Research Article - Current Pediatric Research (2024) Volume 28, Issue 1
The practice of effective breastfeeding technique and its associated factors among lactating mothers visiting Jimma university medical center, Southwest Ethiopia.
Tilahun Wodaynew1, Abebe Merchaw1, Wondwosen Molla2, Aynalem Yetwale3*
1Department of Nursing, Institute of Health, Woldia University, Woldia, Ethiopia
2Department of Midwifery, Institute of Health Dilla University, Dilla, Ethiopia
3Department of Midwifery, Institute of Health, Woldia University, Woldia, Ethiopia
- Corresponding Author:
- Aynalem Yetwale
Department of Midwifery, Institute of Health, Woldia University, Woldia, Ethiopia
E-mail: aynalemyetwale@gmail.com
Received: 25 December, 2023, Manuscript No. AAJCP-24-123406; Editor assigned: 27 December, 2023, Pre QC No. AAJCP-24-123406 (PQ); Reviewed: 10 January, 2024, QC No. AAJCP-24-123406; Revised: 17 January, 2024, Manuscript No. AAJCP-24-123406 (R); Published: 24 January, 2024, DOI:10.35841/0971-9032.28.01.1185-1189.
Abstract
Background: The practice of good positioning and attachment during lactation plays a great role in the practice of exclusive breast feeding. Yet, there is a scarcity of evidence concerning breast feeding techniques in sub-saharan Africa including Ethiopia. Hence, this study was conducted to assess the practice of attachment and positioning during lactation and its associated factors among lactating mothers visiting Jimma university medical center.
Methods: An institutional-based cross-sectional study was conducted on 415 lactating mothers from December 15, 2020, to January 15, 2021. Study participants were selected by using a systematic sampling technique. Data were collected by using a pre-tested interviewer-administered questionnaire and observational checklist. Multiple logistic regression analyses were performed to identify independent predictors, and the strength of association was evaluated by using an odds ratio at 95% confidence interval and a P-value<0.05 was considered to declare significant associations.
Results: In this study, the overall proportion of effective lactation technique was 39.3%. Primipara (AOR; 0.37; 95% CI (0.18-0.77)). Unmarried marital status (AOR; 0.61; 95% CI (0.379-0.99)). Receiving immediate breastfeeding techniques counseling (AOR; 0.318 95% CI (0.19-0.51)) were association with the practice of effective breastfeeding technique.
Conclusions: The overall practice of effective attachment, suckling and positioning during lactation in this study was very low compared to the world health organization recommendation. Marital status, parity and breastfeeding technique counseling immediately after delivery were significant factors associated with the practice of effective lactation technique. Hence, each mother should be counselled and observed for the mother’s and infant’s positioning and effective suckling at the onset of breastfeeding before discharge. Besides, special emphasis should be placed on primipara and unmarried mothers to improve the practice of effective breast feeding technique.
Keywords
Breastfeeding technique, Lactating mothers, Ethiopia.
Introduction
Breastfeeding mothers need to practice effective breastfeeding technique in order to achieve successful and fruitful lactation [1]. Effective breastfeeding techniques are a combination of correct positioning of mother and baby, proper attachment of the baby to the breast, and sucking during breastfeeding [2]. According to the recommendations of the World Health Organization (WHO), good practices are important to promote exclusive breastfeeding [3].
Inadequate breastfeeding technique can lead to breast problems like cracked nipples, mastitis, and breast abscess and is also the cause of early breastfeeding cessation. Moreover, the practice of poor breastfeeding technique leads to stunting, poor weight gain and decreased immunity during childhood [4,5]. The World Health Organization and baby-friendly initiative designed a counseling and demonstration program for effective lactation technique for the mothers during perinatal period.
