Research Article - The International Tinnitus Journal (2020) Volume 24, Issue 1
The eight cervical nerves and its role in Tinnitus
1Department of Pain Therapy, Pain Clinic De Bilt, The Netherlands
2Department of Neurology, OLVG, Amsterdam, The Netherlands
3Zaans Medisch Centrum, Zaandam, The Netherlands
Send correspondence to: Henk M. Koning Department of Pain Therapy, Pain Clinic De Bilt, Netherlands, E-mail: hmkoning@pijnkliniekdebilt.nl Phone: +0031302040753.
Paper submitted on January 27, 2020; and Accepted on February 20, 2020
Citation: The eight cervical nerves and its role in Tinnitus. 24(1):15-20.
Abstract
Introduction: The eight cervical nerves might be a source of input to the auditory system.
Objectives: The object was to assess the efficacy of infiltration of the eight cervical nerve root for treating tinnitus patients and to find indicators for a successful result.
Design: Retrospective cohort study. Subjects were 79 tinnitus patients visiting our clinic in a three-year period and who were treated with infiltration of the eight cervical nerve root.
Results: Twenty-six percent of the tinnitus patients had a reduction of their tinnitus following an infiltration of the eight cervical nerve root. Most of the successfully treated patients rated the effect of therapy as a moderate reduction of 25% to 50%. Fifty percent of the successful treated patients still had benefit at 6.6 months. In 5% of the patients, their tinnitus was aggravated after the infiltration of the eight cervical nerve roots. Patients with a hearing loss at 500 Hz that exceed the hearing loss at 2 kHZ responded the most to infiltration of the eight cervical nerve.
Conclusion: Infiltration of the eight cervical nerve root reduced the intensity of tinnitus in 26% of the cohort of 79 tinnitus patients with a moderate to good effect. This therapy for tinnitus patients’ needs to be considered, especially in those with a hearing loss at 500 Hz that exceed the hearing loss at 2 kHZ.
Introduction
The somatosensory system innervating the head, neck, and shoulders is closely associated with the auditory system [1-4]. Neurons that link to the auditory pathway reside in the dorsal root ganglia of the second, the seventh, and the eight cervical nerve and in the trigeminal ganglion [3]. Treatment of the second cervical nerve can result in a reduction of the intensity of tinnitus for a subgroup of tinnitus patients [5]. However, there are no studies of therapy of the eight cervical nerve in tinnitus patients. The object was to assess the effect of infiltration of the eight cervical nerve root for treating tinnitus and to find indicators for a successful result.
Materials and Methods
Design: A monocenter retrospective cohort study.
Ethical Approval: Approval was given by the Medical research Ethics Committees United (Nieuwegein, the Netherlands).
Subjects: Patients with tinnitus lasting longer than 1 month and referred to Pain Clinic De Bilt by their general practitioner or otolaryngologist. Additional inclusion criterium was a magnetic resonance imaging of the brain in patients with unilateral tinnitus. All patients treated with infiltration of the eight cervical nerve roots for tinnitus in our clinic in a three-year period (October 2016 - October 2019) were included.
Outcome: The primary outcomes were self-reported benefit at 7 weeks on a 4-point Likert scale (none [0%], slight [less than 25%], moderate [25% to 50%], good [50% or more]), and the period of relief.
Adverse Effects: Adverse events were recorded, whether or not caused by the procedure.
Infiltration of the Eight Cervical Nerve Roots: All infiltrations of the eight cervical nerve were performed on an outpatient basis. The patient was in supine position during the procedure. The radiographic projection was in oblique view with the neural foramen of the eight cervical nerve at its largest diameter. This level was marked with a pointer on the skin and used as entry point for the needle. The puncture site was disinfected and a 23-gauge needle (Top Neuropore needle XE-S, Tokyo, Japan) was introduced. Under X-ray guidance, the needle tip was placed at the opening of the foraminal canal of the eight cervical nerve. Under continuous fluoroscopic guidance, 0.5 ml Iohexol (Omnipaque 240, Eindhoven, the Netherlands) was injected. The contrast should be seen to flow around the nerve root but should not flow proximally into the epidural, subdural, or subarachnoid space. After confirming the needle position and without aspirating of blood, a mixture of 0.5 ml bupivacaine 0.5% (Bupivacaine Aurobindo, Baarn, the Netherlands) and 0.5 ml dexamethasone (Dexamethasone CF, Etten-Leur, the Netherlands) were injected. The patients were reevaluated 7 weeks following therapy.
