Research Article - Biomedical Research (2017) Artificial Intelligent Techniques for Bio Medical Signal Processing: Edition-I
The prognostic impact of the coronary collateral circulation in patients with coronary artery disease: A meta-analysis
Huizheng Zhu*, Yudan Liang, Tian Zuo and Minzhou ZhangDivision of Chest Pain Center, Guangdong Provincial Hospital, the 2nd Clinical College of Guangzhou University of Chinese Medicine, Guangzhou, PR China
- *Corresponding Author:
- Huizheng Zhu
Division of Chest Pain Center Guangdong
Provincial Hospital The 2nd Clinical
College of Guangzhou University of Chinese Medicine, PR China
Accepted on January 18, 2017
Abstract
Background: Coronary Collateral Circulation (CCC) is an alternative source of blood supply to an ischemic myocardial region. The study of animal models showed that coronary collateral circulation on the myocardial had obvious protective effect of survival but it for humans the influence of the prognosis was still controversial.
Aims: The aim of this meta-analysis is to explore the impact of collateral circulation on prognosis.
Methods and Results: We performed an electronic literature search of PubMed, Embase, Chinese Biomedical Database (CBM), China National Knowledge Infrastructure (CNKI) Cochrane Library, assessed the association between coronary collateral circulation and prognosis, searched from the 1989 up to July 2016, there was no language restriction. A total of 16 studies enrolling 16447 participants were included in this analysis. Patients with high collateralization showed a reduced mortality compared with those with low collateralization Risk Ratios (RR) 0.66 [95% Confidence Intervals (CI) 0.54-0.82]; P=0.0001). The RR for ‘high collateralization’ showed a reduced incidence of re-infarction compared with those with low collateralization was 0.69 (95% CI: 0.52~0.92 p=0.01), in patients with Major Adverse Cardiovascular Events (MACE), it was (RR 0.62 [95% CI 0.46–0.84], p=0.002).
Conclusions: Abundant collateral circulation could reduce coronary heart disease mortality, recurrence of myocardial infarction and adverse cardiovascular events. However, in the revascularization, arrthythmia, cardiac death and so on, showed not reach statistical significance.
Keywords
Coronary collateral circulation, Prognosis.
Introduction
Coronary Heart Disease (CHD), or called Coronary Artery Disease (CAD), refers to a problem with the coronary arteries near the heart that supplies oxygen as well as nutrients to heart muscles, wherein the regional blood supply is not sufficient for delivering the oxygen required by the heart muscle. CHD is the top most cause of death in several developed nations, and makes up for around seventeen percent of all deaths as well as forty-nine percent of deaths due to cardio-vascular diseases in Australia. CHD is typically because of atheroma, which refers to fatty deposits in blood vessels; with an estimate that more than twenty percent of CHDs in the world are because of no physical activities or exercises [1]. For clinically stable patients with CHDs who are responsive to treatments, the advantages of physical activities are greater than the risks involved. Regular exercises are shown to be as efficient in secondary prevention as several drug interventions with none of the side effects that they induce. Exercises of moderate intensity has several advantages for individuals with CHDs: 1) prevention of narrowing of blood vessels (anti-atherosclerotic), 2) prevention of blood clotting (anti-thrombotic), 3) assists in the delivery of blood to heart (anti-ischaemic), as well as 4) assists in the maintenance of normal heart rhythm (anti-arrhythmic). This decreases the load on the heart when in rest as well as in the process of doing exercises. This in turn leads to decrease in the symptoms and reduction in the risk of death due to CHDs. Further advantages due to exercises for individuals with CHDs are: 1) enhanced physical functions, 2) psychological wellbeing, 3) favourable change in blood pressure, 4) high density lipo-protein (HDL) cholestrol, as well as 5) insulin sensitivity [2].
