization (WHO) regards oral and dental health as a necessity and a vital element of public health in the entire lifetime and believes that poor oral health can have dramatic effects on the quality of life. The role of oral and dental health in ensuring and promoting public health has been acknowledged in such a way that it is now considered to be one of 11 main goals in the 21st century [2,3]. Moreover, one of the aims the WHO had pursued up until 2010 was to reduce caries by 15% and gum diseases (periodontal diseases) by 48% for the 35-44 age range [3]. Dental caries (tooth decay) is among the most common diseases affecting humans and is never restricted to a specific age, gender, race, geographical area, or period [4]. Due to particular physiological conditions, some groups are more susceptible to dental caries. For instance, hormonal and nutritional changes render pregnant mothers liable to caries and periodontal diseases. Definitely, health care delivered easily in normal circumstances is likely to face problems in pregnant women’s case. Owing to this, the majority of pregnant women, particularly those ensuring partial compliance with oral and dental health prior to pregnancy, may suffer from severe dental pain and increased dental caries during pregnancy. Hence, certain circumstances during pregnancy require more oral and dental care and disregard for this essential would not only cause oral and dental health problems but also endanger the health of other body systems and the fetus [5-7]. Various studies on dental caries have been conducted worldwide [8]. They report that the prevalence of dental caries in pregnancy is 23-43%. Some studies reveal that dental care in pregnant women is at a low level so that 58-65% of them overlook oral and dental health care and their performance is not in favorable conditions [9-13]. The mean decayed, missing, or filled teeth index (hereafter DMFT) is higher among pregnant women than among other people in the community so that, according to a study, the mean DMFT among Brazilian pregnant women was 12.51 ± 4.21 and only 6.3% of the study population had no dental caries [14]. In another study on Italian pregnant women, the mean of DMFT was 7.9 ± 4.2 [15]. A study demonstrated that the oral and dental health condition among pregnant women in Ahvaz, Iran, was average and their mean DMFT was 6.23 ± 3.01. Furthermore, a different study in Arak, Iran, reported that the mean of mothers’ oral and dental health behavior in that city was below average (43 out of the total score of 100) and their mean DMFT was 5.4 ± 2.83 [16,17]. In a study on pregnant women in Isfahan, the mean of DMFT was found to be 10.6 ± 4.21 [18]. According to studies by Thomas et al. and Shamsi et al., over half of pregnant women had not been visited by a dentist during their most recent pregnancy. These statistics show the presence of a poor oral and dental health culture among pregnant women, which necessitates the development of appropriate solutions [19,20]. Prevention is the most important way to reduce dental caries. The first step in prevention is to foster a culture of health and prevention among people so that, as indicated in a study, we can reduce some cases of oral and dental diseases by 80% through health education but 20% of cases are beyond our control [14]. The effectiveness of health education programs largely depends on the proper application of theories and models used in health education. In fact, better theoretical frameworks and more fundamental health needs lead to more effective health programs [21]. One of the effective models for health education and prevention is the health belief model (HBM), used in the field of preventive health behaviors. According to this model, individuals adopt preventive health behaviors when they believe they are at risk of a disease (perceived susceptibility) and the disease may lead to deleterious consequences (perceived severity). Furthermore, there are behaviors which help prevent a disease or reduce its severity and complications (perceived benefits); however, there are physical, mental, or financial barriers to the performance of these behaviors (perceived barriers). On the other hand, in order to perform a behavior, individuals should perceive themselves to be capable of performing preventive behaviors (perceived self-efficacy) [22]. Positive effects of perceived susceptibility and perceived self-efficacy on oral and dental health care behaviors and DMFT have been confirmed [15,23-25].
Considering the increase in the mean of DMFT during pregnancy, the vulnerability of pregnant mothers, effects of poor oral and dental health on pregnancy (which could result in low birth weight, preterm delivery, and preeclampsia, for example), and the significance of preventing primary dental caries in children and reducing caries in adolescence [6,26-30], the present study aimed to explore the relationship of perceived sensitivity and self-efficacy to DMFT in pregnant women from Delfan, Iran.