Data Assessment: The charts of all tinnitus patients were reviewed retrospectively to select those who underwent an infiltration of the eight cervical nerve for tinnitus. Data recorded from these patients included tinnitus characteristics, self-reported benefit at 7 weeks on a 4-point Likert scale (none [0%], slight [less than 25%], moderate [25% to 50%], good [50% or more]), and the duration of action. The findings of the audiogram at the worst side of the tinnitus were used for analysis. In case of tinnitus with equal intensity on both sides, the mean of the audiographic findings was used for analysis. The lateral cervical spine radiograph was used for measuring the parameters of the cervical vertebral column [6]. Seven weeks after the procedure, further therapy of tinnitus was continued. If patients underwent other treatments, the duration of action until the next treatment was recorded. All tinnitus patients with a good result following infiltration of the eight cervical nerve root and without relapse, were requested for an interview. In December 2019, an assessment by telephone took place to evaluate the time of recurrence of their tinnitus.
Statistical Methods: The data were statistical analysed with Minitab 18 (Minitab Inc., State College, PA, USA). For continuous and for dichotomous variables, Student’s t-test and χ2 test were calculated respectively. Survival analysis techniques computed the duration of the effect of therapy. Multiple regression analysis obtained a model to predict a successful result on tinnitus. Discriminant analysis evaluated the correlation of variables with the result of the infiltration of the eight cervical nerve root. A P-value less than 0.05 was statistically significant.
Results
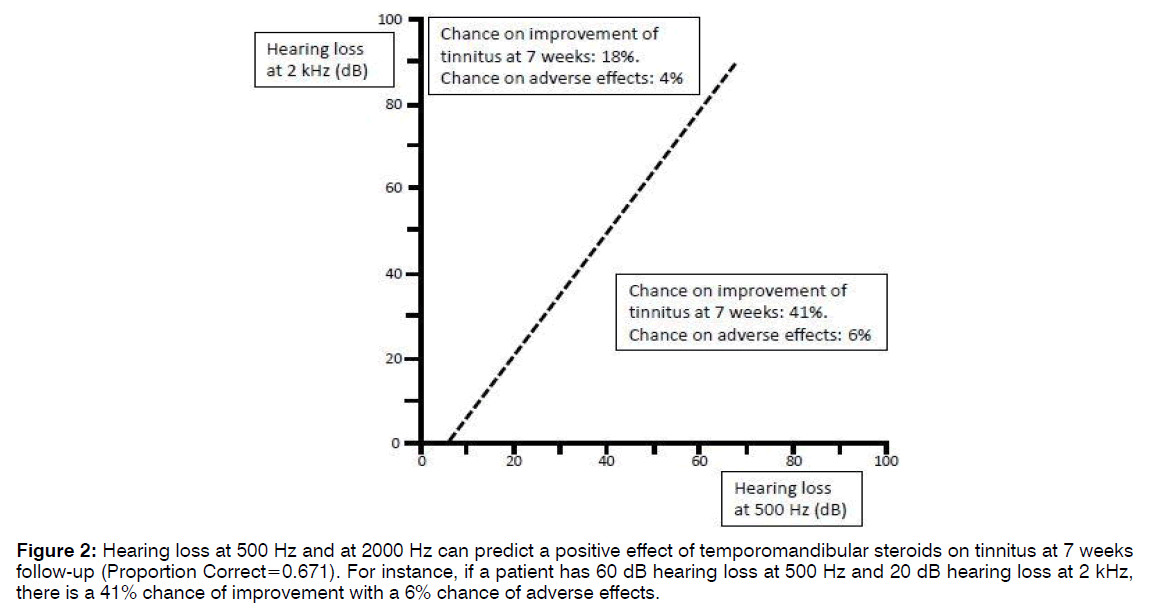
In a three-year period, 79 tinnitus patients underwent with infiltration of the eight cervical nerve root. A description of this patient is shown in Table 1. There was three dropouts. Twenty of seventy-six patients (26%) observed a reduction of their tinnitus afterwards and they rated the improvement as: 25% good, 55% moderate, and 20% slight. In 5% of the patients, their tinnitus was aggravated after the infiltration of the eight cervical nerve root. Figure 1 shows a Kaplan-Meier plot indicating the probability of permanent tinnitus relief after successful infiltration of the eight cervical nerve root. Fifty percent of the successful treated patients still had benefit at 6.6 months. Patients with a positive result of infiltration of the eight cervical nerve root on the tinnitus were compared with the other patients (Table 2). Reduced hearing at the lower frequencies (250-1000 Hz) was found in the group of patients with a positive outcome of infiltration