Research Article - Journal of Public Health and Nutrition (2022) Volume 5, Issue 4
Assess the magnitude of under nutrition and associated factors among pregnant women attending antenatal care service in public hospitals of Western Ethiopia.
Haile Bikila*
Department of Public Health, Wollega University, Nekemte, Western Ethiopia
- *Corresponding Author:
- Bikila H
Department of Public Health
Wollega University
Nekemte
Western Ethiopia
E-mail: haile.bikila@gmail.com
Received: 23-Dec-2021, Manuscript No. AAJPHN-21-50525; Editor assigned: 27-Dec-2021, Pre QC No. AAJPHN-21-50525(PQ); Reviewed: 11-Jan-2022, QC No. AAJPHN-21-50525; Revised: 11-Apr-2022, Manuscript No. AAJPHN-21-50525(R); Published: 18-Apr-2022, DOI: 10.35841/aajphn-5.4.116
Citation: Bikila H. Assess the magnitude of under nutrition and associated factors among pregnant women attending antenatal care service in public hospitals of Western Ethiopia. J Pub Health Nutri. 2022;5(4):116
Abstract
Background: Pregnancy is a time when the body is under a lot of stress, which increases your dietary needs. Under nutrition is a worldwide health issue, especially among pregnant women. Malnutrition during pregnancy can result in miscarriages, fetal deaths during pregnancy, preterm delivery, and maternal mortality for both the mother and her fetus. Therefore, this research was aimed to assess the magnitude of under nutrition and associated factors among pregnant women attending antenatal care services at public hospitals at Western Ethiopia. Objective: To assess the magnitude of under nutrition and associated factors among pregnant women attending Antenatal Care service in Public Hospitals of western Ethiopia. Methods: Facility based cross-sectional study was conducted from April 10 to May 10, 2020 among 780 pregnant mothers. The study participants were selected by systematic random sampling methods from antenatal care clinics of the hospitals. Interviewer administered structured questionnaire was used to collect the data and Mid-upper arm circumference, height and weight were measured to determine the magnitude of under nutrition among the study participants. The data were entered to Epi Info version 7.2.3, and then exported to SPSS version 24 for analysis. Multivariable logistic regression was used to identify independent predictors considering Adjusted Odd Ratio (AOR) at p-value ≤ 0.05 to measure the strength of association between dependent and independent variables. Result: The magnitude of under nutrition among pregnant women was found to be 39.2% (95%CI: 35.7%, 42.6%). Rural residence [(AOR=1.97, 95% CI: (1.24, 3.14)], substance use [(AOR: 3.33, 95% CI: (1.63, 6.81)], low dietary diversity of women [(AOR= 7.56, 95% CI: (4.96, 11.51)], mildly food insecure household [(AOR= 4.36, 95% CI: (2.36, 8.79)], moderately food insecure household [(AOR= 3.71, 95%CI: (1.54, 8.79), and severely food insecure household [(AOR= 6.96, 95% CI: (3.15, 15.42)] were factors significantly associated with under nutrition. Conclusion: The study showed that the magnitude of under nutrition is very high among pregnant women. Factors associated with under nutrition of pregnant women were rural residency, household food insecurity, dietary diversity and substance use. Therefore, all concerned bodies should made efforts to reduce the risk of under nutrition by reducing substance use and improving household food security there by to increase women’s dietary diversity.
Keywords
Under nutrition, Pregnancy, Associated factor.
Abbreviations
ANC: Antenatal Care; AOR: Adjusted Odds Ratio; COR: Crude Odds Ratio; DALYs: Disability Adjusted Life Years; FAO: Food And Agricultural Organization; FFQ: Food Frequency Questionnaire; GDP: Gross Domestic Product; GHI: Global Hunger Index; HFIAS: Household Food Insecurity Access Scale; MCH: Maternal And Child Health; MDDW: Minimum Dietary Diversity Of Women; MUAC: Mid Upper Arm Circumference; SDGs: Sustainable Development Goals; UN: United Nations; UNICEF: United Nations International Children’s Emergency Fund; USA: United States of America; WHO: World Health Organization
Background
Under nutrition is the result of inadequate intake of food in terms of either quantity or quality, poor utilization of nutrients due to infections or other illnesses, or a combination of these immediate causes [1]. Pregnancy strongly depends on the health and nutritional status of women and a high proportion of pregnant women are affected by poor nutrition which leads them to unhealthy and distress conditions. Under nutrition goes beyond calories and signifies deficiencies in any or all of the following: energy, protein, and/or essential vitamins and minerals [2].
Pregnancy constitutes states of considerable physiological stress, which cause increased nutritional demands. If these demands are in adequate, not only the nutritional status of the subject will affect, but also the course of pregnancy and lactation. Nutrition-related problems form the core of many current issues in women’s health, and poor nutrition can have profound effects on reproductive outcomes [3]. Lack of adequate nutrition of good quality and quantity during pregnancy can cause health problems for both the mother and her fetus. Under nutrition is among the most common causes of maternal mortality [1,4].
The prevalence of undernourishment-the percentage of the population without regular access to adequate calories-has stagnated since 2015, and the number of people who are hungry has actually risen to 822 million from 785 million in 2015 [1]. Expectant and nursing mothers, infants and children constitute the most vulnerable segments of a population from the nutritional standpoint. The Global Burden of Disease Study 2013 identified that maternal and child malnutrition causes 1.7 million deaths and 176.9 million DALYs (Disability Adjusted Life Years) [5]. A survey carried out in South India revealed that among poor women whose dietaries during pregnancy provided 1400-1500 calories and about 40 g of protein daily, nearly 20% of pregnancies had terminated in abortions, miscarriages or stillbirths [6].
Maternal under nutrition directly or indirectly causes about 3.5 million deaths of women in developing countries [7]. In developing countries, it has been estimated that poor nutritional status in pregnancy accounts for 14% of fetuses with IUGR (Intra Uterine Growth Retardation), and maternal stunting account for a further 18.5% [8]. If adolescents or women are undernourished during pregnancy, the cycle of maternal malnutrition, fetal growth restriction, child stunting, subsequent lifetime of impaired productivity, and increased maternal and fetal morbidity and mortality are continued [9].
Under nutrition among women in reproductive age is significantly higher in Africa due to chronic energy and/ or micronutrient deficiencies especially during pregnancy [10,11]. In developing nations the prevalence of under nutrition among pregnant women ranges from 13% to 38% [12,13]. The situation is worse in Africa that the burden of malnutrition among pregnant women is about 23% [14].
A 2018 WHO (World Health Organization) African region report indicates, nine countries in Africa had a prevalence rates above 15%, this includes Ethiopia in which maternal underweight exceeds 20% [15]. Recent study done among young pregnant mothers in Ethiopia indicates the prevalence of under nutrition is 38% [16]. Individual studies across Ethiopia indicates high rates of under nutrition among pregnant women, ranging from 9.2% to 44, 9% [17-24], making Ethiopia to be one of the countries with highest burden of maternal under nutrition from the world.