Materials and Methods
The present research was a cross-sectional descriptiveanalytical study. The study population included 300 primiparous women who were in the first trimester of pregnancy and had attended private offices in Delfan in 2015. From eight private offices in this city which were geographically and culturally the same, four were randomly selected. First, 300 pregnant women were chosen from these four private offices using simple random sampling and were included in the study. Then, objectives of the study were explained to them and they were assured that their data would be kept confidential. To be included in the study, the subjects had to provide informed consent and have basic literacy skills. Exclusion criteria were engagement in dentistry-related occupations, lack of interest in the study, failure to complete the questionnaire, and suffering from any oral and dental disease or any progressive gum disease. In the present research, the reason for selecting primiparous women was that, generally, women who give birth for the first time have never been trained by a midwife and also have no personal experience; moreover, they have no dental changes caused by a previous pregnancy.
The sample size was calculated at 298 minimum according to the following equation
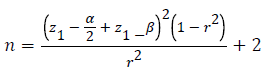
In this equation, n = sample size, α = error rate (set at 0.05;
hence,  1–β=test power (set at 0.80;
hence,
1–β=test power (set at 0.80;
hence,  , and r=correlation coefficient
between the HBM constructs and DMFT (0.16 minimum in a
preliminary study on 30 subjects).
, and r=correlation coefficient
between the HBM constructs and DMFT (0.16 minimum in a
preliminary study on 30 subjects).
Data were gathered using a three-part questionnaire. Part 1 comprised demographic data, including age, gestational age (GA), educational status, income level, insurance coverage, and employment status. Part 2 consisted of a DMFT checklist, which was based on the WHO report [30] and included questions about the rate of decayed, missing, and filled teeth. Part 3 was composed of questions concerning the HBM constructs (15 questions on knowledge, eight questions on perceived susceptibility, and nine questions on perceived selfefficacy). As for the scoring of the questionnaire, it should be remarked that correct and incorrect responses to knowledge questions were scored 1 and 0, respectively, and the total score ranged from 0 to 15. Responses to questions about perceived susceptibility and self-efficacy were scored from 0 to 4 (0=“Totally disagree”, 1= “Disagree”, 2= “Don’t know”, 3= “Agree” and 4= “Totally agree”). The total score for perceived susceptibility ranged between 0 and 32; however, the total score for perceived self-efficacy ranged from 0 to 36. This questionnaire had been used in a study by Shamsi et al. in 2012 and its content validity was confirmed to be >0.79 [17]. As for its reliability, it should be mentioned that Cronbach’s alphas for perceived susceptibility and self-efficacy were 0.73 and 0.76, respectively; moreover, Cronbach’s alpha was >0.7 for each construct and dimension in the study by Shamsi et al. [15]. Hence, the tool reliability was at an acceptable level and had been confirmed. The DMFT checklist was completed by a dentist. Data were collected and fed into the SPSS program, version 20. They were analyzed using the following descriptive and analytical statistical tests: Pearson’s correlation coefficient, Spearman’s correlation coefficient, and independent t-test. The significance level was set at α<0.05.
Results
Results showed that the mean age of the pregnant women in the study was 23.1 ± 3.9 years and their mean GA was 9.7 ± 2.9 weeks. The mean of their DMFT was 7.46 ± 4.59. The means of decayed, missing, and filled teeth were 4.98 ± 3.38, 1.44 ± 2.39, and 1.07 ± 2.05, respectively. Their mean scores of knowledge, perceived susceptibility, and perceived selfefficacy were 7.08 ± 1.60, 23.50 ± 3.4, and 27.56 ± 4.43, respectively (Table 1).