of the eight cervical nerve root on tinnitus, however it was not statistical significant. Multivariate analysis indicated that reduced hearing at 500 Hz and at 2000 Hz predict successful outcome of infiltration of the eight cervical nerve root on tinnitus (p=0.037). With discriminant analysis, the patient group with a higher chance on positive result of infiltration of the eight cervical nerve root was identified (Figure 2). Patients fulfilling these criteria, 41% of them were successfully treated with infiltration of the eight cervical nerve root. The criteria shown in Figure 2 had a sensitivity of 55% and a specificity of 71% for predicting a successful response following infiltration of the eight cervical nerve root in patients with tinnitus. Positive and negative predictive values were 41% and 82% respectively.
| Prevalence | Median | Q1 – Q3 | |
| Age (year) | 60 | 52 – 67 | |
| Gender (male) | 67% | ||
| Unilateral tinnitus | 39% | ||
| Self-perceived hearing loss | 71% | ||
| Cervical pain | 62% | ||
| Period of tinnitus (year) | 7.0 | 2.5 – 17.0 | |
| Hearing loss (dB) at: | |||
| 250 Hz | 15 | 10 – 31 | |
| 500 Hz | 15 | 10 – 30 | |
| 1 KHz | 15 | 10 – 40 | |
| 2 KHz | 20 | 10 – 40 | |
| 4 KHz | 40 | 25 – 60 | |
| 8 KHz | 60 | 35 – 73 |
Table 1: Clinical characteristics of the patients with tinnitus.
| Positive effect of therapy of nerve C8 (n=20) | No effect of therapy of nerve C8 (n=56) | P-value | |||||
| Prev. | Mean | SEM | Prev. | Mean | SEM | ||
| Age (year) | 58 | 2.3 | 60 | 1.7 | 0.619 | ||
| Gender (male) | 65% | 68% | 0.816 | ||||
| Unilateral tinnitus | 40% | 38% | 0.844 | ||||
| Self-perceived hearing loss | 75% | 68% | 0.546 | ||||
| Cervical pain | 65% | 64% | 0.954 | ||||
| Age at the start of tinnitus (year) | 49 | 2.4 | 48 | 2.0 | 0.794 | ||
| Hearing loss (dB) at: | |||||||
| 250 Hz | 31 | 5.8 | 21 | 2.7 | 0.153 | ||
| 500 Hz | 32 | 5.8 | 22 | 2.9 | 0.129 | ||
| 1 KHz | 32 | 5.8 | 22 | 2.9 | 0.145 | ||
| 2 KHz | 30 | 5.0 | 27 | 3.2 | 0.608 | ||
| 4 KHz | 43 | 4.7 | 45 | 3.4 | 0.701 | ||
| 8 KHz | 56 | 6.5 | 57 | 3.8 | 0.887 | ||
| Angle between vertebrae C2 and C6 (degrees): | 9 | 2.0 | 8 | 1.4 | 0.652 | ||
| Farfan’s measurement of disc space height (%): | |||||||
| C2-C3 | 39 | 1.9 | 39 | 1.1 | 0.872 | ||
| C3-C4 | 36 | 1.3 | 35 | 1.3 | 0.582 | ||
| C4-C5 | 33 | 2.0 | 34 | 1.1 | 0.645 | ||
| C5-C6 | 27 | 2.1 | 25 | 1.2 | 0.386 | ||
| C6-C7 | 24 | 2.0 | 26 | 1.1 | 0.435 | ||
| Size of anterior osteophyte (%) at: | |||||||
| C3 | 7 | 1.1 | 8 | 0.7 | 0.449 | ||
| C4 | 10 | 1.2 | 12 | 1.0 | 0.477 | ||
| C5 | 20 | 1.9 | 19 | 1.2 | 0.475 | ||
| C6 | 14 | 1.4 | 14 | 0.9 | 0.966 | ||
Table 2: Patients with a positive effect of therapy of the eight cervical nerves on their tinnitus at 7 weeks were compared with nonresponders.