Malnutrition is holding back development with unacceptable human consequences [1]. Globally, hunger and malnutrition reduce a Gross Domestic Product (GDP) of a given country by 1.4-2.1 trillion United States Dollar (USD) a year. Similarly, malnutrition costs between 3 and 16% annual GDP of the 54 African countries, and for mentioning Ethiopia loss 16.5% a year [25,26].
Despite efforts made to improve the problem; the progress made in last decade was very low, and currently the burden of under nutrition is continued to be the major public health problem in developing countries including our country Ethiopia [3]. Different studies done across our country tried to show the burden and determinant of under nutrition among pregnant women, in any consideration of the problems of under nutrition, these segments require special consideration. As under nutrition caused by complex interrelated factors the programs and interventions designed to reduce its burden should depend on the reliable and recent information derived from extensive studies targeting this segment of population. Therefore, this study intended to provide valuable information to contribute to existing knowledge on the nutritional status of pregnant women at national and local level.
Materials and Methods
Study design, area, and period
An institution-based cross-sectional study design was carried out. This study was conducted in public general hospitals of the Oromia region. The study was conducted in five public hospitals in the zone were the selected study area. This study was conducted in Public Hospitals of western Ethiopia from April 10 to May 10, 2020.
Source and Study population
The source populations were all third-trimester pregnant women who were coming for delivery and antenatal care visits in the selected public general hospitals of the Oromia region. Third-trimester pregnancy women who were coming for antenatal care visits in general public hospitals of the Oromia region western part were selected as the study population.
Inclusion and exclusion criteria
All selected third-trimester pregnant women who were coming for ANC in public general hospitals during the study period were included, whereas pregnancy women with bilateral edema, who were seriously sick and unable to respond to the interview, were excluded from the study.
Sample size and Sampling techniques
Sample size was calculated using double population proportion formula by assuming precision OR (Odd ratio) 1.52 (d) =5%, confidence level =95% (Ζα/2=1.96), and proportion of under nutrition (P1 proportion among exposed group) 49.5%, (p2 proportion among exposed group) 39.2%. By, it becomes 768. By considering a 5% non-response rate, 806 pregnant women were taken as a final sample size after using the design effect two.
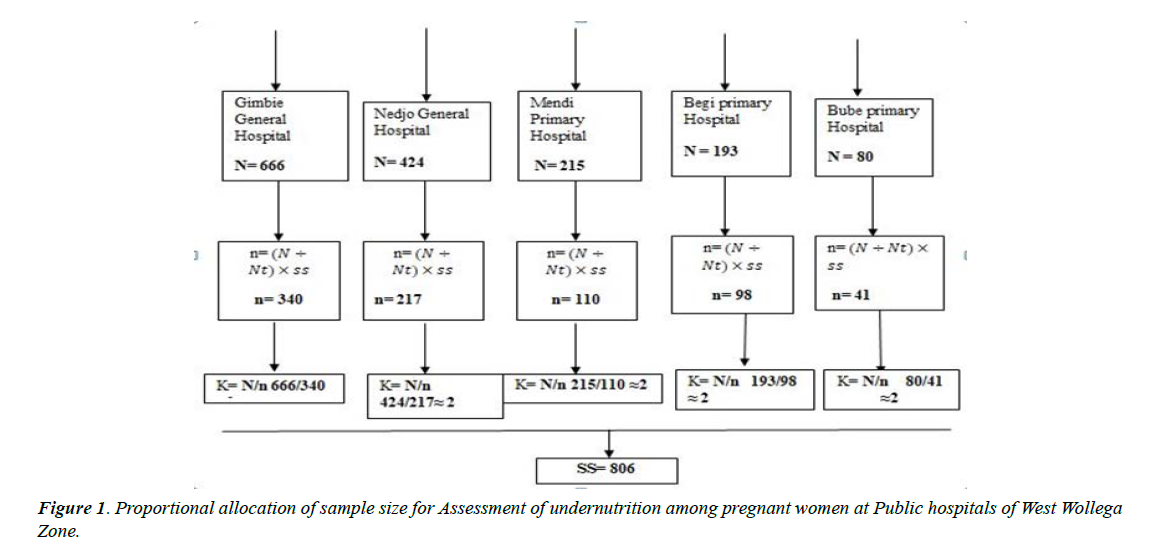
The sample size was allocated proportional to their average monthly client flow. Systematic sampling was used to select the study units from pregnant women attending ANC. The interval K value was determined for samples at each hospital by dividing the number of units in the population (N) by the desired sample size (n). The first respondent selected by lottery method, and then every second respondent was included until the desired sample size was attained (Figure 1).
Data collection procedure
A semi-structured questionnaire was initially prepared in English and then translated into the regional language; Afaan Oromo was used. Afaan Oromo version was again translated back to English to check for any inconsistencies or distortion in the meaning of words. Data were collected using an interviewer-administered, and MUAC measurement questionnaire was adapted from the literature. Data collection was performed by one BSc Nurse as supervisor and five Midwifery nurses (Diploma) were employed for data collection. To assure the quality of the data properly designed data collection instrument and training of data collectors and supervisors was done, the enumerators and the supervisor were given training for three days on procedures, techniques, ways of collecting the data, and monitoring the procedure especially on anthropometric measurement. Ten percent pretest was done at the, Gida public general hospital to check the consistency of the questioner. The collected data were reviewed and checked for completeness by supervisors and principal investigators each week. MUAC was measured by considering the mothers in Frankfurt plane and sideways to measure the left side, arms hanging loosely at the side with the palm facing inward, taken at marked midpoint of upper left arm, a flexible non stretchable tape were used, and difference between trainee and trainer was 0-5 mm after standardization of measurement error calculation before data collection.
Independent and dependent variable
Nutritional status of pregnant mothers is the outcome variable, and the independent variables were all the sociodemographic characteristics, dietary habit, environmental, maternal obstetrical and gynecology history. A brief description of how some of these variables were measured is as follows.
Dependent variable
The mid-upper arm circumstance values below a cutoff point <23 cm were considered as under nutrition in this study, whereas for the individual 23 cm and above, was considered normal [13].
Potential confounding factor
Potential confounding variables measured in the study were socio-demographic characteristics, obstetrics and gynecology including the age of mother, marital status, religion, educational background of mothers, women’s decision-making autonomy, household income, occupation, ethnicity, number of antenatal care visits, type of pregnancy, maternal previous surgery, malaria, parity, iron and folic acid supplementation, marriage at age, substance use, hemoglobin level, coffee intake, husband’s support, difficulty to access food during the last three months, Dietary diversity, household food insecurity, prenatal feeding habits like skipping meals, frequency of meal, habit of eating snack, food avoidance, and food intake and history of low birth weight.
Anthropometric measurement
The anthropometric measurement mid upper arm circumstance was taken from individual third-trimester pregnant women. Intra-observer and inter-observer variability of anthropometric measurement were assessed on 10 volunteers to reduce Technical Error of Measurement (TEM) at end of training. The measuring instruments were calibrated after each session of measurements. The Supervisor gave close supervision and technical supports, and checked the collected data for completeness, accuracy, and consistency every day and onsite.