The integrated management of neonate and childhood illness guidelines supported that the organized assessment of lactation technique and counseling of the women on appropriate positioning and attachment of infants to the breast are needed for effective breastfeeding technique. Despite the practice of effective suckling, positioning and attachment during lactation having a confirmed benefit for the baby and women, its practice is disappointing in African countries including Ethiopia [6]. Several studies conducted on the prevalence and factors associated with exclusive breastfeeding, but the issue of effective breastfeeding technique practice is not get adequate attention and there is a shortage of evidence in the study area. Hence, this study was conducted to assess the practice effective suckling, attachment and positioning during lactation and its associated factors among lactating mothers visiting Jimma university medical center.
Materials and Methods
Study area, peried and study design
An institutional-based cross-sectional study design was conducted at Jimma university medical centre. Geographically, it is located in the city of Jimma, 352 km Southwest of Addis Ababa. Currently, the hospital has 800 beds and is expected to provide health services for more than 20 million people living in the south-western part of Ethiopia and as well as services for South Sudan and neighbouring countries. In addition, the hospital serves as a teaching, health, and research center. This study was from December 15, 2020, to January 15, 2021.
Population
All breastfeeding mother-infant pairs attending the postnatal and expanded program of immunization units in Jimma university medical center were considered as a source population, whereas all selected lactating mother-infant pairs of immediate postpartum mothers whose neonates were alive and mothers came for postnatal care visits and mothers came for immunization service at the EPI unit were considered as the study population. However, the study, mothers with seriously ill infants and neonates with cleft lip and cleft palate were excluded.
Sample size determination and sampling procedure
For this study, the following assumptions: A 95% confidence level, a 5% margin of error, a 10% non-response and the proportion of effective breastfeeding techniques was 43.4% in Hariri city, Eastern Ethiopia were considered to calculate the sample size, and then the sample size was 415 [7]. The average number of immediate postpartum mothers whose neonates were alive and who came for postnatal care visits and immunization units in Jimma university medical center in the last two months were first identified from the client registration book to select the required sample. Study participants were selected by using a systematic sampling technique.
Study variables
Dependent variables: The practice of effective breastfeeding technique.
Independent variables: Socio-demographic variables (age, religion, ethnicity, marital status, educational status, place of residence, women’s occupation, husband educational status).
Obstetric factors (parity, previous place of delivery, gestational age at first ANC visit, number of ANC visit completed, PNC visits, counseling on breastfeeding during ANC, and immediately after delivery).
Operational definition
Breast feeding technique: The composite of attachment, positioning, and suckling during breastfeeding.
Effective breastfeeding technique: In this study effective breast feeding technique is the combination of at least 3 criteria from attachment, 2 criteria from positioning, and 2 criteria from suckling [8].
Data collection tools and procedures
A pretested and semi-structured interviewer-administered questionnaire and a world health organization observation checklist in both Afan Oromo and Amharic languages. The questionnaire was first developed in English, which was modified and adapted from previous studies [9] by reviewing various studies and translated into both the Amharic language and Afan Oromo as per the mother tongue of the participants. The questionnaire was then back-translated into English to check for consistency. Data collection and supervision were performed by six and two BSc midwifery professionals from other health facilities, respectively. Daily meetings were conducted between data collectors, supervisors, and principal investigators to discuss emerging issues and evaluate the progress of the study.
Data quality control/management
To assure the quality of the tool, a pre-test was done on the observational checklist and the questionnaire on a 5% of the sample size at Agaro hospital two weeks before data collection. Subsequently, the tools were modified as required. The collected questionnaires were then checked for completeness.
Data processing and analysis
The consistency and completeness of the collected data were checked and entered by using Epi-data version 3.1 and then exported to the Statistical Package for Social Sciences (SPSS) version 23 software for further analysis. A descriptive statistical analysis was performed and presented as tables, and figures. To assess the association between explanatory variables and outcome variables, bi-variable and multivariable logistic regression analysis were conducted, and independent variables with p-values ≤ 0.25 in the bivariate analysis were considered as a candidate for multivariable logistic regression analysis. The strength of association was evaluated using odds ratio at 95% confidence interval and P-value<0.05 was considered to declare significant associations.