| Variables | No. | Min | Max | Mean | SD |
|---|---|---|---|---|---|
| Knowledge | 300 | 3 | 15 | 7.08 | 1.6 |
| Perceived susceptibility | 300 | 2 | 32 | 23.5 | 3.99 |
| Perceived self-efficacy | 300 | 2 | 36 | 27.56 | 4.43 |
| Age | 300 | 16 | 37 | 23.07 | 3.93 |
| gestational age | 300 | 5 | 14 | 9.73 | 2.96 |
| DMFT* | 300 | 0 | 23 | 4.76 | 4.59 |
| Decayed teeth | 300 | 0 | 16 | 4.94 | 3.38 |
| Missing teeth | 300 | 0 | 20 | 1.44 | 2.39 |
| Filled teeth | 300 | 0 | 16 | 1.07 | 2.05 |
| *Decayed, missing, and filled teeth | |||||
Table 1. The mean scores of the pregnant women’s knowledge, perceived susceptibility, perceived self-efficacy, age, gestational age, DMFT, and the DMFT components.
The highest and lowest frequency of education among the pregnant women in the study was for high-school education (43.7%) and elementary education (8.7%), respectively. Moreover, 94.7% of them were housewives and 5.3% were employed. The highest frequency of average economic condition among them was 54.3% and the lowest frequency of excellent economic condition was 1%. Furthermore, 58.7% of the pregnant women had medical insurance but 41.3% of them had no medical insurance (Table 2).
| Variables | No. | % | |
|---|---|---|---|
| Educational status | Primary school | 26 | 8.7 |
| Junior high school | 46 | 15.3 | |
| High school | 131 | 43.7 | |
| University | 97 | 32.3 | |
| Economic status | Low | 54 | 18 |
| Average | 163 | 54.3 | |
| Good | 80 | 26.7 | |
| Excellent | 3 | 1 | |
| Medical insurance | Yes | 176 | 58.7 |
| No | 124 | 41.3 | |
| Occupational status | Housewives | 284 | 94.7 |
| Employed | 16 | 5.3 | |
| Total | 300 | 100 | |
Table 2. The frequency distribution of demographic (socio-economic) variables for the pregnant women in the study.
According to Pearson’s correlation coefficient, there was a significant and inverse relationship between the mean score of knowledge and the mean of DMFT (p<0.001, r=-0.205), the mean score of perceived susceptibility and the mean of DMFT (p= 0.002, r=-0.174), and the mean score of perceived selfefficacy and the mean of DMFT (p<0.001, r=-0.270) (Table 3). Pearson’s correlation coefficient revealed that there was a significant and positive correlation between the pregnant mothers’ age and DMFT (p=0.001, r=0.188). However, there was no significant relationship between the mothers’ age and decayed teeth (p=0.79, r=-0.015) but their age had a significant and positive correlation with missing teeth (p<0.001, r=0.278) and with filled teeth (p=0.03, r=0.119). Pearson’s correlation coefficient also showed that there was a significant and positive correlation between GA and the mean of DMFT (p=0.001, r=0.198) and between GA and decayed teeth (p<0.001, r=0.213). Nevertheless, there was no significant relationship between GA and missing teeth (p=0.70, r=0.022) and between GA and filled teeth (p=0.25, r=0.067) (Table 4).
| Variables | Knowledge | Perceived susceptibility | Perceived self-efficacy | DMFT |
|---|---|---|---|---|
| Knowledge | 1 | |||
| Perceived susceptibility | p=0.001 | 1 | ||
| r=0.189 | ||||
| Perceived self-efficacy | p=0.080 | p<0.001 | 1 | |
| r=0.165 | r=0.424 | |||
| DMFT | p<0.001 | p=0.002 | p<0.001 | 1 |
| r=-0.205 | r=-0.174 | r=-0.270 |
Table 3. Pearson’s correlation between the HBM constructs and DMFT.
| Variables | Age | GA | DMFT |
|---|---|---|---|
| Age | 1 | ||
| GA | p=0.91 | 1 | |
| r=0.006 | |||
| DMFT | p=0.001 | p=0.001 | 1 |
| r=0.188 | r=0.198 | ||
| Decayed teeth | p=0.79 | p<0.001 | p<0.001 |
| r=-0.015 | r=0.213 | r=0.741 | |
| Missing teeth | p<0.001 | p=0.70 | p<0.001 |
| r= 0.278 | r=0.022 | r=0.527 | |
| Filled teeth | p=0.03 | p=0.25 | p<0.001 |
| r=0.119 | r=0.067 | r=0.401 |
Table 4. Pearson’s correlation between the pregnant mothers’ age, GA, DMFT, and the DMFT components.