Results
Socioeconomic and demographic characteristics of pregnant women
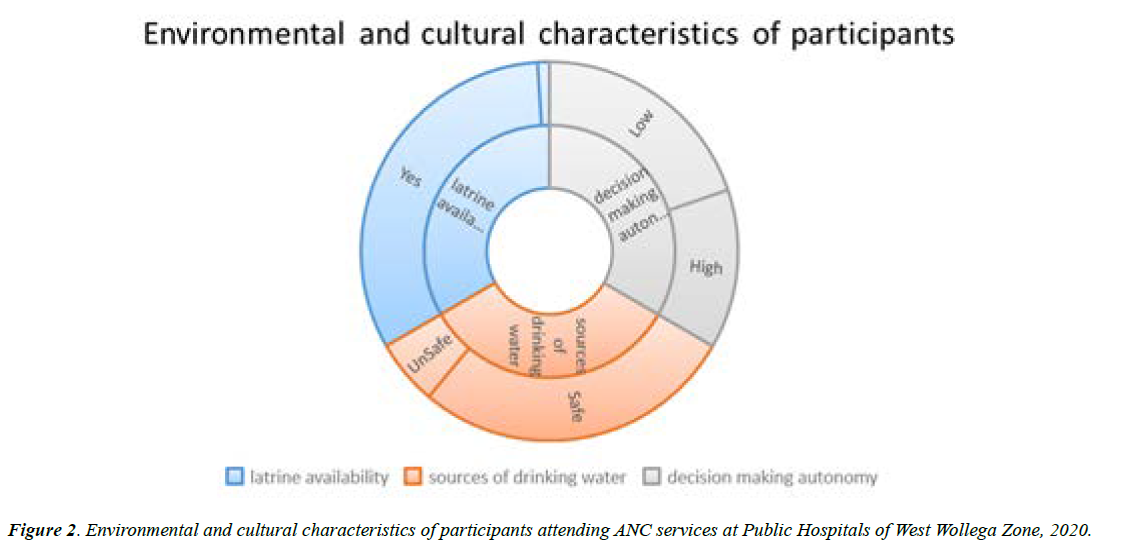
Out of 806 pregnant initially planned to be included in the study, 780 of them were participated with 96.8% response rate. The mean (± SD) age of respondents was 26 ± 5.32. The median family size of respondents was three persons. Majorities (64.7%) of respondents were Protestant, and about 20% were Orthodox follower. All most all of the participants (97.7% were married. Majority (53.1%) of respondents are urban dwellers while the rest (46.9%) are rural residents. About 24% of respondents completed tertiary education while only 8% had no formal education. Nearly half (48.6%) of participants were Housewife, and only 6.4% of them were daily laborers. Majority (55.4%) of respondent’s family have >1500 ETB monthly income (Table 1). Nearly all 96.7% of participants have latrine near their house, while 83.7% have access to safe water source, and Fifty nine percent of pregnant women have low decision-making autonomy while the rest have high decision-making autonomy (Figure 2).
| Variables | Frequency | Percent | |
|---|---|---|---|
| Religion of respondents | Muslim | 72 | 9.2 |
| Protestant | 505 | 64.7 | |
| Orthodox | 158 | 20.3 | |
| Others | 45 | 5.8 | |
| Marital status of respondents | Single | 12 | 1.5 |
| Married | 762 | 97.7 | |
| Divorced | 6 | 0.8 | |
| Residence | Urban | 414 | 53.1 |
| Rural | 366 | 46.9 | |
| Respondents occupational status | Government employee | 151 | 19.4 |
| Merchant | 118 | 15.1 | |
| House wife | 379 | 48.6 | |
| Daily laborer | 50 | 6.4 | |
| Student | 82 | 10.5 | |
| Couples occupational status | Government employee | 182 | 23.7 |
| Farmer | 253 | 32.9 | |
| Merchant | 134 | 17.4 | |
| Daily laborer | 199 | 25.9 | |
| Age group of respondents | 15-24 | 330 | 42.3 |
| 25-34 | 396 | 50.8 | |
| 35-49 | 54 | 6.9 | |
| Respondents educational status | No formal education | 60 | 7.7 |
| Primary education | 282 | 36.2 | |
| Secondary education | 252 | 32.3 | |
| Tertiary education | 186 | 23.8 | |
| Couples educational status | No formal education | 54 | 7 |
| Primary education | 246 | 32 | |
| Secondary education | 294 | 38.3 | |
| Tertiary education | 174 | 22.7 | |
| Family size of respondent | =3 | 486 | 62.3 |
| 04-Jun | 240 | 30.8 | |
| >6 | 54 | 6.9 | |
| Presence of under five children in the house hold | No | 456 | 58.5 |
| Yes | 324 | 41.5 | |
| Household monthly income | <1000 | 246 | 31.5 |
| 1000-1500 | 102 | 13.1 | |
| >1500 | 432 | 55.4 | |
| Note: Others* 7th day Adventists | |||
Table 1. Socio-demographic characteristics of participants attending Antenatal care services at Public Hospitals of West Wollega Zone, 2020
Reproductive and health care characteristics of the respondents
A mean (± SD of age at first marriage, number of pregnancy, and gestational age of respondents were 19(± 2.14) years, 2 (± 1.16) pregnancy, and 30 (± 5.1) weeks respectively. About three fourth of participants were married at age of 18 years and above. Majority (63.8%) of respondents were at their third trimesters of pregnancy, about two third 68.5 of them were multigravida. Seven hundred and two of respondents (90%) said their current pregnancy was intended. About 78% of respondents were used any type of contraceptive before current pregnancy. One hundred fifty six (20%) of respondents reported history of pregnancy related complication, 8.5% reported history of current illness, and 3.8% reported history of chronic illness, while only 6.3% of them have history of substance use(Table 2).
| Variables | Frequency | Percent | |
|---|---|---|---|
| Age at first marriage of respondents (N=774) | <18 years | 132 | 17.1 |
| = 18 years | 642 | 82.9 | |
| Trimesters of pregnancy | Second | 282 | 36.2 |
| Third | 498 | 63.8 | |
| Number of pregnancy | Prim gravida | 246 | 31.5 |
| Multigravida | 534 | 68.5 | |
| Number of birth (N=528) | Null para | 276 | 52.3 |
| Multipara | 252 | 47.7 | |
| Previous birth interval (N=252) | <2 years | 30 | 11.9 |
| 2 to 4 years | 150 | 59.5 | |
| >= 4 years | 72 | 28.6 | |
| Intention of current pregnancy | No | 78 | 10 |
| Yes | 702 | 90 | |
| Number of antenatal care visit | First visit | 210 | 26.9 |
| Second visit | 216 | 27.7 | |
| Third visit | 210 | 26.9 | |
| Fourth visit | 144 | 18.5 | |
| Previous contraceptive use | No | 174 | 22.3 |
| Yes | 606 | 77.7 | |
| Nutritional advice during pregnancy (N=570) | No | 276 | 48.4 |
| Yes | 294 | 51.6 | |
| Use of iron and folic acid supplementation (N=570) | No | 36 | 6.3 |
| Yes | 534 | 93.7 | |
| Deworming (N=570) | No | 473 | 83 |
| Yes | 97 | 17 | |
| History of pregnancy complication | No | 624 | 80 |
| Yes | 156 | 20 | |
| History of current illness | No | 714 | 91.5 |
| Yes | 66 | 8.5 | |
| History of frequent illness | No | 708 | 90.8 |
| Yes | 72 | 9.2 | |
| History of chronic illness | No | 750 | 96.2 |
| Yes | 30 | 3.8 | |
| Substance use | No | 731 | 93.7 |
| Yes | 49 | 6.3 | |
Table 2. Reproductive and medical characteristics of participants attending Antenatal care services at Public Hospitals of West Wollega Zone, 2020 (N=780)
Dietary characteristics of the respondents
Two hundred and thirty six (30.3%) of participants respond as consuming meals less than three times a day while majority of respondents (62.3%) of them said not increased their meals since pregnancy. Nearly half (49.2%) of pregnant women reported no habit of eating snack. Only 14.6% of participants have habit of fasting, while 18.5% have food avoidance and 8.5% have habit of skipping meal during current pregnancy.
