Research Article - Biomedical Research (2017) Volume 28, Issue 17
The ratio of neutrophil lymphocytes and CRP comparison in young obese individuals
Asl?han Dilara Demir1*, Zeynep Hülya Durmaz2, Tuba Ozkan3,Orhan Demir4, R?dvan Güçkan5 and Çetin K?l?nç5
1Department of Internal Medicine, Amasya University Research Hospital, Amasya, Turkey
2Department of Biochemistry, Amasya University Research Hospital, Amasya, Turkey
3Department of Dietetics, Amasya University Research Hospital, Amasya, Turkey
4Department of Cardiology, Amasya University Research Hospital, Amasya, Turkey
5Department of Microbiology, Amasya University Research Hospital, Amasya, Turkey
- *Corresponding Author:
- Aslihan Dilara Demir
Department of Internal Medicine
Amasya University Research Hospital
Amasya, Turkey
Accepted date: August 03, 2017
Abstract
Objective: Obesity is a growing problem of public health in developed and developing countries, and its prevalence is increasing in Turkey. Neutrophils play an important role in inflammation. C-Reactive Protein (CRP) is an important mediator in inflammation. In our study, we aimed to compare the changes in CRP levels and Neutrophil Lymphocyte Ratio (NLR) in obese individuals.
Methods: Totally 298 individuals (251 female and 47 male) were included in the study. Patients were divided into three groups according to Body Mass Index (BMI) values. Serum neutrophil and lymphocyte levels and CRP levels were measured.
Results: There is a positive correlation between Body Mass Index (BMI) and CRP. There is also a positive correlation between BMI and n/l. However, even it is too low, it can be considered as insignificant. The 4.5% of the high CRP level is attributed to an increase in BMI. Only 0.1% of the very low increase in neutrophil lymphocyte rate is attributed to an increase in the BMI.
Conclusion: There is no statistical significance between neutrophil lymphocyte levels and BMI groups. In our study, the use of CRP as an indicator of inflammation in obese younger individuals is more useful than n/l ratio.
Keywords
Obesity, C-reactive protein (CRP), Neutrophil lymphocyte ratio (NLR)
Introduction
Obesity is a growing public health problem in developed and developing countries [1]. In Turkey, the prevalence of obesity in adults has increased from 18.8% to 36% over two decades [2]. While the prevalence of overweight is higher in men, the prevalence of obesity is higher in women [3].
The 10-15% of body weight in males and 15-20% in females constitute fat tissue. Fat tissue has functions such as storage of fat soluble vitamins, physical protection, energy storage, and thermogenesis. Obesity is the result of the excessive increase of the fat tissue [4]. Adipose tissue is a fat support and an endocrine organ. In addition, it is effective in the metabolism and energy balance of the macronutrients [5].
Obesity is a multifactorial disease resulting from genotype and environmental interaction [6]. It is associated with many diseases such as diabetes, hypertension, dyslipidemia, atherosclerosis, and malignant diseases [1]. Obesity causes subclinical inflammation [7]. Although inflammatory processes at the onset of obesity are not very clearly defined, it has been known that leukocytes play a very important role in inflammation [8].
Lately, there has been a lot of evidence supporting the association between obesity and inflammation. Studies have focused on adipokines, macrophages, adiponectin, and immunocytes in fat tissue [9]. The increase in bioactive peptides produced in obesity affects the development of hypertension (angiotensinogen), impaired fibrinolysis (plasminogen activator inhibitor-1), and insulin resistance (acylation-stimulating protein, tumor necrosis factor, Interleukin-6, resistin) [10].
CRP is an important marker of inflammation. In recent years, CRP has begun to be used as an inflammation marker in the neutrophil lymphocyte ratio [11].
Neutrophils are the most important mediators of natural immunity. In the initial defense against pathogens, neutrophils are effective in the acute inflammatory response. Neutrophil lymphocyte ratio is a simple, inexpensive, and effective marker of inflammation. It is associated with many inflammatory and malignant diseases.
CRP is the most important acute phase protein. CRP is a protein released from secondary hepatocytes in response to interleukin 6, interleukin 1α, and tumor necrosis factor β induction [12]. CRP is an important effector in an immune response in obesity [13].
It has been shown in a large number of studies that there is a relationship between obesity and CRP levels [14]. Leukocyte count and high-sensitivity C-reactive protein (hs-CRP) indicate inflammation [15]. CRP increases in many inflammatory, infectious, and malignant diseases [16].