CHD, characterized by myocardial ischemia or necrosis caused by vascular stenosis or occlusion, is one of the leading causes of deaths and hospital admissions worldwide and constitutes the leading cause of disease burden in the world according to the 2010 Global Burden of Disease Study (GBD) [3]. The study of animal models showed that coronary collateral circulation on the Myocardial has obvious protective effect of survival but it for humans the influence of mortality and the prognosis is still controversial [4]. The statement that coronary arteries are pure end ones has been proven false for several years now. CCC links the epi-cardial coronary arteries in individuals with as well as without CAD. The collateral arteries are capable of remodelling as well as expanding in the event of an epi-cardial coronary artery stenosis, giving an alternate source of blood supply to at risk myocardium. In individuals with ST elevation infarction, a relevant protective role of collateral has been seen with regard to small infarct size, preserving cardiac functions post acute infarction, decrease in after infarct ventricular dilation, as well as postinfarct aneurysm formations. But, the typical effect of CCC on mortality is ambiguous. The goal of the systemic overview as well as meta-analysis is the integration of all present data for assessing the effect of CCC on mortality in individuals with stable or acute CADs [5]. There are some advantages to the present study. First of all, the related clinical researches in recent years are updated. Secondlythe study is relatively complete contains the outcome indicators related with prognosis of CHD such as MACE, Arrthythmia and so on.
Literature Review
Significant advantages of collaterals were established by Meier et al. [5] and Pascal Meier et al. [6]. Another meta-analysis by illustrates the relationship between Coronary collaterals and risk for restenosis after percutaneous coronary. Thus the metaanalysis by Akin et al. [7] discusses the effects of collaterals on deaths and re-infarctions .However, the above article lack of analysis to illustrate the influence of coronary collateral circulation on the prognosis of outcome indicators such as MACE, Revascularization, Arrhythmia and so on. Hoebers et al. [8] performed a metaanalysis and evaluated Left Ventricular Ejection Fraction (LVEF) prior as well as post Chronic Total Occlusions (CTO) Percutaneous Coronary Intervention (PCI) as well as long-term mortality. The current metaanalysis proves that successful re-canalization of a CTO led to considerable enhancement of 4.44 percent absolute LVEF points, decreased negative remodelling as well as enhancement of survival (OR: 0.52).
Akin et al. [9] studied predictors of poor coronary collaterals of 248 patient who had high-grade coronary stenosis or occlusion on their angiogram. For classification of CCC, the authors utilized the Rentrop classification. Individuals with poor CCC had considerably greater Neutrophil-to-Lymphocyte ratio (N/L) in comparison to the individuals with more developed CCC, (4.2 ± 2.8 vs. 3 ± 3.1, p=0.001), while mean platelet volume, red cell distribution width as well as uric acid were not considerably distinct. Logistic regression analysis proved that N/L ratio (odds ratio 1.199, 95% confidence interval 1.045-1.375) as well as serum triglyceride levels [Odds Ratio (OR)=1.006, 95% CI=1.001-1.010] were independent predictors of poorly developed CCC. Zimarino et al. [10] conducted a metaanalysis of research that reported on clinical results of individuals with Multi-Vessel Coronary Artery Diseases (MVCAD) who got treatment with CR as well as IR, with exhaustive (>80%) usage of stents for PCI or arterial conduits in Coronary Artery Bypass Graft (CABG). Relative Risk (RR) as well as 95 percent confidence interval (CI) for all-cause mortality were evaluated as the primary endpoint, while Myocardial Infarction (MI) as well as repeat revascularization were the secondary endpoint.
Materials and Methods
Document retrieval method
We performed an electronic literature search of PubMed, Embase, CBMCNKI Cochrane Library, assessed the association between coronary collateral circulation and prognosis. Searched from the 1989 till July 2016, there was no language restriction, search terms included ‘collateral circulation’, ‘prognosis’, in addition, we also hand-searched the bibliographies of all relevant reviews and the selected articles for other potential studies. Our systematic review and meta-analysis was conducted according to the checklist of Meta-analysis of Observational Studies in Epidemiology (MOOSE) [11], and the Preferred Reporting Items for Systematic reviews and Meta-Analyses guidelines (PRISMA) [12].
Rules of the documents incorporation
The rules that the literature could be incorporated into this study included: Content of coronary collateral follow study on the prognosis of patients with coronary heart disease clinical research in both Chinese and English articles. Observation method of the literature on coronary collateral circulation is clear, on the basis of basis rentrop grade or collateral circulation collateral blood flow number of CFI. Can offer data directly or via get full text in full Computed data available to prognosis, and the following documents were excluded: Case reports, review the literature, the original data is not complete and the same or similar, in vain to contact the author, Choose one of the most complete data references included.
Filtering and extraction of the data
Two investigators independently extracted data from all of the included studies using a standardized excel file. Disagreements were resolved by consensus. The following information on study characteristics was extracted from each article: first author, Publication year, Group, age, Female, Outcome and multivariable-adjusted or unadjusted risk estimates and their 95% CI.