More than three forth (80%) of pregnant women have poor prenatal feeding habit, 40% of them consumed low dietary diversity. From total participants, 600 (76.9%) were from food secure, 10.8% were from mildly food insecure, 5.4% were from moderately food insecure, and 6.9% were from severely food insecure household (Table 3). All most all (97.7%) of the participants adequately consume cereals, more than three forth (80.1%) adequately consume legumes, and more than half (58.3%) adequately consume dark green leafy vegetables. Less than half of respondents adequately consume the rest of food group listed in the table below, except milk and its products, which no participants have adequately consumed during last four weeks before the study (Table 4).
| Variables | Frequency | Percent | |
|---|---|---|---|
| Frequency of meals in a day | <3 | 236 | 30.3 |
| =3 | 544 | 69.7 | |
| Increased frequency of meals | No | 486 | 62.3 |
| Yes | 294 | 37.7 | |
| Habit of eating snack | No | 384 | 49.2 |
| Yes | 396 | 50.8 | |
| Habit of fasting | No | 666 | 85.4 |
| Yes | 114 | 14.6 | |
| Food avoidance | No | 636 | 81.5 |
| Yes | 144 | 18.5 | |
| Habit of skipping meal | No | 714 | 91.5 |
| Yes | 66 | 8.5 | |
| Prenatal feeding habits of respondents | Poor | 630 | 80.8 |
| Good | 150 | 19.2 | |
| Dietary diversity of woman | Low | 312 | 40 |
| High | 468 | 60 | |
| Household food insecurity status | Food secure | 600 | 76.9 |
| Mild | 84 | 10.8 | |
| Moderate | 42 | 5.4 | |
| Severe | 54 | 6.9 | |
Table 3. Prenatal feeding habits of participants attending Antenatal care services at Public Hospitals of West Wollega Zone, 2020
| Variable | Category | Frequency | Percent |
|---|---|---|---|
| Cereals intake | Inadequate | 18 | 2.3 |
| Adequate | 762 | 97.7 | |
| Legumes intake | Inadequate | 155 | 19.9 |
| Adequate | 625 | 80.1 | |
| Dark green leafy vegetables intake | Inadequate | 325 | 41.7 |
| Adequate | 455 | 58.3 | |
| Yellow orange vegetables intake | Inadequate | 522 | 66.9 |
| Adequate | 258 | 33.1 | |
| White roots and tubers intake | Inadequate | 532 | 68.2 |
| Adequate | 248 | 31.8 | |
| Flesh meats intake | Inadequate | 696 | 89.2 |
| Adequate | 84 | 10.8 | |
| Milk and milk products intake | Inadequate | 768 | 98.5 |
| Adequate | 12 | 1.5 | |
| Eggs intake | Inadequate | 672 | 86.2 |
| Adequate | 108 | 13.8 | |
| Oils and fats intake | Inadequate | 522 | 66.9 |
| Adequate | 258 | 33.1 |
Table 4. Consumption of common food groups among participants attending ANC services at Public Hospitals of West Wollega Zone, 2020
Nutritional status of respondents
The mean (± SD) MUAC of pregnant women studied was 24.24 (± 2.7) cm. The magnitude of under nutrition (MUAC <23 cm) was 39.2%, (95%CI: 35.7%, 42.6%) (Figure 3)
Results of logistic regression analysis: Under nutrition was taken as a dependent variable and compared against each independent variable for association. Bivariable logistic regression was done to identify factors associated with nutritional status of pregnant women. Accordingly, household food insecurity, low dietary diversity, poor prenatal feeding habits, number of pregnancy, trimesters of pregnancy, age at first marriage less than 18 years, family size ≥6, substance use, chronic illness, rural residence, not eating snack, not increase frequency of meal shows significant association with under nutrition crudely at 25% (Tables 5-7).
| Associated Factors | Undernutrition (MUAC<23) | P-Value | COR | 95%C.I for COR | |||
|---|---|---|---|---|---|---|---|
| Yes Count (%) | No | Lower | Upper | ||||
| Count (%) | |||||||
| Age group of respondents | 15-24 | 138(41.8) | 192(58.2) | 0.717 | 0.89 | 0.5 | 1.6 |
| 25-34 | 144(36.4) | 252(63.6) | 0.251 | 0.71 | 0.4 | 1.27 | |
| 35-49 | 24(44.4) | 30(55.60) | 1 | ||||
| Respondents residence | rural | 198(54.1) | 168(45.9) | 0 | 3.34 | 2.47 | 4.51* |
| urban | 108(26.1) | 306(73.9) | 1 | ||||
| Household monthly income | <1000 | 112(47.5) | 124(52.5) | 0.263 | 1.29 | 0.79 | 5.25 |
| 1000-1500 | 46(45.1) | 56(54.9) | 0.156 | 1.17 | 0.54 | 3.98 | |
| >1500 | 178(41.2) | 254(58.8) | 1 | ||||
| Family size of respondent | >=6 | 30(55.6) | 24(44.4) | 0.039 | 1.82 | 1.03 | 3.20* |
| 04-May | 78(32.5) | 162(67.5) | 0.032 | 0.7 | 0.51 | 0.97 | |
| <=3 | 198(40.7) | 288(59.3) | 1 | ||||
| Presence of under five children | Yes | 138(42.6) | 186(57.4) | 0.105 | 0.79 | 0.59 | 1.05 |
| No | 168(36.8) | 288(63.2) | 1 | ||||
| Sources of drinking water | Unsafe | 48(80) | 12(20) | 0.479 | 1.15 | 0.78 | 1.68 |
| Safe | 258(35.8) | 462(64.20) | 1 | ||||
| No latrine | Yes | 12(50) | 12(50) | 0.276 | 1.57 | 0.7 | 3.54 |
| No | 294(38.9) | 462(61.1) | 1 | ||||
| Decision making autonomy | Low | 186(40.3) | 276(59.7) | 0.478 | 1.11 | 0.83 | 1.49 |
| High | 120(37.7) | 198(62.3) | 1 | ||||
| Substance use | Yes | 32(65) | 17(34.7) | 0 | 3.14 | 1.71 | 5.76* |
| No | 274(37.5) | 45762.5) | 1 | ||||
| Respondents educational status | No formal education | 66(55) | 54(45) | 0.528 | 1.21 | 0.67 | 2.2 |
| Primary education | 162(52.9) | 144(47.1) | 0.127 | 1.35 | 0.92 | 1.97 | |
| Secondary education | 66(28.9) | 162(71.1) | 0.576 | 1.12 | 0.75 | 1.66 | |
| Tertiary education | 12(9.5) | 114(90.5) | 1 | ||||
| Couples educational status | No formal education | 72(60) | 48(40) | 0.393 | 1.31 | 0.71 | 2.43 |
| Primary education | 108(50) | 108(50) | 0.425 | 0.85 | 0.57 | 1.27 | |
| Secondary education | 9638.1) | 156(61.9) | 0.141 | 1.33 | 0.91 | 1.96 | |
| Tertiary education | 30(16.7) | 150(83.3) | 1 | ||||
| Respondents occupational status | farmer | 66(45.8) | 78(54.2) | 0.258 | 1.33 | 0.81 | 2.17 |