According to Spearman’s correlation coefficient, there was no significant association between the mean of DMFT and the pregnant women’s education (p=0.62, r=0.029) or between decayed teeth and their education (p=0.67, r=-0.024); however, there was a significant and inverse association between their education and missing teeth (p=0.04, r=-0.117). Moreover, there was a significant and positive correlation between their education and filled teeth (p=0.001, r=0.184). Spearman’s correlation coefficient showed that there was a significant and inverse relationship between the mean of DMFT and the pregnant women’s economic condition (p=0.002, r=-0.182), between decayed teeth and their economic condition (p=0.002, r=-0.179), and between missing teeth and their economic condition (p<0.001, r=-0.213). Nonetheless, no significant association was found between the pregnant women’s economic condition and filled teeth (p=0.32, r=0.057) (Table 5).
| Variables | Educational status | Economic status |
|---|---|---|
| DMFT | p=0.62 | p=0.002 |
| r=0.029 | r=-0.182 | |
| Decayed teeth | p=0.67 | p=0.002 |
| r=-0.024 | r=-0.179 | |
| Missing teeth | p=0.04 | p<0.001 |
| r=-0.117 | r=-0.213 | |
| Filled teeth | p=0.001 | p=0.39 |
| r=0.184 | r=0.057 |
Table 5. Spearman’s correlation between the pregnant mothers’ educational status, economic status, DMFT, and the DMFT components.
The independent t-test demonstrated that there was no significant difference between the pregnant women with medical insurance and those lacking medical insurance with respect to the mean of DMFT (p=0.96); moreover, there was a significant difference between the employed women and the housewives with respect to the mean of DMFT (p=0.03) so that the mean of DMFT was higher among the employed pregnant women (Table 6).
| Variables | DMFT | Independent t-test P-value | |
|---|---|---|---|
| Medical insurance | Yes | 7.45 ± 4.3 | 0.96 |
| No | 7.47 ± 4.9 | ||
| Occupational status | Housewives | 7.3 ± 4.6 | 0.03 |
| Employed | 9 ± 2.6 | ||
Table 6. The mean of DMFT based on the pregnant women’s medical insurance and occupational status.
Discussion
The results of the present research showed that the mean scores of knowledge and DMFT had a significant relationship with each other. Among the pregnant women whose mean score of knowledge was higher, the mean score of DMFT was lower. These results were in line with those of a study by Ogawa et al. but were inconsistent with results of a study by Bahri et al. [31,32]. Various studies have indicated that pregnant women have a limited knowledge of oral and dental health so that, in a study by Keirse et al., only 35% of pregnant women cared about oral and dental health during pregnancy [9]. In research by Habashneh et al., 60% of pregnant women were unaware that they should have been visited by a dentist during pregnancy and 68% preferred to be visited after pregnancy [33]. Results of a study by Kandan et al. revealed that 45% of women had the idea that no dental procedure should be carried out during pregnancy [34]. These statistics necessitate enhancing pregnant women’s and pregnancy health personnel’s knowledge [35]. Results of this study demonstrated that the mean scores of perceived susceptibility and self-efficacy had a significant relationship with DMFT so that the pregnant women whose mean scores of perceived susceptibility and selfefficacy were higher had a lower mean of DMFT.
It is also in line with results of a study by Shahnazi et al., who said it would be possible to prevent the increase in pregnant women’s DMFT by increasing perceived susceptibility and self-efficacy [23,25]. It is important for a pregnant mother to know to what extent she is at risk of dental caries. In addition, considering the role of self-efficacy, individuals will be stimulated to perform health behaviors and they will also perform these behaviors to confront challenges when they feel they are in control of health behaviors. Among effective factors in this field are proper brushing and flossing, the capability to overcome drowsiness and lethargy, and the ability to go on a low-sugar diet. Effects of perceived susceptibility and selfefficacy on oral and dental health care behaviors have been confirmed [15,23,24]. In the present research, the mean of DMFT in the pregnant women from Delfan was 7.46 ± 4.59, which was higher than that in pregnant women from Arak in Iran (5.4 ± 2.83), Ahvaz in Iran (6.23 ± 3.01), India (4.44 ± 3.68), and Finland (2.9 ± 3.22) [16,17,36,37].