Figure 2: Hearing loss at 500 Hz and at 2000 Hz can predict a positive effect of temporomandibular steroids on tinnitus at 7 weeks follow-up (Proportion Correct=0.671). For instance, if a patient has 60 dB hearing loss at 500 Hz and 20 dB hearing loss at 2 kHz, there is a 41% chance of improvement with a 6% chance of adverse effects.
Discussion
Infiltration of the eight cervical nerve root reduced the intensity of tinnitus in 26% of the cohort of 79 tinnitus patients with a moderate to good effect. 50% of the successful treated patients still had benefit at 6.6 months. Patients with a hearing loss at 500 Hz that exceed the hearing loss at 2 kHZ responded the most to infiltration of the eight cervical nerve.
Tinnitus can be related to the nervous system of the cervical spine [2]. The cervical structures evoke inhibitory and excitatory responses in the dorsal cochlear nucleus with a predominance of inhibitory responses [7,8]. Activation of the dorsal root ganglia can cause disinhibition of the dorsal cochlear nucleus eventually resulting in tinnitus [9]. The neurons that cross-connect to the auditory system are present in the dorsal root ganglia of the second, the seventh, and the eight cervical nerve, and in the trigeminal ganglion [1-3]. In our study, we observe an effect of infiltration of the eight cervical nerve root in 26% of the tinnitus patients, indicating that the eight cervical nerve is involved in the pathogenesis of tinnitus.
The dorsal root ganglion is the origin of the dorsal columnmedial lemniscal system (Figure 3). The dorsal columnmedial lemniscal system mediates proprioception and discriminative sensation, and includes the cuneate nucleus. The dorsal root ganglia of the seventh and the eight cervical nerves project to the cuneate nucleus [10]. The cuneate nucleus transmit their information to the granule cell domain of the cochlear nucleus [4]. The granule cell domain is a part of extralemniscal auditory pathway ending at the secondary auditory cortex [1]. It can stimulate the central auditory system in a manner distinct from acoustic stimulation and it is linked to the limbic system. The extralemniscal auditory system is related to mechanisms underlying tinnitus
A disbalance between the auditory and the somatosensory input to the auditory pathway can elicit tinnitus [11]. Reduced auditory input makes the dorsal cochlear nucleus more sensitive to trigeminal stimulation [8]. It seems that these findings could also be valid for input from the cervical dorsal root ganglia. In our study, a successful result of infiltration of the eight cervical nerve root was associated with a hearing loss at 500 Hz that exceed the hearing loss at 2000 Hz.