| merchant | 18(25) | 54(75) | 0.867 | 1.03 | 0.7 | 1.53 | |
| house wife | 198(51.6) | 186(48.4) | 0.651 | 1.16 | 0.6 | 2.24 | |
| daily laborer | 18(33.3) | 36(66.7) | 0.099 | 1.58 | 0.92 | 2.73 | |
| government employee | 6(6.7) | 84(93.3) | 1 | ||||
| Couples occupational status | farmer | 192(56.1) | 150(43.9) | 0.094 | 1.4 | 0.94 | 2.06 |
| merchant | 18(15) | 102(85) | 0.551 | 1.15 | 0.73 | 1.82 | |
| daily laborer | 72(52.2) | 66(47.8) | 0.774 | 1.06 | 0.7 | 1.61 | |
| government employee | 24(14.8) | 138(85.2) | 1 | ||||
| Note: * = statistically significant at p-value < 0.25, 1: reference category, COR: Crude Odds Ratio, 95%CI: 95 percent confidence interval | |||||||
Table 5. Bivariate analysis of Socio demographic factors associated with undernutrition among pregnant women attending ANC at West Wollega public Hospitals, 2020
| Associated Factors | Undernutrition (MUAC<23) | P-Value | COR | 95% CI for COR | |||
|---|---|---|---|---|---|---|---|
| Yes, Count (%) | No. Count (%) | Lower | Upper | ||||
| Number of pregnancy | multigravida | 228(42.7) | 306(57.3) | 0.004 | 1.61 | 1.17 | 2.21* |
| prim gravida | 78(31.7) | 168(68.3) | 1 | ||||
| Trimesters of pregnancy | 3rd trimester | 174(34.9) | 324(65.1) | 0.001 | 0.61 | 0.45 | 0.82* |
| 2nd trimester | 132(46.8) | 150(53.2) | 1 | ||||
| Age at first marriage | <18 years | 96(72.7) | 36(27.3) | 0 | 5.49 | 3.62 | 8.32* |
| >=18 years | 210(32.7) | 432(67.3) | 1 | ||||
| History of illness in current pregnancy | Yes | 30(45.5) | 36(54.5) | 0.28 | 1.32 | 0.8 | 2.2 |
| No | 276(38.7) | 438(61.3) | 1 | ||||
| History of chronic illness | Yes | 18(60) | 12(40) | 0.021 | 2.41 | 1.14 | 5.06* |
| No | 288(38.4) | 262(61.6) | 1 | ||||
| History of pregnancy complication | Yes | 60(38.5) | 96(61.5) | 0.826 | 0.96 | 0.67 | 1.38 |
| No | 246(39.40) | 378(60.60) | 1 | ||||
| No previous contraceptive use | Yes | 72(41.40) | 102(58.60) | 0.51 | 1.12 | 0.8 | 1.58 |
| No | 234(38.60) | 372(61.40) | 1 | ||||
| Number of antenatal care visit | first visit | 84(40) | 126(60) | 0.276 | 0.79 | 0.51 | 1.21 |
| second visit | 66(30.60) | 150(69.4) | 0.003 | 0.52 | 0.34 | 0.81 | |
| third visit | 90(42.9) | 120(57.1) | 0.58 | 0.89 | 0.58 | 1.36 | |
| fourth visit | 66(45.8) | 78(54.2) | 1 | ||||
| Non intended pregnancy | Yes | 36(46.2) | 42(53,8) | 0.188 | 1.37 | 0.86 | 2.2 |
| No | 270(38.5) | 432(61.5) | 1 | ||||
| Note: * = statistically significant at p-value <0.25, 1: reference category, COR: Crude Odds Ratio, 95%CI: 95 percent confidence interval | |||||||
Table 6. Bivariate analysis of Reproductive and medical factors associated with undernutrition among participants attending ANC services at West Wollega public Hospitals, 2020
| Associated Factors | Undernutrition (MUAC<23) | P-Value | COR | 95% CI for COR | |||
|---|---|---|---|---|---|---|---|
| Yes, Count (%) | No, Count (%) | Lower | Upper | ||||
| Less than three meals in a day | Yes | 95(40.3) | 141(59.7) | 0.7 | 1.06 | 0.78 | 1.45 |
| No | 211(38.8) | 333(61.2) | 1 | ||||
| No habit of eating snack | Yes | 186(48.4) | 198(51.6) | 0 | 2.16 | 1.61 | 2.89* |
| No | 120(30.3) | 276(69.7) | 1 | ||||
| Not increased frequency of meals | Yes | 240(49.4) | 246(50.6) | 0 | 3.37 | 2.43 | 4.67* |
| No | 66(22.4) | 228(77.6) | 1 | ||||
| Food avoidance during pregnancy | Yes | 54(37.5) | 90(62.5) | 0.638 | 0.91 | 0.63 | 1.33 |
| No | 252(39.60) | 384(60.4) | 1 | ||||
| Habit of fasting while pregnant | Yes | 54(47.4) | 60(52.6) | 0.055 | 1.48 | 0.99 | 2.2 |
| No | 252(37.8) | 414(62.2) | 1 | ||||
| Habit of skipping meal | Yes | 54(81.8) | 12(18.2) | 0 | 8.25 | 4.33 | 15.71* |
| No | 252(35.3) | 462(64.7) | 1 | ||||
| Prenatal feeding habits | Poor | 187(29.7) | 443(70.3) | 0.236 | 0.84 | 0.25 | 1.67 |
| Good | 50(33.3) | 150(66.7) | 1 | ||||
| Household food insecurity status | Severe | 42(77.9) | 12(22.2) | 0 | 8.57 | 4.41 | 16.67* |
| Moderate | 30(71.4) | 12(28.8) | 0 | 6.12 | 3.06 | 12.23* | |
| Mild | 60(71.4) | 24(28.6) | 0 | 6.12 | 3.69 | 10.14* | |
| Food secure | 174(29) | 426(71) | 1 | ||||
| Dietary diversity of woman | Low | 222(71.2) | 90(28.8) | 0 | 11.28 | 8.03 | 15.84* |
| High | 84(17.9) | 384(82.0) | 1 | ||||
| Dark green leafy vegetables intake | inadequate | 121(37.2) | 204(62.8) | 0.334 | 0.87 | 0.65 | 1.16 |
| adequate | 185(40.7) | 270(59.3) | 1 | ||||
| Yellow orange vegetables intake | inadequate | 216(41.4) | 306(58.6) | 0.081 | 1.32 | 0.97 | 1.8 |
| adequate | 90(34.9) | 168(65.1) | 1 | ||||
| White roots and tubers intake | inadequate | 207(38.9) | 325(61.1) | 0.788 | 0.96 | 0.7 | 1.31 |
| adequate | 99(39.9) | 149(60.1) | 1 | ||||
| Flesh meats intake | inadequate | 270(38.8) | 426(61.2) | 0.472 | 0.85 | 0.53 | 1.34 |
| adequate | 36(42.9) | 48(57.1) | 1 | ||||
| Eggs intake | inadequate | 265(39.4) | 407(60.6) | 0.771 | 1.06 | 0.7 | 1.62 |
| adequate | 41(38) | 67(62.0) | 1 | ||||
| Oils and fats intake | inadequate | 202(38.7) | 320(61.3) | 0.664 | 0.94 | 0.69 | 1.27 |
| adequate | 104(40.3) | 154(59.7) | 1 | ||||
| Note: * = statistically significant at p-value <0.25, 1: reference category, COR: Crude Odds Ratio, 95%CI: 95 percent confidence interval | |||||||
Table 7. Bivariate analysis of dietary factors with nutritional status of pregnant women attending antenatal care clinics in public hospitals of west Wollega Zone, 2020
Variables associated with adjusted analysis: pregnant women, accordingly, household food insecurity, low dietary diversity, substance use and residence were identified as independent predictors of under nutrition among pregnant women.