However, the mean of DMFT was lower than that in pregnant women from Isfahan in Iran (10.6 ± 4.21) and Italy (7.9 ± 4.2) [15,18]. The above-mentioned studies show that pregnant women’s mean DMFT is high so that a study in India revealed that the mean of DMFT was 3.42 ± 2.23 in pregnant women but it was 1.96 ± 1.24 in non-pregnant women [36]. The difference in DMFT in different cities of Iran and also other parts of the world reflect effects of different geographical regions, different cultures, different personal and eating habits, and poor oral and dental health care [38,39]. The reasons for a high prevalence of dental caries in Iran, as compared with other countries such India and Finland, might be a high-sugar diet, a high intake of sugar and sweet food (so that the consumption of sweet food in the Iranian community rose from 25.1 kg in 1991 to 31 kg in 2006 [an increase of 22%]), and their poor oral and dental health behaviors [15]. In the present research, the mean of decayed teeth in the pregnant women (4.94 ± 3.38) was higher than the means of missing teeth (1.44 ± 2.39) and filled teeth (1.07 ± 2.05). This finding is in line with results of studies by Pentapati et al. and Marinho et al., which could have been due to pregnancy conditions and hormonal changes or poor oral and dental health in these women [36,40]. The current research indicated a significant relationship between the pregnant mothers’ age and the mean of DMFT so that the mean of DMFT increased with an increase in their age. This finding was consistent with results of studies by Shamsi et al. [17], Allameh et al. [18], Kumar et al. [41], Tonello et al. [42], and Karunachandra et al. [43], but was inconsistent with results of a study by Vergnes et al. [44]. In the present research, there was a significant relationship between the mothers’ age and missing and filled teeth, but not decayed ones. In the study by Shamsi et al., filled and decayed teeth were significantly related to mothers’ age [20]. The study by Karunachandra et al. showed that there was a significant relationship between mothers’ age and decayed teeth [43].
The difference in the DMFT components (that is, decayed, missing, and filled teeth) in various studies could have resulted from cultural, geographical, educational, and economic differences between the study groups. The present research revealed that there was a significant association between GA and the mean of DMFT so that the mean of DMFT rose as GA increased. This result is in line with results of the studies by Kumar et al. [41] and Kandan et al. [34] but was inconsistent with results of the study by Allameh et al. [18]. In the current study, there was a significant relationship between GA and decayed teeth, which is consistent with results of the study by Kumar et al. [41] but is inconsistent with results of the study by Allameh et al. [18]. In the present study, the rate of decayed teeth went up as GA increased, which could have resulted from pregnant women’s high intake of sugar and sweet food, the increased frequency of consuming calories, and their disregard for oral and dental health care due to hormonal and nutritional changes [14,16,38,41]. The present research demonstrated that there was no significant relationship between the pregnant women’s educational status and the mean of DMFT, which is inconsistent with results of studies by Gharizadeh et al. [16], Shamsi et al. [17], and Vano et al. [45]. The reason for this difference might have been the difference in the frequency of education in the conducted studies and also economic, geographical, and cultural diversities of the study populations. The current study showed a significant association between the mothers’ educational status and missing and filled teeth, but not decayed teeth. In studies by Vano et al. [45] and Senna et al. [46], a significant relationship, too, was observed between the pregnant mothers’ educational status and filled and missing teeth so that the rate of missing teeth was lower and the rate of filled teeth was higher among those who were more educated.