Ethical consideration
Ethical clearance letter was obtained from Jimma university institutional review board and official letter of cooperation obtained from the Jimma university medical center. Informed consent was obtained from each participant before the interviews. The participants informed about the purpose of the study and that all information obtained from the study participants would be kept strictly confidential.
Results
Socio-demographic characteristics of the study participants
Among 415 study participants, 405 were interviewed and observed for breastfeeding technique from postpartum and an EPI unit which gives a response rate of 97.6%. More than half (51.1%) of study participants were found in the age group between 20–30 years. 175 (43.2%) of the participants were Muslim religious followers, and most of the respondents were housewives (35.1%) (Table 1).
| Variable | Category | Frequency | Percent |
|---|---|---|---|
| Age | <20 | 64 | 15.8 |
| 20-30 | 207 | 51.1 | |
| >30 | 134 | 33.1 | |
| Religion | Muslim | 175 | 43.2 |
| Orthodox | 133 | 32.8 | |
| Protestant | 77 | 19 | |
| Catholic | 12 | 3 | |
| Adventist | 8 | 2 | |
| Ethnicity | Oromo | 185 | 45.7 |
| Amhara | 99 | 24.4 | |
| Keffa | 55 | 13.6 | |
| Wolaita | 41 | 10.1 | |
| Tigre | 15 | 3.7 | |
| Others | 10 | 2.5 | |
| Marital status | Unmarried | 54 | 13.3 |
| Married | 351 | 86.7 | |
| Occupation of the mother | Housewife | 142 | 35.1 |
| Government employee | 105 | 25.9 | |
| Nongovernmental employee | 54 | 13.3 | |
| Private business | 70 | 17.3 | |
| Student | 19 | 4.7 | |
| Farmer | 15 | 3.7 | |
| Maternal education status | Don’t educated | 47 | 11.6 |
| Read and write | 51 | 12.6 | |
| Primary education | 112 | 27.7 | |
| Secondary education | 88 | 21.7 | |
| Above secondary | 107 | 26.4 |
Table 1. Socio-demographic characteristics of lactating mothers visiting in Jimma university medical center Jimma Southwest Ethiopia, 2020.
Infant-related characteristics
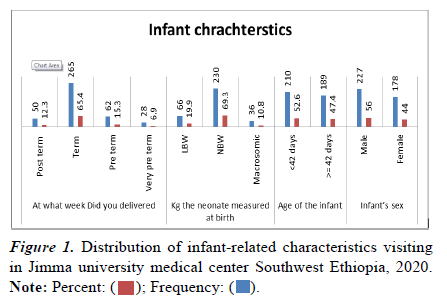
More than half of the infants (52.6%) age were less than 42 weeks, and 56% of them were male by sex. The majority of the infants 265 (65.4%) were delivered at term and approximately 69.3% of the infants had normal birth weight Figure 1.
Maternal health care service utilization related characteristics
More than half study participants (54.6%) were multiparous and had received information about BFT (77.8%) during antenatal care. More than half (56.8%) had previous experience of breastfeeding and majority of participants (64%) had antenatal counseling about breastfeeding, and 61% of them received immediate BFT counselling after delivery in Table 2.
| Variable | Category | Frequency | Percent |
|---|---|---|---|
| Parity | Primipara | 184 | 45.4 |
| Multipara | 221 | 54.6 | |
| Received information about breastfeeding | Yes | 315 | 77.8 |
| No | 90 | 22.2 | |
| Antenatal care counselling about BFT | Yes | 259 | 64 |
| No | 146 | 36 | |
| Get immediate BFT counselling after delivery | Yes | 247 | 61 |
| No | 158 | 39 | |
| Previous experience of breast feeding | Yes | 230 | 56.8 |
| No | 175 | 43.2 | |
| Was this pregnancy planned? | Yes | 277 | 68.4 |
| No | 128 | 31.6 | |
| Where did you attend ANC | Health post | 42 | 10.4 |
| Health center | 285 | 70.4 | |
| Hospital | 78 | 19.3 | |
| Number of ANC visit received | Once | 21 | 5.2 |
| Twice | 106 | 26.2 | |
| Three times | 119 | 29.4 | |
| Four times | 159 | 39.2 | |
| PNC visit | Yes | 288 | 71.1 |
| No | 117 | 28.9 | |
| Frequency of postnatal care visit | 1 | 164 | 57 |
| ≥ 2 | 124 | 43 |
Table 2. Distribution of obstetrics related characteristics participants visiting Jimma University medical center, Jimma, Southwest Ethiopia, 2020.