The odds of under nutrition were four times [AOR=4.36, 95% CI: (2.36, 8.79)] more among mildly food insecure household, and nearly four times [AOR=3.71, 95% CI: 1.54, 8.61), among moderately food insecure households, and six times [AOR=6.96, 95% CI: (3.15,15.42)] among severely food insecure household) compared with their food secure counterparts. Pregnant women with low dietary diversity had seven times [AOR=7.56, 95% CI :( 4.96, 11.51)] increased odds of under nutrition than those with high dietary diversity status.
Moreover, the odds of under nutrition was three times [AOR=3.33, 95% CI: 1.63, 6.81)] among substance users -than their counter- parts. Rural pregnant women had nearly three times [AOR=2.68, 95%CI: 1.77, 4.06)] increased odds of under nutrition than urban women (Table 8).
| Associated factors | Undernutrition(MUAC<23cm) | Bivariate analysis | Multivariable analysis | ||||||
|---|---|---|---|---|---|---|---|---|---|
| COR | 95% C.I COR | AOR | 95% C.I AOR | ||||||
| Yes | No | Lower | Upper | Lower | Upper | ||||
| Household food insecurity status | Severe | 42(77.9%) | 12(22.2%) | 8.57 | 4.41 | 16.67 | 6.96 | 3.15 | 15.42** |
| Moderate | 30(71.4%) | 12(28.8%) | 6.12 | 3.06 | 12.23 | 3.71 | 1.54 | 8.96** | |
| Mildly | 60(71.4%) | 24(28.6%) | 6.12 | 3.69 | 10.14 | 4.55 | 2.36 | 8.79** | |
| Food secure | 174(29%) | 426(71%) | 1 | 1 | |||||
| Dietary diversity of woman | Low | 222(71.2%) | 90(28.8%) | 11.28 | 8.03 | 15.85 | 7.56 | 4.96 | 11.51** |
| High | 84(17.9%) | (384)82.0% | 1 | 1 | |||||
| Prenatal feeding habits | Poor | 343(54.4%) | 287(45.6%) | 5.77 | 3.48 | 9.57 | 1.81 | 0.86 | 3.83 |
| Good | 131(87.3%) | 19(12.7%) | 1 | 1 | |||||
| Number of pregnancy | Multigravida | 228(42.7%) | 306(57.3%) | 1.61 | 1.17 | 2.21 | 0.98 | 0.6 | 1.6 |
| Prim gravida | 78(31.7%) | 168(68.3%) | 1 | 1 | |||||
| Trimesters of pregnancy | Third trimester | 174(34.9%) | 324(65.1%) | 0.61 | 0.45 | 0.82 | 0.78 | 0.52 | 1.17 |
| Second trimester | 132(46.8%) | 150(53.2%) | 1 | 1 | |||||
| Age at first marriage | < 18 years | 96(72.7%) | 36(27.3%) | 5.49 | 3.62 | 8.32 | 1.62 | 0.93 | 2.82 |
| >= 18 years | 210(32.7%) | 432(67.3%) | 1 | 1 | |||||
| Family size | >=6 | 30(55.6%) | 24(44.4%) | 1.82 | 1.03 | 3.2 | 0.47 | 0.22 | 1 |
| 4_5 | 78(32.5%) | 162(67.5%) | 0.7 | 0.51 | 0.97 | 0.77 | 0.48 | 1.23 | |
| <=3 | 198(40.7%) | 288(59.3%) | 1 | 1 | |||||
| Substance use | Yes | 32(65%) | 17(34.7%) | 3.14 | 1.71 | 5.76 | 3.33 | 1.62 | 6.81** |
| No | 274(37.5%) | 457(62.5%) | 1 | 1 | |||||
| History of chronic illness | Yes | 18(60%) | 12(40%) | 2.41 | 1.14 | 5.07 | 2.83 | 0.98 | 8.12 |
| No | 288(38.4%) | 262(61.6%) | 1 | 1 | |||||
| Respondents residence | Rural | 198(54.1%) | 168(45.9%) | 3.34 | 2.47 | 4.51 | 2.68 | 1.77 | 4.06** |
| Urban | 108(26.1%) | 306(73.9%) | 1 | 1 | |||||
| No habit of eating snack | Yes | 186(48.4%) | 198(51.6%) | 2.16 | 1.61 | 2.9 | 1.07 | 0.67 | 1.69 |
| No | 120(30.3%) | 276(69.7%) | 1 | 1 | |||||
| Not increased frequency of meals | Yes | 240(49.4%) | 246(50.6%) | 3.37 | 2.43 | 4.67 | 1.21 | 0.7 | 2.07 |
| No | 66(22.4%) | 228(77.6%) | 1 | 1 | |||||
| Note: ** indicates statistically significant at P-value<0.05, 1 indicates reference, COR=Crude Odd Ratio, AOR=Adjusted Odd Ratio | |||||||||
Table 8. Multivariate analysis of factors associated with under nutrition among pregnant women attending ANC services at public hospitals of west Wollega Zone
Discussion
The current study tried to reveal the magnitude and factors associated with undernutrition among pregnant women in West Wollega Zone, Western part of Ethiopia. Accordingly, nearly forty percent (39.2%) of participants were undernourished and factors associated with their nutritional status were residency, substance use, household food insecurity and low dietary diversity of women.