Results of the current study showed a significant relationship between the economic status and the mean of DMFT in the pregnant women so that the mean of DMFT was higher when the economic status was lower. These results are in line with results of the studies by Shamsi et al. [17] and Rawtiya et al. [47] but they were inconsistent with results of the study by Marinho et al. [40]. In the present study, there was a significant association between the economic status and decayed teeth so that the rate of decayed teeth was lower when the economic status was higher, which is in line with results of studies by Shamsi et al. [20] and Rawtiya et al. [47]. In the current study, there was a significant association between the economic status and missing teeth so that the rate of missing teeth was higher as the economic status was lower, which is in line with the study by Rawtiya et al. [47]. The present study revealed no significant relationship between the economic status and filled teeth, which is inconsistent with results of the study by Rawtiya et al. [47]. Considering the WHO’s 2020 goal for reducing the rate of missing teeth at age 18 and in the 35-44 age range due to dental caries, it is necessary to have oral and dental health education for the community, especially those in low socio-economic status in order to prevent the increase in dental caries and tooth extraction [48]. The results of the current study revealed no significant difference between the mean of DMFT and medical insurance coverage, which is in line with findings of the study by Shamsi et al. [17]. The reasons for this difference could be the fact that, in Iran, the cost of dental care services is high, dental insurance covers only visit and consulting, and dental costs are not in proportion to people’s income level. The present research demonstrated a significant difference between the mean of DMFT and the pregnant women’s employment status so that the mean of DMFT in them was higher, which is consistent with the results of a study by Massamba et al. [49]. The reasons why the mean of DMFT in the employed pregnant women was high could have been eating sugary and sweet snacks at work, being under occupational stress (along with general pregnancy conditions), and failing to devote enough time to oral and dental health.
Conclusion
Given the vulnerability of pregnant women, the increase in the mean of DMFT during pregnancy (as compared with the normal community), effects of oral and dental health on pregnancy, and results of the relationship between DMFT and the two constructs (namely, perceived susceptibility and perceived self-efficacy) in the pregnant women from Delfan, it should be mentioned that, in order to improve pregnant women’s knowledge, perceived susceptibility, and perceived self-efficacy, it is necessary to develop health education programs based on the HBM constructs, particularly among pregnant mothers in low socio-economic status. It is also necessary to conduct oral and dental health care programs for pregnancy health personnel.
References
- Hunter LP, Yount SM. Oral health and oral health care practicesamong low-income pregnant women. J Midwifery Womens Health 2011; 56: 103-109.
- Slade GD, Spencer AJ. Development and evaluation of the Oral Health Impact Profile. Community Dent Health 1994; 11: 3-11.
- Petersen PE. The World Oral Health Report 2003: continuous improvement of oral health in the 21st century-the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol 2003; 31: 3-23.
- Moses J, Rangeeth BN. Prevalence Of Dental Caries, Socio-Economic Old School Going Children Of Chidambaram Status And Treatment Needs Among 5 To15 Year Old School Going Children Of Chidambaram. J Clinic Diag Res 2011; 1: 146-151.
- Gaffield ML, Gilbert BJ, Malvitz DM, Romaguera R. Oral health during regnancy: an analysis of information collected by the pregnancy risk assessment monitoring system. J Am Dent Assoc 2001; 132: 1009-1016.
- Honkala S, Al-ansari J. Self-reported oral health, oral hygiene habits and dental attendance of pregnant women in Kuwait. J Clinic Periodont 2005; 32: 809-814.
- Achtari MD, Georgakopoulou EA, Afentoulide N. Dental care throughout pregnancy: what a dentist must know. Oral Health Dent Manag 2012; 11: 169-176.
- Varenne B, Petersen PE, Ouattara S. Oral health behaviour of children and adults in urban and rural areas of Burkina Faso, Africa. Int Dent J 2006; 56: 61-70.
- Keirse MJ, Plutzer K. Women's attitudes to and perceptions of oral health and dental care during pregnancy. J Perinat Med 2010; 38: 3-8.