Effective breastfeeding technique
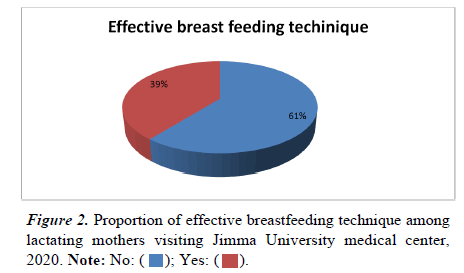
The overall proportion of effective lactation technique (attachment, positioning and suckling) in the study area was 39.3% (Figure 2).
Breast feeding positioning, attachment and suckling
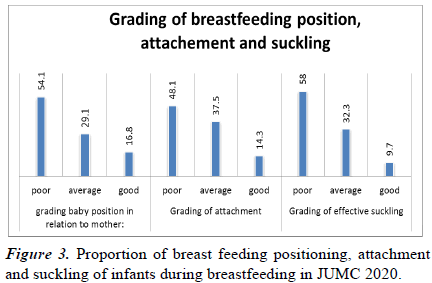
From 405 study participants, correct positioning (16.8%), appropriate attachment (14.3%), and good suckling (9.7%) were observed during breastfeeding in Figure 3.
Factors associated with the practice of effective breast feeding technique
To identify independent variables which had association with lactation technique, logistic regression analysis was performed. From the multivariable analysis; three variables were significantly associated with the practice of effective breastfeeding techniques. The odds of practicing effective breastfeeding technique in primipara (first time) mother were 38.6% (AOR=0.614; 95% CI (0.379, 0.995)) lower compared to multiparous women. The probability of practicing effective BFT in unmarried women was 63.5% (AOR=0.375; 95% CI (0.182, 0.774)) less than married women. The likelihood of having effective BFT was 69.2% less than (AOR=0.318; 95% CI (0.199, 0.510)) among mothers who didn’t receive immediate BFT counselling after delivery compared to their counterparts in Table 3.
| Variables | Category | Effective breastfeeding technique | Ineffective Breastfeeding Technique | COR (95% CI) | AOR (95% CI) |
|---|---|---|---|---|---|
| Marital status | Unmarried | 11 | 43 | 0.351(0.175,0.703)** | 0.375(0.182,0.774)** |
| Married | 148 | 203 | 1 | 1 | |
| Parity | Primipara | 60 | 124 | 0.596(0.397, 0.895)* | 0.614(0.379, 0.995)* |
| Multipara | 99 | 122 | 1 | 1 | |
| Antenatal counselling about BFT | Yes | 114 | 145 | 1 | 1 |
| No | 45 | 101 | 0.567(0.369, .870) | 0.778(0.488, 1.240) | |
| Immediate BFT counselling after delivery | Yes | 123 | 124 | 1 | 1 |
| No | 36 | 122 | 0.297(0.190,0.465)*** | 0.318(0.199, 0.510)*** | |
| Previous experience of breast feeding | Yes | 101 | 132 | 1 | 1 |
| No | 58 | 114 | 0.661(0.440, 0.994) | 0.904(0.556, 1.469) |
Table 3. Factors associated with the practice of breastfeeding techniques among lactating mothers visiting JUMC, 2020
Discussion
In this study, the overall practice of effective breast feeding technique (positioning, attachment and suckling) was 39.3%. The result of this study are consistent with studies conducted in Harar city, eastern Ethiopia (43.4%), South Ari, southern Ethiopia (36.5%), and Cheluvamba hospital in India (43%) (7,10,11). However, the finding of current study is lower than the study conducted in Libya (48%) [9]. The variation may be due to the variation in sample size (the current study had a larger sample size than previous studies) as well as differences in health care setup, socio-cultural and study period.