Materials and Methods
In this study, Amasya University Sabuncuo?lu ?erefeddin Training and Research Hospital patient database was used. The study was conducted between January 1, 2016 and 31 December 2016 with patients who applied to the internal diseases outpatient clinic. In this study, we aimed to compare the neutrophil lymphocyte ratio and C-reactive protein levels in young obese subjects. The liver enzymes and blood creatinine levels of the patients were normal. HGB, HCT, MCV, MCH, MCHC were also in the normal range. Patients with anemia, heart failure, renal insufficiency, hypothyroidism, and hyperthyroidism were excluded from the study. Totally 298 patients were included in the study. The body mass index values were calculated by dividing the height values to the square of the body weight values. Patients were divided into groups according to their body mass index values. Neutrophil lymphocyte ratio and C-reactive protein levels were compared between the groups. Of all patients, 23 (16.5%) and 116 (83.5%) of them who had BMI values less than 30 were respectively males and females. Furthermore, 24 (17.4%) and 114 (82.6%) of them who had BMI values between 30 and 39.9 were respectively males and females. Finally, 21 (100%) of them who had BMI values 40 or more were females.
Blood neutrophil measurements (normal values: 50.0-70.0%) and blood lymphocyte measurements (normal values: 20-40%) were measured on a MindRay 6800 hemogram instrument. CRP (normal values: 0.00-5.0 mg/l) were studied by SIEMENS BN II instrument by using the nephelometric method. The CV value of the method was 2.6.
Findings
GraphPad Prism version 6.00 (GraphPad Software, La Jolla California USA) was used for statistical analysis. One-way ANOVA was used to compare quantitative data. Multiple logistic regression analyzes were performed in order to investigate how dependent variables were affected by independent variables. The Chi-Square test was used to understand gender differences. The results were evaluated in the 95% confidence interval and p<0.01 was accepted as statistically significant. Correlation between the parameters was done by Pearson correlation analysis. Correlation coefficient (r) was evaluated as weak when it was between 0.00-0.24, moderate when it was between 0.25-0.49, strong when it was between 0.50-0.74, and very strong when it was between 0.75-1.00.
Totally 298 patients were evaluated. According to body mass indexes of participants, 139 of them (46.6%) had BMI values less than 30, 138 of them (46.3%) had BMI values between 30 and 39.9, and 21 of them (7%) had BMI values 40 and over. Of all patients, 23 male patients (16.5%) and 116 female patients (83.5%) had BMI values less than 30. Twenty-four of the male patients (17.4%) and 114 of the female patients (82.6%) had BMI values between 30 and 39.9. Twenty-one of the female patients (100%) had BMI values 40 or more. Table 1 shows the gender differences according to the body mass index values of patients. No statistically significant difference was observed between groups in terms of gender.
| BMI <30 (n=139) | BMI 30-39.9 (n=138) | BMI ≥ 40 (n=21) | χ2 | p | ||||
|---|---|---|---|---|---|---|---|---|
| Gender | n | % | n | % | n | % | ||
| Female | 116 | 83.5 | 114 | 82.6 | 21 | 100 | 4.268 | 0.1184 |
| Male | 23 | 16.5 | 24 | 17.4 | 0 | 0 | 2 | |
Table 1. Gender differences according to the body mass index values.
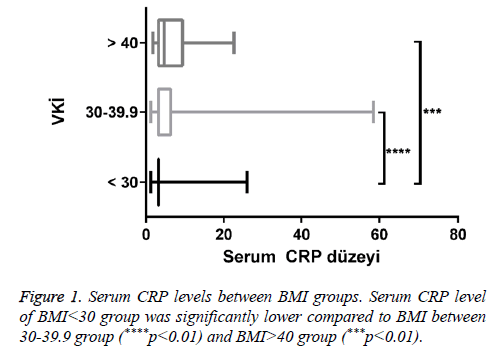
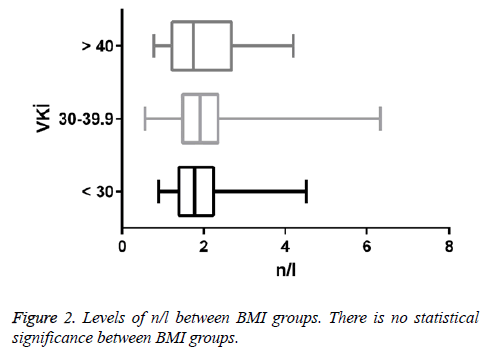
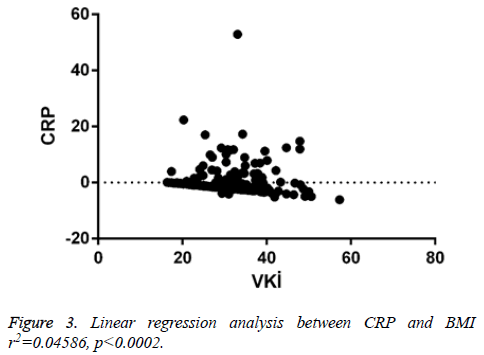
There was a positive correlation between BMI and CRP (r=0.214, p<0.0002). The difference was less and it can be considered insignificant. There was a positive correlation between BMI and n/l (r=0.03886, p<0.504). There was a positive correlation between CRP and n/l (r=0.199, p<0.00056). When linear regression analysis was performed, 4.5% of the CRP increase was attributed to the increase in body mass index (r2=0.04586) (Figures 1-3 and Table 2).
| Parameters | BMI | CRP | n/l | |
|---|---|---|---|---|
| BMI | r | 1 | ||
| p | ||||
| CRP | r | 0.214* | 1 | |
| p | 0.0002 | |||
| n/l | r | 0.03886* | 0.199* | 1 |
| p | 0.504 | 0.00056 |
Table 2. Analysis of correlation between parameters.