- Offenbacher S, Lieff S, Boggess KA, Murtha AP, Madianos PN, Champagne CM, McKaig RG, Jared HL, Mauriello SM, Auten RL Jr, Herbert WN, Beck JD. Maternal periodontitis and prematurity. Part I: Obstetric outcome of prematurity and growth restriction. Ann Periodontol 2001; 6: 164-174.
- Moore S, Ide M, Coward PY, Randhawa M, Borkowska E, Baylis R, Wilson RF. A prospective study to investigate the relationship between periodontal disease and adverse pregnancy outcome. Br Dent J 2004; 197: 251-258.
- Mangskau KA, Arrindell B. Pregnancy and oral health: utilization of the oral health care system by pregnant women in North Dakota. Northwest Dent 1996; 75: 23-28.
- Lydon-Rochelle MT, Krakowiak P, Hujoel PP, Peters RM. Dental care use and self-reported dental problems in relation to pregnancy. Am J Public Health 2004; 94: 765-771.
- Rovida TA, Moimaz SA, Limba DP, Garbin CA. Self-perepception and Oral Health in Pregnant Adolescents. OHDM 2014; 13: 842-846.
- Villa A, Abati S, Pileri P, Calabrese S, Capobianco G, Strohmenger L, Ottolenghi L, Cetin I, Campus GG. Oral health and oral diseases in pregnancy: a multicentre survey of Italian postpartum women. Aust Dent J 2013; 58: 224-229.
- Gharizadeh N, Haghiighizadeh MH, Sabarhaji W, Karimi A. A study of DMFT and oral hygiene and gingival status among pregnant women attending Ahwaz health centers. Sci Med J Ahvaz Jundishapur Univ MedSci 2005; 43: 40-47.
- Shamsi M, HidarniaA, NiknamiS. A survey of oral health care behaviorin pregnant women of Arak: Application of health belief model. J Mazandaran Univ Med Sci 2012; 22: 104-115.
- Allameh M, Khademi H, Eslami M. A cross-sectional survey on the relationship between some biologic maternal characteristics and dental status of pregnant women in Isfahan, Iran, in 2012. J Oral Health Oral Epidemiol 2014; 3: 72-78.
- Thomas NJ, Middleton PF, Crowther CA. Oral and dental health care practices in pregnant women in Australia: a postnatal survey. BMC Pregnancy Childbirth 2008; 8: 13.
- Shamsi M, Hidarnia A and Niknami SH. Self-Reported Oral Hygiene Habits and Self-Care in the Oral Health in Sample of Iranian Women During Pregnancy World. Appl Sci J 2013; 22: 647-656.
- Butler J. In: 1 ed. Principal of health education and health promotion, editor. USA: WadsWorth. 2001.
- Glanz K, Rimer BK, Viswanath K. Health behavior and health education. 4 ed. New York: John Wiley & Sons. 2008.
- Ramezankhani A, Mazaheri M, Dehdari T, et al. Relationshipbetween health belief model constructs and DMFT among five-grade boy students in the primary school in Dezfool. Sci Med J 2011; 10: 221-228.
- Buglar ME, White KM, Robinson NG. The role of self-efficacy in dental patients' brushing and flossing: testing an extended Health Belief Model. Patient Educ Couns 2010; 78: 269-272.
- Shahnazi H, Hosseintalaei M, Esteki Ghashghaei F, Charkazi A, Yahyavi Y, Sharifirad G. Effect of Educational Intervention on Perceived Susceptibility Self-Efficacy and DMFT of Pregnant Women. Iran Red Crescent Med J 2016; 18: 24960.
- Boggess KA, Urlaub DM, Massey KE. Oral hygiene practices and dental service utilization among pregnant women. J Am Dent Assoc 2010; 141: 553-561.
- Berkowitz RJ. Acquisition and transmission of mutans streptococci. J Calif Dent Assoc 2003; 31: 135-138.
- Meyer K, Geurtsen W, Günay H. An early oral health care program starting during pregnancy: results of a prospective clinical long-term study. Clin Oral Investig 2010; 14: 257-264.
- World Health Organization. Oral Health Surveys: Basic Methods. 4th ed. Geneva, Switzerland: World Health Organization. 1997.