Quality evaluation of the references
Based on the Newcastle-Ottawa Scale (NOS) [13] evaluation criteria, the quality assessments were carried out for the documents, so as to examine whether there is a bias in the documents and the extent of its impact (Table 1). Selection of research objects: the determination of the cases; the representation of the cases; the selection of control objects; the determination of control objects; each item was 1 points, respectively. Comparability between groups: the comparability of cases and controls needed to be considered in the design and statistical analysis; this entry was 2 points. Exposure factor measurement: the determination of exposure factors; the same method was to determine the exposure factors of patients and control group; No response rate. The determination of exposure factors was 2 points and other exposure factor measurements were 1 points. The total score was greater than or equal to 5 points then the quality was reliable.
| Lead author | Representativeness | Control Group | Ascertainment | Endpoint not presentat start | Assessment Ofoutcome | Follow-up duration | Adequacy follow-up |
|---|---|---|---|---|---|---|---|
| Hansen | * | * | * | * | * | * | |
| Perez | * | * | * | * | * | ||
| Antioniucci | * | * | * | * | * | * | |
| Monteiro | * | * | * | * | * | ||
| Xueling | * | * | * | * | * | ||
| Meier | * | * | * | * | * | * | * |
| Regieli | * | * | * | * | * | * | |
| Desch | * | * | * | * | * | * | |
| Steg | * | * | * | * | * | ||
| Llia | * | * | * | * | * | ||
| Tomasz | * | * | * | * | * | * | |
| Laiwenwen | * | * | * | * | * | ||
| Seiler | * | * | * | * | * | * | |
| Angela | * | * | * | * | * | * | |
| Monteiro | * | * | * | * | * | * | |
| Hara | * | * | * | * | * | * |
Table 1. Evaluation of the quality of the sixteen included studies by using the Newcastle-Ottawa Scale.
Definitions
Collateral circulation was studied as per the Rentrop grading system from “0” to “3”. Grade 0: undeveloped no filling of collateral vessel; Grade 1: lesser developed filling of sides of arteries, however no main trunk visualised via collateral; Grade 2: more developed partial filling of epi-cardial part of stenosed arteries via collateral; and Grade 3: entire filling of epi-cardial part [14]. On the basis of Rentrop Grading, the examined patients were split into two sets: those with poor collateral (grades 0 & 1), as well as those with good collateral (grades 2 & #). Correlation of duration of hypertension was performed through grading collateral.
Evaluation of coronary collateral circulation in most study is a method of using coronary angiography under visual Rentrop Grading, grading level is considered to be less than 1 of coronary collateral circulation is not rich. Rich, more than 2 grade level for the coronary collateral circulation is abundant. In the study, the grading of coronary collateral circulation is not rich (Rentrop 0). Abundant collateral circulation (Rentrop 1-3). The number of CFI was evaluated, and the CFI <0.25 was considered as the coronary collateral circulation is not rich, CFI=0.25 for coronary collateral circulation is abundant.
Statistical methods
The statistical analysis of the data was carried out by the use of Review Manager 5.3, the differences of statistical significance were compared by the use of p=0.05, and the fixed effect model and random effect model of the two kinds of modeling methods were used to merge the data. The random effects model was used when the statistical heterogeneity (p<0.05), and the random effect model was used in the good homogeneity. Besides, analysis of "funnel plot" in the production of bias of literature results was carried out, and the research literature was analyzed according to the influencing factors.
Results
Search results
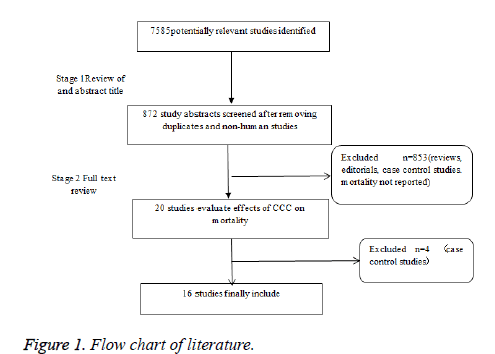
Among 7585 potentially relevant citations, 872 articles were considered of interest and fully reviewed. Of these 857 studies were excluded because of use of 1) reviews; 2) editorials; 3) case control studies; 4) mortality and prognosis not reported (Figure 1). Therefore a total of 16 trials [15-28] were finally included.