The present study revealed that the practice of effective breast feeding technique were 39.6% less likely in primipara (firsttime) mothers compared to their counterparts [10]. The overall proportion of this study are consistent with studies in India, Libya, and southern and eastern Ethiopia [11–17]. This is because multiparous mothers might have greater knowledge and skill in breastfeeding and they have more child care experience including breastfeeding technique from their previous pregnancies and deliveries than primiparous (firsttime) mothers.
Another explanatory variable which had a significant association with effective breast feeding technique was marital status. The probability of practicing effective lactation technique was 63.5% less likely in unmarried women than their counterparties. This finding was supported by studies conducted in Nepal and Ethiopia [18–20]. This may be due to the encouragement that married women receive from their spouses and shared activities that encourage breastfeeding.
Immediate breast feeding technique counselling after delivery was another significant variable for the practicing effective lactation technique in this study. Mothers who did not receive counseling on breastfeeding strategies immediately after birth were 69.2% less likely compared to their counterparts. This finding is supported by studies conducted in Heraa general hospital in India, Raipur city in Chhattisgarh, Rural Nagpur, Harar, and South Ari district in Ethiopia [7,13,21]. This may be due to the fact that adequate breastfeeding counseling in the postpartum period is necessary for effective breastfeeding practice. Thus, mothers receiving counseling can demonstrate correct attachment and position and receive feedback from their healthcare providers about their experiences [22].
Conclusion
The overall proportion of practicing effective breast feeding technique was lower than world health organization recommendation. Independent variables: Marital status of the mother, parity (number of birth), and counselling immediately after delivery about BFT were significant variables associated with the practice of effective breast feeding technique. Hence, before discharge the mother, each mother should be observed for the mother’s and infant’s attachment, and effective suckling at the onset of breastfeeding. Besides, special emphasis should be placed on primipara and unmarried mothers’ immediately after delivery and in the Expanded Program of Immunization (EPI) unit to improve breastfeeding techniques.
Limitations of the study
Even though, both an observation checklist and an interview administrated questionnaires was used to assess the practice of effective breast feeding technique, this study was conducted in one public facility and hence can´t be generalized to other hospitals in Ethiopia.
Declarations
Acknowledgment
The authors extended their acknowledgement to all the mothers and neonates who participated in the study. We would like to convey our gratitude for data collectors, supervisors and Jimma University medical center staffs.
Ethical approval
Ethical clearance was obtained from the institutional review board of Jimma university. An official letter of cooperation was obtained from the Jimma university medical center. Informed consent was obtained from each participant prior to the interviews. The participants were assured that the information they were going to give would be used only for the purpose of the study and that all information obtained from the study participants would be kept strictly confidential.
Funding
The authors declared that no funding.
Declaration of conflicts of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article
Availability of data
All data are available upon request
Authors' contributions
All authors (TW, AM, WM, and AY) contributed to the study conception, design, data acquisition, data entry, data analysis, data interpretation, drafting the manuscript, editing, and critically reviewing the manuscript. The final manuscript was read and approved by all authors.
References
- WHO. Protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services. World Health Organization. 2017; 1–136.
- Health MOF. Integrated management of newborn and childhood illnesses (IMNCI). 2018; 1–64.
- Zimmermann M. Infant and young child and feeding. Mountain research and development. 2004; 19–23.
- Parashar M, Singh S, Kishore J, et al. Breastfeeding attachment and positioning technique, practices, and knowledge of related issues among mothers in a resettlement colony of Delhi. Infant, Child, Adolesc Nutr. 2015; 7(6): 317–22.