Cervical spine disorders can trigger tinnitus [12,13]. Degenerative changes in the lower cervical spine are reported to only rarely cause tinnitus, while instability at the craniocervical junction or dysfunction between the second and the fourth cervical vertebrae more often results in tinnitus [13]. However, we found that in 26% of all tinnitus patients the eight cervical nerve is probably involved in the pathogenesis. Also, most of the tinnitus patients had disc degeneration between the fifth and the seventh cervical vertebrae in combination with an anterior osteophyte of the fifth cervical vertebrae. Statistical analysis of the effect of nerve infiltration of the eight cervical nerve did not show any significant difference for signs of degenerative changes of the cervical spine. It could be possible that we did not include the correct cervical level in our study. The intervertebral disc between the seventh cervical and the first thoracic vertebrae is difficult to assess on the lateral cervical spine radiograph of the cervical spine, because of the projections of the shoulders.
Limitations are the retrospective design, the outcome measures, and the number of patients in our study. A prospective study is recommended. Another limitation is the use of lateral cervical spine radiograph in this study. MRI might be a better choice for observing any pathology between the seventh cervical and the first thoracic vertebrae.
Conclusion
Modification of somatosensory input the auditory system can be useful for treating tinnitus patients. Infiltration of the eight cervical nerve root reduced the intensity of tinnitus in 26% of the cohort of 79 tinnitus patients with a moderate to good effect. This therapy for tinnitus patients’ needs to be considered, especially in those with a hearing loss at 500 Hz that exceed the hearing loss at 2 kHZ.
Conflict of Interest
The authors declare no potential conflict of interest on publishing this paper.
References
- Dehmel S, Cui YL, Shore SE. Cross-modal interactions of auditory and somatic inputs in the brainstem and midbrain and their imbalance in tinnitus and deafness. Am J Audiol. 2008;17:193-209.
- Ralli M, Altissimi G, Turchetta R, Mazzei F, Salviati M, Cianfrone F, et al. Somatosensory Tinnitus: Correlation between cranio-cervico-Mandibular Disorder History and Somatic Modulation. 2016;21:372-82.
- Zhan X, Pongstaporn T, Ryugo DK. Projections of the second cervical dorsal root ganglion to the cochlear nucleus in rats. J Comp Neurol. 2006:496:335-48.
- Shore S, Zhou J, Koehler S. Neural mechanisms underlying somatic tinnitus. Prog Brain Res. 2007;166:107-23.
- Koning HM, Ter Meulen BC. Pulsed radiofrequency of C2 dorsal root ganglion in patients with tinnitus. Int Tinnitus J. 2019;23:91-6.
- Koning HM, Koning MV, Koning NJ, Ter Meulen BC. Anterior Cervical Osteophytes and Sympathetic Hyperactivity in Patients with Tinnitus: Size Matters. Int Tinnitus J. 2018;22:97-102.
- Bressi F, Casale M, Papalia R, Moffa A, Di Martino A, Miccinilli S, et al. Cervical spine disorders and its association with tinnitus: The "Triple" hypothesis. Med Hypotheses. 2017;98:2-4.
- Shore SE, Koehler S, Oldakowski M, Hughes LF, Syed S. Dorsal cochlear nucleus responses to somatosensory stimulation are enhanced after noise-induced hearing loss. Eur J Neurosci. 2008;27:155-68.
- Levine RA. Somatic (craniocervical) tinnitus and the dorsal cochlear nucleus hypothesis. Am J Otolaryngol. 1999;20:351-62.
- Arvidsson J, P faller K. Central projections of C4-C8 dorsal root ganglia in the rat studied by anterograde transport of WGA-HRP. J Comp Neurol. 1990;292:349-63.
- Shore SE. Plasticity of somatosensory inputs to the cochlear nucleus implications for tinnitus. Hear Res. 2011;281:38-46.
- Simmons R, Dambra C, Lobarinas E, Stocking C, Salvi R. Head, Neck, and Eye Movements That Modulate Tinnitus. Semin Hear. 2008;29:361-70.
- Montazem A. Secondary tinnitus as a symptom of instability of the upper cervical spine: operative management. Int Tinnitus J. 2000;6:130-3.