Document statistics of the rule
16 documents were chosen as the research objects, there were 16447 participants. (Table 2). The included studies were published from1989 to 2016.
| Study | Year | Follow (months) | PCI | Group | Mean age (y) | Female (%) | endpoints |
| Hansen | 1989 | 120 | No | High CCC Low CCC | 49.2 47.9 | 10 7 | mortality |
| Perez | 1999 | In-hospital | No | High CCC Low CCC | 64.0 64.0 | 18 18 | mortality |
| Antioniucci | 2002 | 6 | Yes | High CCC Low CCC | 63 64 | 18 18 | mortality re-infarction revascularization MACE |
| Monteiro | 2003 | 15.7 | Yes | High CCC Low CCC | 63.3 65.3 | 11 10 | mortality re-infarction MACE heartfailure、recurrent angina pectoris |
| Xueling | 2003 | In-hospital | Yes | High CCC Low CCC | 62 58 | na na | mortality |
| Meier | 2007 | 120 | Yes | High CCC Low CCC | 61.0 62.0 | 21 24 | mortality re-infarction |
| Regieli | 2009 | 24 | Yes | High CCC Low CCC | 57.0 56.0 | na na | mortality re-infarction MACE cardiac death |
| Desch | 2009 | 6 | Yes | High CCC Low CCC | 64.0 66.0 | 26 24 | mortality MACE |
| Steg | 2010 | 60 | 50% PCI | High CCC Low CCC | 58.4 60.4 | 23 20 | mortality re-infarction heart failure |
| Llia | 2011 | 84 | Yes | High CCC Low CCC | 54 59 | na na | mortality |
| Tomasz | 2012 | 24 | Yes | High CCC Low CCC | 59 57 | 24 29 | mortality revascularization |
| Laiwenwen | 2013 | In-hospital | Yes | High CCC Low CCC | 64.76 62.13 | 19.8 14.6 | mortality MACE arrhythmia heart failure recurrent angina pectoris |
| Seiler | 2014 | 84 | Yes | High CCC Low CCC | 61 62 | na na | mortality re-infarction revascularization MACE cardiac death stroke |
| Angela | 2014 | 12 | Yes | High CCC Low CCC | 62 60 | 24 33 | mortality re-infarction revascularization arrhythmia heart failure recurrent angina pectoris stroke |
| Meier | 2014 | 12 | Yes | High CCC Low CCC | 61 60 | 24 38 | mortality |
| Hara | 2016 | 60 | Yes | High CCC Low CCC | 64.5 65 | 22.1 22.1 | mortality |
CFI:Collateral Flow Index; CCCL:Coronary Collateralization; na: not available; PCI:Percutaneous Coronary Intervention.
Table 2. Characteristics of the sixteen studies included in the meta-analysis.
Mortality
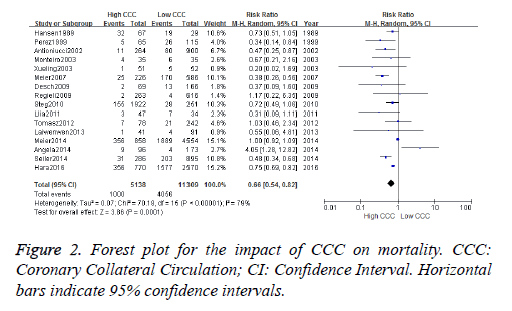
All causes mortality was observed in 1000 out of 5138 patients (19.4%) patients in High CCC versus 4056 out of 11309 patients (45.4%) in Low CCC (RR [95% CI]=0.66 [0.54-0.82], p=0.0001; z=3.86), to heterogeneous data into 16 documents, according to the inspection. There is heterogeneity among studies (chi-square=70.18, P<0.00001, I2=79%), the random utility model meta analysis is adopted to produce. Forest plot show difference is statistically significant (Z=3.86 p=0.0001). A value of RR is 0.66 (95% CI: 0.54~0.82), illustrates that coronary collateral group of patients, mortality is lower than no coronary collateral circulation (Figure 2).