- Radzewicz E, Milewska M, Mironczuk-Chodakowska I, et al. Breastfeeding as an important factor of reduced infants’ infection diseases. Prog Heal Sci 2018; 8(2): 70–4.
- WHO. Guideline: Counselling of women to improve breastfeeding practices. 2018.
- Tiruye G, Mesfin F, Geda B, et al. Breastfeeding technique and associated factors among breastfeeding mothers in Harar city, Eastern Ethiopia. Int Breastfeed J 2018; 13(1): 1–9.
- Kronborg H, Væth M. How are effective breastfeeding technique and pacifier use related to breastfeeding problems and breastfeeding duration? Birth. 2009; 36(1): 34–42.
- Banginwar A, Toweir A, Goyal R, et al. Breastfeeding practices: Positioning, attachment (latch-on) and effective suckling-A hospital-based study in Libya. J Fam Community Med 2011; 18(2): 74.
- Hanne Kronborg, Michael Væth P. How effective breastfeeding technique and pacifier are use related to breastfeeding problems and breastfeeding duration one. 2009; 36(1): 34-42.
- Nagendra K, Shetty PN, Rudrappa S, et al. Evaluation of breast feeding techniques among postnatal mothers and effectiveness of intervention: Experience in a tertiary care centre. Sri Lanka Journal of Child Heal 2017; 46(1): 39–43.
- Degefa N, Tariku B, Bancha T, et al. Breast feeding practice?: Positioning and attachment during breast feeding among lactating mothers visiting health facility in Areka Town, Southern Ethiopia 2019; 2019.
- Yilak G, Gebretsadik W, Tadesse H, et al. Prevalence of ineffective breastfeeding technique and associated factors among lactating mothers attending public health facilities of South Ari district, Southern Ethiopia. PLoS One 2020; 15(2): 1–15.
- Goyal RC, Banginwar AS, Ziyo F, et al. Breastfeeding practices?: Positioning, attachment (latch-on) and effective suckling–A hospital-based study in Libya. J Family Community Med 2011; 18(2): 74–79.
- Mamta P, Satyavir S, Bilkish N, et al. Breastfeeding attachment and positioning technique, practices, and knowledge of related issues among mothers in a resettlement colony of Delhi. 2015; 7(6): 1-6.
- Suresh S, Sharma KK, Saksena M, et al. Predictors of breastfeeding problems in the first postnatal week and its effect on exclusive breastfeeding rate at six months: Experience in a tertiary care centre in Northern India. Indian J Public Health 2014; 58(4): 270–3.
- Ulak M, Chandyo RK, Mellander L, et al. Infant feeding practices in Bhaktapur, Nepal: A cross-sectional, health facility based survey. Int Breastfeed J 2012; 7: 1–8.
- Egata G, Berhane Y, Worku A. Predictors of non-exclusive breastfeeding at 6 months among rural mothers in east Ethiopia: A community-based analytical cross-sectional study. Int Breastfeed J 2013; 8(1): 15–20.
- Mamo K, Dengia T, Abubeker A, et al. Assessment of exclusive breastfeeding practice and associated factors among mothers in West Shoa zone, Oromia, Ethiopia. Obstet Gynecol Int 2020; 2020.
- Gupta SA, Sharma M, Ekka A, et al. Effect of health education on breastfeeding initiation techniques among postnatal mothers admitted in a tertiary care centre of Raipur city, Chhattisgarh. Int J Community Med Public Heal 2018; 5(10): 4340.
- Thakre SB, Thakre SS, Ughade SM, et al. The breastfeeding practices: The positioning and attachment initiative among the mothers of rural Nagpur. J Clin Diagnostic Res 2012; 6(7 SUPPL.): 1215–8.
- El-Khedr SM, Lamadah SM. Knowledge, attitude and practices of Saudi women regarding breast feeding at Makkah Al Mukkaramah. J Biol Agric Healthc 2014; 4(9): 56–65.
 ); Frequency: (
); Frequency: ( ).
).