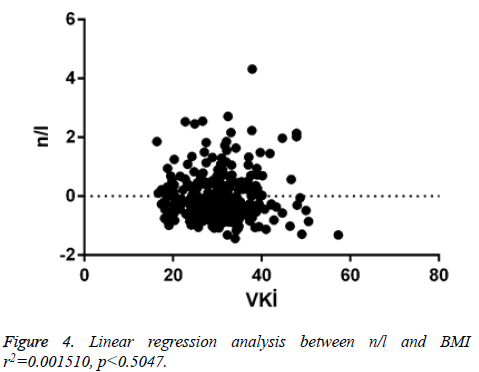
When linear regression analysis was performed, 0.1% of the very low increase in n/l was attributed to the increase in body mass index (r2 =0.001510) (Figure 4).
Discussion
Trellakis et al. investigated the role of neutrophils in obese patients and the regulation of neutrophils by adiponectin. Elevated levels of neutrophil lymphocytes, high-sensitivity Creactive protein, chemokines (such as CXCL8, CCL3, CCL5), apoptosis markers (such as M30 and M65), and some neutrophil products have been shown to be an indicator of inflammation in overweight and obese individuals [9].
In a study conducted by Nijhuis et al. neutrophil activation markers such as calprotectin were studied in 37 severe obese and 9 normal overweight patients. The levels of these markers were significantly higher in obese group compared to the healthy group [17].
Visser et al. found an association between increased BMI and increased CRP levels in 17-39 y old overweight and obese patients. Low-grade inflammation was observed in overweight and obese subjects [18].
Atmaca et al. investigated the relationship between neutrophil lymphocyte ratio and obesity in 116 patients. It was found that elevated neutrophil levels were observed with increased inflammation. It was determined that the increased percentage of neutrophil lymphocytes was correlated with the BMI ratio. It was observed that the ratio of neutrophil lymphocytes can be used as an inflammatory marker in obese patients [11].
Kim et al. studied with 104 Korean patients who were between the ages of 34 and 60. It was shown that higher CRP levels have been shown to be associated with central obesity even in low-risk individuals [19].
Furuncuo?lu et al. performed a study and investigated the effect of obesity on n/l and platelet/lymphocyte ratio in 223 patients who were between the ages of 18 and 65. It was observed that WBC, neutrophil, lymphocyte, and platelet counts were easily affected by BMI [20].
Bahad?r et al. conducted a study with 1267 patients with obesity and metabolic syndrome. It was shown that there was a significant increase in CRP level with BMI and there was no increase n/l ratio [15].
According to the results of the 9 y study, Laurson et al. found that there was an increase in CRP levels and white blood cells in subgroups [21].
Lao et al. found a strong association between the number of neutrophil lymphocytes and the metabolic syndrome in a study involving 3020 men and 7256 women.
In this study, we aimed to compare the neutrophil lymphocyte ratio and C-reactive protein levels in young obese individuals. There is no statistical correlation between neutrophil lymphocyte ratio and BMI groups. However, even it is too low, there is a positive correlation between BMI and n/l. The reason of this is that leukocytes may also play an important role in the inflammatory response. CRP levels were significantly higher in the BMI<30 groups compared to BMI between 30-39.9 and 40 BMI>40 groups. In our study, we found a positive correlation between BMI and CRP. Obesity is an inflammatory process and this suggests that CRP, one of the important markers of inflammation, may increase. When linear regression analysis was performed, 4.5% of the high CRP level was attributed to an increase in BMI. Furthermore, 0.1% of the very low increase in neutrophil lymphocyte rate was attributed to an increase in the BMI. CRP and n/l ratio can be used as markers in obese individuals. It was found that the increase in n/l was lower than that of CRP. In our study, the use of CRP as an indicator of inflammation in obese younger individuals was more useful than n/l ratio.
There were limitations in our study. For instance; there were a limited number of patients. We also did not have information about patient’s diets, smoking habits, daily activities, and their effort statuses. Factors such as gender and age may affect the subclinical inflammation and gender distribution was not the same in all groups. In addition, there was no male patient in the BMI>40 group. These can be considered as the weak points of the study.
References
- Argolo DF, Lyengar NM, Hudis CA. Obesity and cancer: concepts and challenges. Indian J Surg Oncol 2015; 6: 390-398.
- C Erem. Prevalence of overweight and obesity in Turkey. IJC Metabolic Endocrine 2015; 8: 38-41.
- Yumuk VD. Prevalence of obesity in Turkey: International association for the study of obesity. Obesity Rev 2005; 6: 9-10
- Keskin S, Sayal? E, Temeloglu E, Ekizoglu ?. Obezite Ve Inflamasyon. Turkiye Klinikleri J MedSci 2005; 25: 636-641.
- Maghsoudi Z, Kelishadi R,Hosseinzadeh-Attar MJ. Association of Chemerin levels with anthropometric indexes and C-reactive protein in obese and non-obese adolescents. ARYA Atheroscler 2015; 11: 102-108.
- Bahad?r A, Baltac? D, Türker Y, Türker Y, Iliev D, Öztürk S. Is the neutrophil-to-lymphocyte ratio indicative of inflammatory state in patients with obesity and metabolic syndrome? Anatol J Cardiol 2015; 15: 816-22.
- Vargas R, Ryder E, Diez-Ewald M, Mosquera J, Durán A, Valero N. Increased C-reactive protein and decreased Interleukin-2 content in serum from obese individuals with or without insulin resistance: Associations with leukocyte count and insulin and adiponectin content. Diabetes Metab Syndr 2015; 1871-4021.
- Trellakis S, Rydleuskaya A, Fischer C, Canbay A, Tagay S, Scherag A. Low adiponectin, high levels of apoptosis and increased peripheral blood neutrophil activity in healthy obese subjects. Obes Facts 2012; 5: 305-318.
- Emral R. Adiponectin and other cytokines .Turkiye Klinikleri J MedSci 2006; 26: 409-420.
- Atmaca HU, Akbas F, Okten IN, Nuhoglu E, BelcikInal B. Nötrofil Lenfosit Oran? Obezitede ?nflamatuar Bir Belirteç Olarak Kullan?labilir mi? ?stanbul Med J 75046.
- Gao SQ, Huang LD, Dai RJ, Chen DD, Hu WJ, Shan YF. Neutrophil-lymphocyte ratio: a controversial marker in predicting Crohn’s diseases verity. Int J ClinExpPathol 2015; 8: 14779-14785.
- Vargas R, Ryder E, Diez-Ewald M, Mosquera J, Durán A, Valero N. Increased C-reactive protein and decreased Interleukin-2 content in serum from obese individuals with or without insulin resistance: Associations with leukocyte count and insulin and adiponectin content. Diabetes Metab Syndr 2015; 15: 1871-4021.
- Brooks GC, Blaha MJ, Blumenthal RS. Relation of C-reactive protein to abdominal adiposity. Am J Cardiol 2010; 106: 56-61.
- Bahad?r A, Baltac? D, Türker1 Y, Türker Y, Iliev D, Öztürk S. Is the neutrophil-to-lymphocyte ratio indicative of inflammatory state in patients with obesity and metabolic syndrome? Anatol J Cardiol 2015; 15: 816-822.
- Kesk?n S, Sayal? E, Temeloglu E, Ek?zoglu ?. Obes?ty and ?nflammat?on.Turkiye Klinikleri J MedSci 2005; 25: 636-641.
- Nijhuis J, Rensen S.S, Slaats Y, vanDielen FM, Buurman WA, Greve JW. Neutrophil activation in morbid obesity, chronic activation of acute inflammation. Obesity 2009; 2014-2018.
- Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB. Elevated C-reactive protein levels in overweight and obese adults. JAMA 1999; 282: 2131-2135.
- Kim M-G, Cho B-H, Wan Chae S, Park T-S, Kim D.S. What do very low plasma concentrations of high-sensitivity C-reactive protein (hs-CRP) mean among healthy middle-aged Koreans? JLM 2015; 5: 14-20.
- Furuncuo?lu Y, Tulgar S, Do?an AN, Cakar S, Tulgar YK, Cakiro?lu B. How obesity affects the neutrophil/lymphocyte and platelet/lymphocyte ratio, systemic immune-inflammatory index and platelet indices: a retrospective study. Eur Rev Med Pharmacol Sci 2016; 20: 1300-1306.
- Laurson KR, McCann DA, Senchina DS. Age, sex, and ethnicity may modify the influence of obesity on inflammation. J Investig Med 2011; 59: 27-31.
- Lao XQ, Neil Thomas G, Jiang C, Zhang W, Adap P, Lam TH. White blood cell count and the metabolic syndrome in older Chinese: the Guangzhou Biobank Cohort Study. Atherosclerosis 2008; 201: 418-424.