Re-infarction
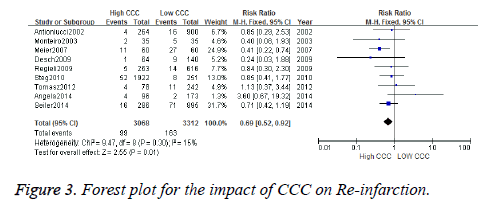
Data regarding myocardial infarction were available in 262 patients. Re-infarction was observed in 99 out of 3068 patients in High CCC versus 163 out of 3312 patients in Low CCC (RR [95% CI]=0.69 [0.52-0.92], p=0.01; z =2.55), to heterogeneous data into 9 documents, according to the inspection. There is heterogeneity among studies (chi-square=9.47, P=0.30, I2=15%), the fixed utility model meta analysis is adopted to produce. Forest plot showed difference was statistically significant (Z=2.55, p=0.01). A value of RR 0.69 (95% CI: 0.52~0.92), showed that the incidence of re-infarction of High CCC less than Low CCC (Figure 3).
Revascularization
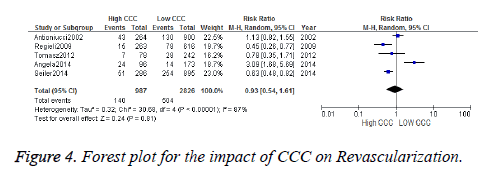
Data regarding revascularization were available in 644 patients. Revascularization was observed in 140 out of 987 patients in High CCC versus 504 out of 2826 patients in Low CCC (RR [95% CI]=0.93 [0.54-1.61], p=0.81; z=0.24), to heterogeneous data into 5 documents, according to the inspection. There is heterogeneity among studies (chisquare= 30.68, P<0.00001, I2=87%), the random utility model meta analysis is adopted to produce. Forest plot showed difference was no statistically significant (Z=0.24, p=0.81) RR .A value of 0.93 (95% CI: 0.54~1.61), showed that the incidence of revascularization of High CCC and Low CCC had no statistical significance (Figure 4).
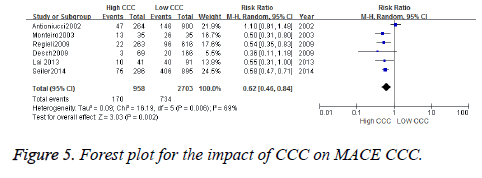
Mace
Data regarding MACE were available in 904 patients. MACE was observed in 170 out of 958 patients in High CCC versus 734 out of 2703 patients in Low CCC (RR [95% CI]=0.62 [0.46-0.84], p=0.002; z=3.03), to heterogeneous data into 6 documents, according to the inspection. There is heterogeneity among studies (chi-square=16.19, P=0.006, I2=69%), the random utility model meta analysis is adopted to produce. Forest plot showed difference was statistically significant (Z=3.03 p=0.002) RR. A value of 0.62 (95% CI: 0.46~0.84), showed that the incidence of MACE of High CCC less than Low CCC (Figure 5).