- Ogawa H, Soe P, Myint B, Sein K, Kyaing MM, Maw KK, Oo HM, Murai M, Miyazaki H. A pilot study of dental caries status in relation to knowledge, attitudes and practices in oral health in Myanmar. Asia Pac J Public Health 2003; 15: 111-117.
- Bahri N, Eliati HR, Salarvand SH. Assessment of DMFT Index in Pregnant Women and its Relationship with knowledge and Attitude and Health Behaviors in Terms of Oral and Dental Cares (Mashhad-2009). Iran J Obestet Gynecol Infertil 2012; 15: 13-20.
- Al Habashneh R, Guthmiller JM, Levy S. Factors related to utilization of dental services during pregnancy. J Clin Periodontol 2005; 32: 815-821.
- Kandan PM, Menaga V, Kumar RR. Oral health in pregnancy (guidelinesto gynecologists, general physicians & oral health careproviders). J Pak Med Assoc 2011; 61: 1009-1014.
- Hashim R. Self-reported oral health, oral hygiene habits and dental service utilization among pregnant women in United Arab Emirates. Int J Dent Hyg 2012; 10: 142-146.
- Pentapati K, Acharya SH, Bhat M. Oral Health among Women-A Cross-sectional Study from South India. Int J Dental Sci Res 2015; 3: 17-19.
- Meurman JH, Furuholm J, Kaaja R. Oral health in women with pregnancy and delivery complications. Clin Oral Investig 2006; 10: 96-101.
- Kannan N, Srivalli L, Patil R. Maternal Oral Health Status & Salivary Fanction in Nellore Population: An Observational Study. Int JMCH 2015; 3: 15-23.
- Vellappally S, Fiala Z, Smejkalová J. Influence of tobacco use in dental caries development. Cent Eur J Public Health 2007; 15: 116-121.
- Marinho A, Dutra F, Lucas S, Abreu M. Conditions and Perceptions of Oral Health in Brazilian Pregnant Women. Brazil Res Pediat Dent Integrat Clinic 2016; 16: 257-268.
- Kumar S, Tadakamadla J, Tibdewal H. Factors influencing caries status and treatment needs among pregnant women attending a maternity hospital in Udaipur city, India. J Clin Exp Dent 2013; 5: 72-76.
- Tonello AS, Zuchieri MAVO, PardiV. Acssessment of Oral Health Status of Pregnant Women Participating in a Familly Health Program in the City of Lucas do Rio Verde-MT-Brazil. Brazil J Oral Sci 2007; 6: 1265-1268.
- Karunachandra NN, Perera IR, Fernando G. Oral health status during pregnancy: rural-urban comparisons of oral disease burden among antenatal women in Sri Lanka. Rural Remote Health 2012; 12: 1902.
- Vergnes JN, Kaminski M, Lelong N. Frequency and risk indicators of tooth decay among pregnant women in France: a cross-sectional analysis. PLoS One 2012; 7: 33296.
- Vano M, Gennai S, Karapetsa D. The influence of educational level and oral hygiene behaviours on DMFT index and CPITN index in an adult Italian population :an epidemiological study. Int J Dent Hygiene 2015; 13: 151-157.
- Senna A, Campus G, Gagliani M. Socio-economic influence on caries experience and CPITL values among a group of Italian call-up soldiers and cadets. Oral Health Prev Dent 2005; 3: 39-46.
- Rawtiya M, Munuga S, Verma K, Khan S, Loomba K. Oral Health and Social Inequality: Prevalence of Dental Caries in relation to Age, Gender and Socioeconomic Status-WHO Goal 2020. IJRD 2014; 3: 12-18.
- Hobdell M, Petersen PE, Clarkson J, Johnson N. Global goals for oral health 2020. Int Dent J 2003; 53: 285-288.
- Massamba D, Gilles B, Daouda C, Mbacké LCM, Aida K, Mbatio D, Ibrahima B, Daouda F. Severity and Magnitude of Caries among Rural Populations in Ferlo in Senegal. O Jepi 2016; 6: 610-615.