The global estimate of maternal malnutrition during pregnancy appears to be decreasing in almost all regions of the globe except in Africa where the number of pregnant mothers with malnutrition has been increasing steadily over time, this shows that the result of this study is relevance to the current status of undernutrition in Africa, and Ethiopia in particular[14]. The finding of this study was almost consistent with the study conducted in the South western part of our country which shows 44.9% [24] and study conducted in Southern part of Ethiopia which was 35.5% [27].
On the other hand, this study result was lower than study done in Kunama population, Tigray, northern Ethiopia, which was observed to be 47.9%, this may be due to that in the above study the proportion of Food insecurity is higher than the present study which could increase the risk of undernutrition [28]. But lower prevalence of undernutrition was reported among studies conducted in Gambella Town (28.6%), Alamata General Hospital (23.2%), rural communities in Haramaya district (19.06%), and Dessie town (19.5%) [17,18,21,29]. The discrepancies between the findings may be due to geographical variation between the studies or due to the variation in the cut off point for MUAC measurement that the studies above uses lower cut off points than the present study, which could under estimate the prevalence of undernutrition.
According to this study, rural residents were three times more likely to have undernutrition than urban ones. It is true that place of residence usually determines people’s life-styles, income, and most notably their health conditions and nutrition [30]. This finding is in line with the finding of systematic review done in Africa, the study done in University of Gondor Hospital, and the study done in Boricha Woreda, Sidama Zone which indicates rural pregnant women were more likely to develop undernutrition than urban ones (13,21,50). But this finding may not be true in developed world, in that one study in USA shows there is no significant association between nutritional status and residency [31].
Another factor that shows independent prediction with under nutrition in this study was substance use. Accordingly, pregnant women who were using substance show three times more risk of undernutrition than those who were not using substance. Women with substance use disorders frequently experience inadequate prenatal care, chronic medical problems, poverty, and domestic violence that may increase vulnerability to poor nutrition [32]. The finding of study in South Western Ethiopia similarly shows that women with history of substance use were two times more at risk of under nutrition than who were not using any substance [24]. Study done in Rural Eastern Ethiopia also reported the risk of undernutrition is 29% more among substance users [31].
In this study, pregnant women who were consuming low dietary diversity were more than seven times more likely be undernourished than those who were consuming high dietary diversity. The finding of this study is consistent with the study done in Dessie town which shows women who had low dietary diversity were nearly six times more likely to contract undernutrition than the other ones [17]. The study done in Gambella town also shows that pregnant women who had low dietary diversity score were two times more at risk of undernutrition than their counter ones [23]. Survey done in Iran, and a study conducted in Kenya were also among other studies that shows similar finding with this study [33,34]. In contrast to this study, dietary diversity was not show any significant correlation with maternal anthropometry in rural Cambodia this may be due to that very proportion of women shows prevalence of low dietary diversity in the study done in rural Cambodia [35].
In this study, respondents who were from food insecure household shows more at risk of malnutrition than those from food secure households. Our finding of an increased prevalence of maternal undernutrition in food insecure households may reflect inequitable intra-household food allocation whereby the nutritional needs of the child and/or other members of the household are prioritized over those of the mother. As evidenced from 2019 FAO food insecurity report that, household food insecurity was found to be associated with more than one form of malnutrition [30]. Similar finding was reported from study done in Gumay district, study conducted in Gambella Town, and study done in Kunama population in Tigray region [23,24, 28]. Study done in Nepal also indicates significant relationship between food adequacy and low nutritional status of pregnant women [36]. In contrast to this, increased maternal anthropometry was observed among women from mildly food insecure households in USA, Brazil and Lebanon, this discrepancy may be due to that these studies were from developed world with different sociodemographic characteristics, and they have different method of assessment when compared to present study [37-39].
Educational status of respondents does not show significant association with under nutrition in current study. But this finding contradicts the finding of the study done in Shashamene district, southern part of Ethiopia which shows literate women were 70% reduction in risk of undernutrition than those who had no formal education [40]. Study done in University of Gondor Hospital also shows the risk of undernutrition was nearly three times among pregnant women with no formal education [22]. The study done in rural Nepal also reported there was a significant relationship between the educational level of the women and the general nutritional status [34]. The reason might be because; food and related factors that have an effect on nutritional status of women are under the control of the household head, even though the women had higher education.
Limitations of the study
? Even though this study tried to cover several variables, it does not include variables that need laboratory investigations such as intestinal parasites, and malaria infection.
? Dietary intake of respondents was measured only on occasional time, and that may not show the seasonal variability on availability of food.
? This study used anthropometric measure to assess nutritional status of pregnant mothers and the effect of technical error was not ruled out that may affect the reliability of result.
? As it is institutional based study, the finding of this study does not fully indicate the characteristics of respondents at community level which means it is not generalized beyond study population.
Conclusion
This study revealed that, nearly forty percent of pregnant women were undernourished showing high prevalence that needs priority attention intervention. The factors that significantly associated with undernutrition were respondent’s residency, substance use, low dietary diversity, and household food insecurity status. The remaining factors studied were not showing any significant association with undernutrition..
Recommendations
Based on the finding of this study the following recommendations were forwarded.
? Governments should adopt coherent policies, which foster cross-sectoral cooperation and strategies to avert the problem of undernutrition among pregnant women.
? Policy makers and implementers should make programs that improve food security status at household level to increase access to high nutritious food and variety of foods among poor.
? Essential investments must be made into nutritionsensitive programme in other areas such as agriculture, education, water and social protection.
? Agricultural sector should implement nutrition sensitive interventions such as increased productivity and dietary diversifications.
? Health workers should disseminate useful information about the harmful effect of using substance during pregnancy at health institution and community level in order to improve the dietary habits of pregnant women especially for rural residents.
? Health workers should also advice pregnant women about the benefits of dietary diversity during pregnancy.
Acknowledgement
We are grateful to officials from Zonal health office and public Hospitals of West Wollega zone, and the health workers of each facility for their valuable contribution during the study. We also extend our thanks to data collectors, respondents, and supervisors for their cooperation during the study.
Declaration
Ethics approval and consent to participate
The study protocol was approved and permission was obtained from Wollega University. An official letter of co-operation was written to the selected Public Hospitals of West Wollega Zone Administration. Information on the studies, including purpose and procedures was given for participants. Written or verbal consent was obtained from each participant. In order to protect confidentiality, names or identifications were not included on the written questionnaires. Identification of the respondents was only through numerical codes.
Consent for publication
'Not applicable'
Availability of data and materials
The finding of this study was generated from the data collected and analyzed based on stated methods and materials. The original data supporting this finding are available from the corresponding author on reasonable request.
Competing interests
"The authors declare that they have no competing interests"
Funding
'Not applicable'
Authors' contributions
LT participated in the design of the study, performed the data collection and the statistical analysis and served as the corresponding author of the manuscript. HB, IF, ZK and MD supervised the study, ensured quality of the data, assisted in the analysis and interpretation of the data. All authors read and approved the manuscript.
References
- Von Grebmer J, Bernstein R, Mukerji F, et al. 2019 Global hunger index: The challenge of Hunger and climate change. 2019.