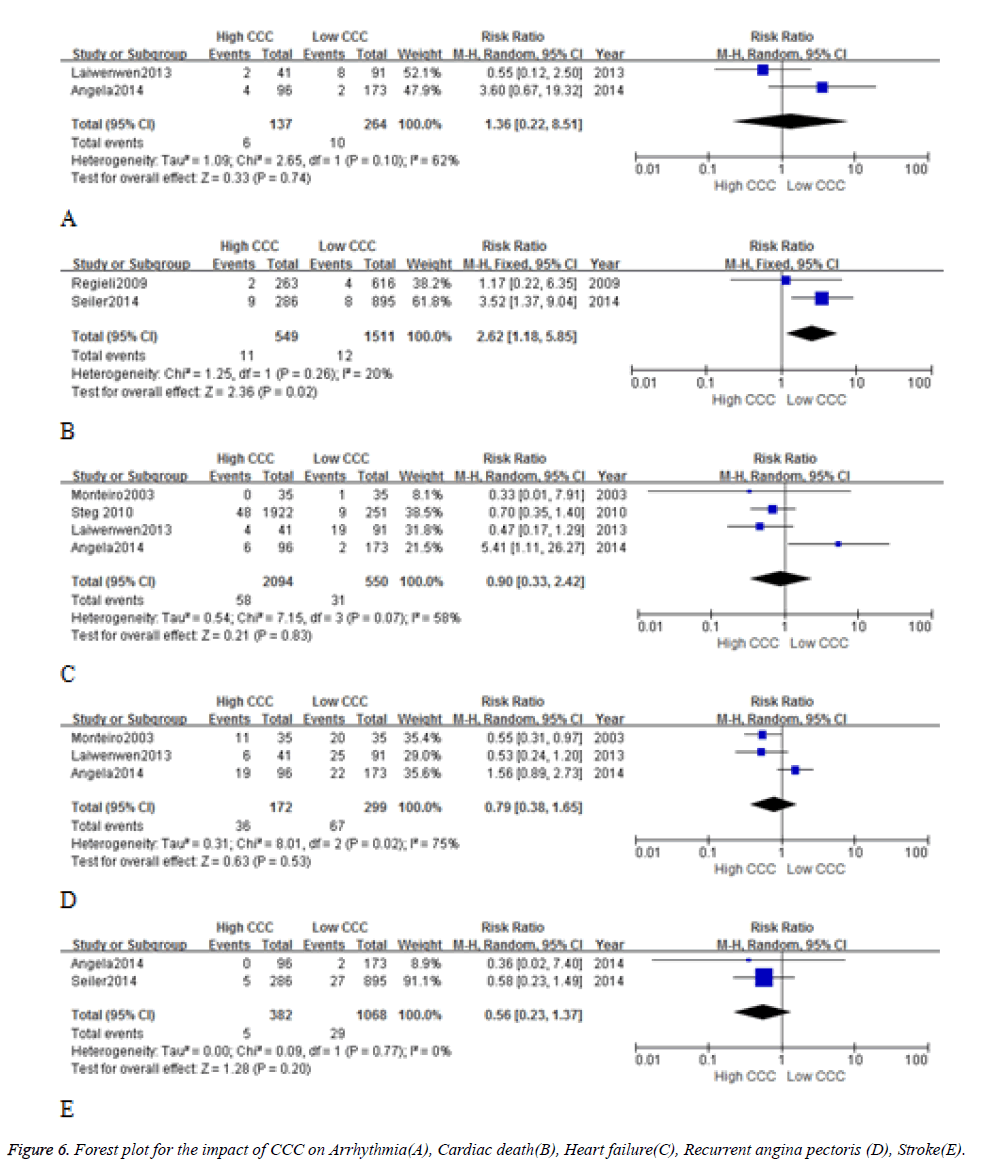
Arrhythmia, Cardiac death, Heart failure, Recurrent angina pectoris, Stroke
In Arrhythmia(A), Cardiac death(B), Heart failure(C), Recurrent angina pectoris (D), Stroke(E) the incidence in High CCC group and Low CCC group have no statistical and clinical significance (Figure 6).
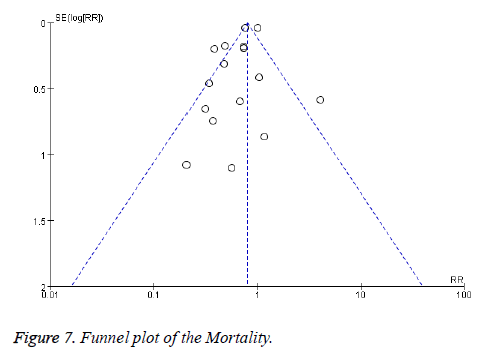
Publication bias
For the above analyses comparing High CCC and Low CCC with Prognosis, In this paper, to analyze the bias of the publication of the 16 articles, and the funnel diagram was drawn (Figure 7), there was no statistical significance in the likelihood of occurrence of bias, therefore, there was no publication bias in the published articles.
Sensitive analysis
Sensitivity analyses by excluding any single study at each turn indicated that there were no changes in the direction of pooling risk estimate of all-cause mortality (pooled RR ranges from 0.61 to 0.71) (Table 3).
| Study | Model | RR(95%CI) | P |
|---|---|---|---|
| Overall | Random | 0.66 | 0.0001 |
| Omitting Hansen 1989 | Random | 0.65 | 0.0002 |
| OmittingPerez1999 | Random | 0.68 | 0.0004 |
| Omitting Antioniucci 2002 | Random | 0.68 | 0.0004 |
| Omitting Monteiro 2003 | Random | 0.66 | 0.0002 |
| Omittingxueling2003 | Random | 0.67 | 0.0002 |
| Omitting Meier 2007 | Random | 0.71 | 0.0009 |
| Omitting Regieli 2009 | Random | 0.66 | 0.0001 |
| Omitting Desch 2009 | Random | 0.67 | 0.0002 |
| Omitting Steg 2010 | Random | 0.65 | 0.0002 |
| Omitting Llia 2011 | Random | 0.67 | 0.0002 |
| Omitting Tomasz2012 | Random | 0.65 | 0.0001 |
| Omittinglai2013 | Random | 0.66 | 0.0001 |
| Omitting Seiler2014 | Random | 0.69 | 0.0007 |
| Omitting Angela2014 | Random | 0.63 | 0.0001 |
| Omittingmier2014 | Random | 0.61 | 0.0001 |
| Omitting Hara2016 | Random | 0.64 | 0.005 |
Table 3. Sensitive analyses for the impact of CCC on Mortality.
Discussion
The result showed that compared with the poor collateral, wellcollateralized group could obviously reduce mortality and incidence of re-infarction and MACE, however in the revascularization, arrhythmia, cardiac death and so on, showed not reach statistical significance. According to the present research, The CCC can improve the survival rate of patients with coronary heart disease and the accuracy of the mechanism is still not clear, may be mainly due to the following aspects. First, the collateral circulation is an important compensatory mechanism of myocardial ischemia. The narrow degree of coronary artery narrow is an important factor in the formation of collateral circulation. The incidence of collateral circulation was 97%~68%. 5%~41% was significantly increased, while the stenosis was less than 90% of the collateral circulation rarely open. Therefore, when a certain part of the myocardial ischemia, normal the potential of microvascular open change between myocardium and ischemic myocardium Coarse, forming a functional collateral circulation, to a certain extent improving myocardial ischemia in this area. Second, the collateral circulation can be reduced Infarct size and cardiac function. Dewood reported in acute Q wave in myocardial infarction, collateral circulation can change the infarct type, reduced infarct size and even the occurrence of myocardial infarction. The establishment of collateral circulation after myocardial infarction can prevent left ventricular remodelling, to reduce the incidence of left ventricular aneurysm. Third, the collateral circulation can be prevent and reduce the occurrence of adverse cardiovascular events, and abundant collateral circulation can reduce the incidence of ventricular arrhythmia, thereby reducing the incidence of ventricular arrhythmia. Occurrence of adverse cardiovascular events such as fibrillation and sudden death, coronary collaterals are an important factor that can potentially alter morbidity and mortality in ischemic heart disease.
The present meta-analysis lack of the prognosis of outcome indicators such as MACE, Arrhythmia, Cardiac death, Stroke and so on. There are some advantages to the present study. First of all, the related clinical researches in recent years are updated. Secondlythe study is relatively complete contains the outcome indicators related with prognosis of CHD such as MACE, Arrhythmia and so on Nevertheless, there are some several limitations in the present meta-analysis. The data included in this analysis are both observational studies. The studies were associated with extensive coronary collateral circulation and prognosis. The causal relationship is hypothesized to exist, and only the intervention of the study is set up. The number of patients was small.
References
- Lim SS, Vos T, Flaxman AD. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet 2012; 380: 2224-2260.
- Murray CJ, Lopez AD. Measuring the global burden of disease. N Engl J Med 2013; 369: 448-457.
- Celik T, Celik M, Iyisoy A. Coronary collateral circulation. Turk KardiyolDernArs 2010; 38: 505-514.
- Sorajja P, Gersh BJ, Mehran R. Impact of collateral flow on myocardial reperfusion and infarct size in patients undergoing primary angioplasty for acute myocardial infarction. Am Heart J 2007; 154: 379-384.
- Meier P, Hemingway H, Lansky AJ, Knapp G, Pitt B. The impact of the coronary collateral circulation on mortality: a meta-analysis. Eur Heart J 2012; 33: 614-621.
- Meier P, Indermuehle A, Pitt B, Traupe T, de Marchi SF, Crake T, Knapp G, Lansky AJ, Seiler C. Coronary collaterals and risk for restenosis after percutaneous coronary interventions: A meta-analysis. BMC Medicine 2012; 10: 62.
- Akin S, Yetgin T, Brugts JJ, Dirkali A, Zijlstra F. Effect of collaterals on deaths and re-infarctions in patients with coronary artery disease: a meta-analysis. Neth Heart J 2013; 21: 146-151.
- Hoebers LP, Claessen BE, Elias J, Dangas GD, Mehran R, Henriques JP. Meta-analysis on the impact of percutaneous coronary intervention of chronic total occlusions on left ventricular function and clinical outcome. Int J Cardiol 2015; 187: 90-96.
- Akin F, Ayça B, Çelik Ö, Sahin C. Predictors of poor coronary collateral development in patients with stable coronary artery disease: Neutrophil-to-lymphocyte ratio and platelets. Anatol J Cardiol 2015; 15: 218-223.
- Zimarino M, Ricci F, Romanello M, Di Nicola M, Corazzini A, De Caterina R. Complete myocardial revascularization confers a larger clinical benefit when performed with state-of-the-art techniques in high-risk patients with multivessel coronary artery disease: A meta-analysis of randomized and observational studies. Catheterization Cardiovascular Intervent 2016; 87: 3-12.
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. J Am Med Assoc 2000; 283: 2008-2012.
- Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2010; 8: 336-341.
- Hansen JF. Coronary collateral circulation: clinical significance and influence on survival in patients with coronary artery occlusion. Am Heart J 1989; 117: 290-295.
- Hossain S, Majumder AAS, Ullah M, Shaha CK, Mannan MA. Association of Hypertension on Development of Coronary Collaterals in Severe Coronary Artery Disease. Cardiovascular J 2015; 7: 98-103.
- Pérez-Castellano N, García EJ, Abeytua M, Soriano J, Serrano JA. Influence of collateral circulation on in-hospital death from anterior acute myocardial infarction. J Am CollCardiol 1998; 31: 512-518.
- Antoniucci D, Valenti R, Moschi G, Migliorini A, Trapani M. Relation between preintervention angiographic evidence of coronary collateral circulation and clinical and angiographic outcomes after primary angioplasty or stenting for acute myocardial infarction. Am J Cardiol 2002; 89: 121-125.
- Monteiro P, Antunes A, Gonçalves LM, Providência LA. Long-term clinical impact of coronary-collateral vessels after acute myocardial infarction. Rev Port Cardiol 2003; 22: 1051-1061.
- Ling X. Collateral circulation infarction area Heart muscle stem dead area in patients with acute myocardial infarction and heart function [D] the influence of hebei, hebei medical university, 2003.
- Meier P, Zbinden R, Togni M, Wenaweser P, Windecker S. Coronary collateral function long after drug-eluting stent implantation. J Am CollCardiol 2007; 49: 15-20.
- Regieli JJ, Jukema JW, Nathoe HM, Zwinderman AH, Ng S. Coronary collaterals improve prognosis in patients with ischemic heart disease. Int J Cardiol 2009; 132: 257-262.
- Desch S, Eitel I, Schmitt J, Sareban M, Fuernau G, Schuler G, Thiele H. Effect of coronary collaterals on microvascularobstruction as assessed by magnetic resonance imaging in patients with acute ST-elevation myocardial infarction treated by primary coronary intervention. Am J Cardiol 2009; 104: 1204-1209.
- Steg PG, Kerner A, Mancini GB, Reynolds HR, Carvalho AC. Impact of collateral flow to the occluded infarct-related artery on clinical outcomes in patients with recent myocardial infarction: a report from the randomized occluded artery trial. Circulation 2010; 121: 2724-2730.
- Rechciñski T, Jasinska A, Peruga JZ. Presence ofcoronarycollaterals in ST-elevation myocardial infarction patients doesnotaffectlong-termoutcome. polskiearchiwummedycynywewnctrznej 2013; 123: 1-2.
- Wenwen L. To investigate the early phase of the collateral circulation in st-elevation acute anterior wall myocardial infarction Direct effects of patients with PCI treatment. Wide east, southern medical university, 2013.
- Seiler C, Engler R, Berner L, Stoller M, Meier P. Prognostic relevance of coronary collateral function: confounded or causal relationship? Heart 2013; 99: 1408-1414.
- Kloepfer AM, Lipson LC, Keeley EC. The Presence of Angiographic Collaterals in non-ST Elevation Myocardial Infarction is a P redictor of Long-Term Clinical Outcomes. Catheter CardiovascInterv 2014; 83: 1-8.
- Meier P. The impact of the coronary collateral circulation on outcomes in patients with acute coronary syndromes: results from the ACUITY trial Heart 2014; 100: 647-651.
- Hara M. Impact of coronary collaterals on in-hospital and 5-year mortality after ST-elevation myocardial infarction in the contemporary percutaneous coronary intervention era: a prospective observational study. BMJ Open 2016; 6: e011105.