- Development Initiatives. Global Nutrition Report 2018: Shining a light to spur action on nutrition. Bristol, UK. 2018.
- Salem S, Eshra D SN. Effect of malnutrition during pregnancy on pregnancy outcomes. 18th Int Conf Nurs Heal care. 2016;5(10):4172.
- Tang AM, Chung M, Dong K, et al. Determining a Global Mid-Upper Arm Circumference Cutoff to Assess Malnutrition in Pregnant Women. FANTA. 2016.
- Black RE, Allen LH, Bhutta ZA, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371(9608):243-60.
- Gopalan C. Effect of nutrition on pregnancy and lactation. Bull World Health Organ. 1962;26(2):203-11.
- Union A. The cost of hunger in Africa: Social and economic impact of child undernutrition in Egypt, Ethiopia, Swaziland and Uganda background paper. Abuja, Nigeria. 2014 Mar.
- Blössner M, Onis M De, Prüss-üstün A, et al. Malnutrition Quantifying the health impact at national and local levels. World Heal Organ. 2005;(12):1-51.
- Black RE, Victora CG, Walker SP, et al. Maternal and child under nutrition and overweight in low-income and middle-income countries. Lancet. 2013;382(9890):427-51.
- Adebowale SA, Adepoju OT, Okareh OT FF. Social epidemiology of Adverse nutritional Outcome among women in nigeria. Pakista J Nutr. 2011;10(9):888-98.
- Lartey A. Maternal and child nutrition in Sub-Saharan Africa : challenges and interventions. Proc Nutr Soc. 2020;67(2008):105-08.
- Ravishankar AK, Ramachandran S SA. Prevalence of chronic energy deficiency and its consequence on children’s nutritional status among the marginalized group in India. 2013;43-4.
- Devgun P, Mahajan SL, Gill KP. Prevalence of chronic energy deficiency and socio demographic profile of women in slums of Amritsar city, Punjab, India. Int J Res in Health Sci. 2014;2(2):527-32.
- Demelash DH, Dadi AF. Burden and determinants of malnutrition among pregnant women in Africa : A systematic review and meta-analysis.PLoS One. 2019;14(9): e0221712.
- World Health Organization. Nutrition in the WHO African Region. Brazzaville: World Health Organization. 2017:1-85.
- Workicho A, Kolsteren P, Belachew T. Burden and determinants of undernutrition among young pregnant women in Ethiopia. Matern Child Nutr. 2018:15(3):1-9.
- Diddana TZ. Factors associated with dietary practice and nutritional status of pregnant women in Dessie town , northeastern Ethiopia : a community-based cross-sectional study. BMC Pregnancy Childbirth. 2019;19:1-10.
- Kedir H, Berhane Y, Worku A. Magnitude and determinants of malnutrition among pregnant women in eastern Ethiopia : evidence from rural , community-based setting. Matern Child Nutr. 2016;12:51-63.
- Kuche D, Singh P, Moges D, et al. Nutritional Status and Associated Factors among Pregnant Women in Wondo Genet District, Southern Ethiopia. J Food Sci Eng. 2015;5:85-94.
- Dadi AF DH. Undernutrition and its associated factors among pregnant mothers in Gondar town, Northwest Ethiopia. PLoS One. 2019;14(4):e0215305.
- Endalifer M, Tewabe M, Adar A et al. Undernutrition and associated factors among pregnant women attending ANC follow up in Alamata general hospital, Northern Region, Ethiopia, 2017. J Nutr Health Food Eng. 2019;9(3):70-8.
- Kumera G, Gedle D, Alebel A, et al. Undernutrition and its association with socio-demographic , anemia and intestinal parasitic infection among pregnant women attending antenatal care at the University of Gondar Hospital , Northwest Ethiopia. Matern health, Neonatol Perinatol. 2018;4:1-10.
- Gebrehiwot TT, Gemeda DH, Nigatu M. Household Food Insecurity , Low Dietary Diversity , and Early Marriage Were Predictors for Undernutrition among Pregnant Women Residing in Gambella , Ethiopia. Hindawi. 2018;2018:10.
- Shiferaw A H. Acute Under Nutrition and Associated Factors among Pregnant Women in Gumay District, Jimma Zone, South West Ethiopia. J Women ’ s Heal Care. 2019;8(2):1-12.
- Forouzanfar MH, Alexander L, Anderson HR, et al. Global , regional , and national comparative risk assessment of 79 behavioural , environmental and occupational , and metabolic risks or clusters of risks in 188 countries , 1990 – 2013 : a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386(10010):2287-323.
- WHO. Nutrition of women in the preconception period, during pregnancy and the breastfeeding period. New york; 2011.
- Mathewos M. Eskindir L. Nutritional status and associated factors among pregnant women in Boricha Woreda, Sidama Zone, Southern Ethiopia, 2013: Institute. Hawassa Univ Coll Med Heal Sci Amare Werku Addis Cont. 2013.
- Abraham S, Miruts G, Shumye A. Magnitude of chronic energy deficiency and its associated factors among women of reproductive age in the Kunama population. BMC Nutr. 2015;1(12):1-9.
- Tafese Z, Kebebu A. A systematic review of maternal feeding practice and its outcome in developing countries. Res J Food Sci Nutr. 2017;2:9-14.
- FAO, IFAD, UNICEF. Food security and nutrition in the world. safeguarding against economic slowdowns and downturns. 2019. 1-212.
- Hill JL, You W, Zoellner JM. Disparities in obesity among rural and urban residents in a health disparate region. BMC Public Health. 2014;14(1051):1-8.
- Forray A. Substance use during pregnancy open peer review. F1000research Rev. 2016;5:887.
- Vakili M, Abedi P, Sharifi M, et al. Dietary diversity and its related factors among adolescents : A survey in Ahvaz-Iran. Glob J Health Sci. 2013;5(2):181-86.
- Lillian M. Dietary diversity and nutritional status of pregnant women Aged 15-49 years attending kapenguria district hospital west pokot county. Kenya. 2013;1:49.
- Mcdonald CM, Mclean J, Kroeun H, et al. Household food insecurity and dietary diversity as correlates of maternal and child undernutrition in rural Cambodia. Eur J Clin Nutr. 2015;69(2):242-46. Available from:
- Acharya SR, Bhatta J, Timilsina DP. Factors associated with nutritional status of women of reproductive age group in rural , Nepal. Asian Pacific J Heal Sci. 2017;4(4):19-24.
- Jomaa L, Naja F, Cheaib R, et al. Household food insecurity is associated with a higher burden of obesity and risk of dietary inadequacies among mothers in Beirut, Lebanon. BMC Public Health. 2017;17(567):1-14.
- Peterson K, Peterson K. Household food insecurity and obesity risk in an urban slum in Brazil.Public Health Theses. 2014;1-47.
- Olson CM. Symposium : advances in measuring food insecurity and hunger in the US. J Nutr. 1999;129(2):504S-05S.
- Belete Y, Negga B, Firehiwot M. Under Nutrition and Associated Factors among Adolescent Pregnant women in shashemenne district, west arsi zone, Ethiopia : A Community- based Study. J Nutr Food Sci. 2016;6(1):1-7.
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref