Research Article - Journal of Parasitic Diseases: Diagnosis and Therapy (2018) Volume 3, Issue 1
The effectiveness of microscopy: Rapid diagnostic test and molecular assay in diagnosing malaria.
Obimakinde ET*, Simon-Oke IA and Osunyemi OS
Department of Biology, Federal University of Technology, Akure, Nigeria
- *Corresponding Author:
- Obimakinde ET
Department of Biology
Federal University of Technology
Akure, Nigeria
Tel: +2347032801215
E-mail: ebenobim@gmail.com
Accepted on February 26, 2018
Citation: Obimakinde ET, Simon-Oke IA, Osunyemi OS. The effectiveness of microscopy: Rapid diagnostic test and molecular assay in diagnosing malaria. J Parasit Dis Diagn Ther. 2018;3(1):10-14. doi: 10.4066/2591-7846.1000022
DOI: 10.4066/2591-7846.1000022
Visit for more related articles at Journal of Parasitic Diseases: Diagnosis and TherapyAbstract
This study was carried out to determine the effectiveness of microscopy, Rapid Diagnostic Test (RDT) and molecular Technique in diagnosing malaria infection in patients at the Federal University of Technology Health Centre, Akure. A total of One hundred and forty (140) patients with malaria symptoms between December 2015 and February 2016 were involved in the study. Prior to the commencement of the research work, approval was given by the Health Research Ethics Committee (HREC) of the University. Blood samples were collected from patients having malaria symptoms and transferred into ethylendiamine tetra-acetic acid (EDTA) container to prevent coagulation of the blood. Malaria screening was done using microscopy method, Rapid Diagnostic Test and molecular assay. The microscopy method used was thick and thin blood film microscopy technique stained with Giemsa stain. Malaria Plasmodium falciparum antigen detection kit was used for Rapid Diagnostic Test while molecular Assay was carried out using nested PCR approach with suitable primers. Chi-square analysis was used to analyze the data obtained from the study. It was observed that P. falciparum was the only species of Plasmodium found in the study area. Result of the study revealed that prevalence of malaria obtained from the samples analyzed using microscopy, Rapid Diagnostic Test and molecular assay ranges from 65% to 73.57%. The molecular assay revealed the highest prevalence of (103)73.57% followed by microscopy analysis (100)71.43% and Rapid Diagnostic Test (91) 65% with no significant difference at P =0.265. It was observed that of the three techniques, Molecular assay and Microscopy were most sensitive for malaria diagnosis. However, molecular assay is expensive, takes time and requires a very standard laboratory with well trained personnel. Therefore, the use of microscopy technique for malaria screening is recommended from this study due to its high sensitivity, cheap cost and low technicality compared to the use of molecular analysise.
Keywords
Malaria, Microscopy, RDT, Molecular, Diagnosis.
Introduction
Malaria is a deadly infectious disease cause by a protozoan parasite of the genus Plasmodium. It is a major public health problem in tropical and subtropical region of the world. Plasmodium falciparum has been incriminated to cause the most serious and sometimes fatal type of malaria most especially in Africa. The other human malaria species, P. vivax, P. ovale, P. malariae, and sometimes P. knowlesi which cause acute, severe illness but mortality rates are low [1,2].
Death rates of 10-30% have been recorded among people of young age referred to hospitals with severe malaria, although in underdeveloped and remote regions where diagnosis and treatment are not readily available, these rates are higher [3,4]. As at 2015, it was estimated that 429,000 deaths from malaria occurred globally most deaths were estimated to have occurred in the World Health Organization (WHO) African Region (92%), followed by the WHO South-East Asia Region (6%) and the WHO Eastern Mediterranean Region (2%) with almost all deaths (99%) resulted from P. falciparum malaria. Also, in 2015, 303,000 malaria deaths were estimated to have occurred in children aged less than 5 years, equivalent to 70% of the global total and is estimated to take the life of a child every 2 minutes [5]. In Nigeria, malaria accounts for over 60% outpatient visits and 30% hospital admissions [6].
There are several techniques use for diagnosis of malaria out of which includes the Microscopy method, Rapid Diagnostic Tests and Molecular Assay. Microscopy method of diagnosis of malaria parasite involves the use of stained blood smears. This method has been in use for century and has been the main tool for diagnosis of malaria in laboratories [7]. This method is relatively simple and requires less training of the microscopists; with an average sensitivity of about 50-100 parasites per microliter of blood [8,9]. Also, this method detects different species of Plasmodium in specimens.
Rapid Diagnostic Tests are based on the detection of antigens derived from malaria parasites in lysed blood, using immuno-chromatographic methods. Currently, this method is increasingly in use for diagnosis of malaria parasite due to the fact that it is rapid, easy to use and does not require much training or special equipment [10]. However, there are limitations to the use of this method because the method is not sensitive to identify different species of Plasmodium and the low sensitivity to detect parasitemia, if the intensity is less than 100 parasites per microliter of blood [11,9]. Molecular technique of detecting malaria parasite is a very sensitive and accurate method of malaria diagnosis. There are two basic approaches for species detection in this method, single Polymerase Chain Reaction (PCR) and nested-PCR. Generally, nested-PCR is more sensitive than single PCR [12]. This method makes use of nuclear small subunit (SSU) rRNA genes as targets for detection of malaria in human. Research has shown that the target genes have highly conserved regions and their copy numbers range from 4 to 8. This feature makes these genes suitable for phylogenetic studies and molecular detection of different species of Plasmodium parasites [13]. Molecular technique is a very sensitive method of diagnosis of malaria parasite that can detect very low parasitemia level which the microscopy and the Rapid Diagnostic Tests cannot detect [14]. Therefore, it is employed for confirmation of diagnosis, epidemiological studies, drug efficacy assessment and to measure the accuracy of microscopy and Rapid Diagnostic Tests [15].
The major means to effective disease management is quick and accurate diagnosis, it is one of the main interventions of the Global Malaria Control Strategy [16,1]. However, malaria infection cannot be diagnosed with symptoms only, it should be confirmed by laboratory diagnosis [17,18]. The aim of the study is to determine the effectiveness of three different diagnostic methods (microscopy, Rapid Diagnostic Test and molecular assay) in the diagnosis of malaria infection in patients at the Federal University of Technology Health Centre, Akure. The study focused on the diagnosis of Plasmodium falciparum base on the fact that previous researches indicated it is the major species that causes malaria infection in the study area.
Materials and Methods
Study area
The Federal University of Technology is located in Akure, the capital city of Ondo State, Nigeria. Akure is located in the rain forest zone between latitude 7°15ꞌ0ꞌꞌN and longitude 5°11ꞌ42ꞌꞌE. Akure has two seasons, which includes the rain (wet) season that ranges from March to October and the dry season that ranges from November to February. Akure has an average annual rainfall of 2378 mm, with temperatures ranging from 25.2 to 28.1°C and relative humidity of 80%. The University Health Centre attends to both Staff and Students of the University.
Ethical clearance
Prior the commencement of the study, approval was given by the Health Research Ethics Committee (HREC) of the University, the chief medical director of the health Centre and from patients for collection of blood who were clearly informed on the aims and objectives of the study.
Patients and sample collection
A total of One hundred and forty (140) symptomatic patients were involved in the study between December 2015 and February 2016. With the use of needle and syringe, two to three blood samples were collected from each patient intravenously. The blood samples were transferred directly into an ethylene diamine tetra-acetic acid (EDTA) container to prevent the blood samples from coagulation.
2-3 drops of blood from EDTA container were spotted on a 3 mm whatmann filter paper (inscribed between a cardboard paper to avoid contamination with other samples) and allowed to dry properly under room temperature. Whatmann filter papers having the dry spots were placed in a plastic container after which desiccants were added to prevent air reaction. The container was stored in refrigerator at 40C. The samples were later transported to the Molecular Entomology and Parasitology Laboratory of the Nigeria Institute of Medical Research (NIMR) for molecular analysis.
Microscopy screening
Thick and thin blood smear were used for microscopic screening of samples using standard protocol as used by [19].
Thick blood smear
With the use of pasture pipette, two-three drops of blood from EDTA container was taken and placed on a clean grease-free glass slide, the blood on the slide was allowed to dry after which the film was stained with Giemsa stain for 15 minutes, [20]. After 15 minutes, the stain was washed off rapidly with distilled water and allowed to dry. Two drops of immersion oil was added to the film and then view under the microscope at x100 objective lens for characteristics features of malaria parasite [21].
Thin blood smear
The same procedures as the thick blood smear was employed but a single drop of blood prepared in a thin film was used.
Rapid Diagnostic Test (RDT)
Malaria Plasmodium falciparum antigen detection kit (Antech Diagnostics Limited, UK) was used for diagnosis. The content of the kit includes, test cassette sealed in an aluminum pouch, Assay diluents (buffer) and pipette.
The cassette was removed from the pouch and placed on a plain surface. With the use of pipette in the kit, about 10 μl of blood was taken from the EDTA container and transferred into the sample well in the cassette. Three drops of buffer was added to the blood in the sample well after which was left for some minutes and allowed to flow to the result window on the cassette. After 15 minutes, the cassette was then checked for the appearance of coloured lines on the result window.
The test was interpreted to be positive if a coloured line appeared at the control region of the cassette and at the test region while the test was interpreted to be negative if only a single coloured line appeared at the control region of the cassette and non at the test region.
Molecular Screening
Deoxyribonucleic Acid (DNA) extraction
DNA was extracted from dry blood spots on the whatmann filter paper with the use of Jena Bioscience DNA Extraction Kit which contains all necessary materials and reagents for extraction. RNase A and Proteinase K were added to the mixture during extraction to degrade all RNA and proteins present [22].
Molecular screening of DNA samples for malaria parasite (Plasmodium falciparum)
After extraction of DNA, molecular screening of samples for P. falciparum was done using nested PCR approach. Master mix, primers and double distilled water were used during the reaction. The master mix consist of; DNA Polymerase, 5x Reaction Buffer B (0.4 M Tris-HCl, 0.1 M (NH4)2 SO4, 0.1% w/v Tween-20), 7.5 mM MgCl2 (1 x PCR solution-1.5 mM MgCl2) 1 Mm dNTPs of each (1 x PCR solution – 200 μM dCTP, 200 μM dGTP and 200 μM dTTP), Blue dye (migration equivalent to 3.5-4.5 kb DNA fragment), yellow dye (migration rate in excess of primers in 1% agarose gel: ˂ 35-45bp) and compound that increases sample density for direct loading.
PCR Nest 1 reaction
With the use of a micro pipette, 2 μl of each DNA samples was put into PCR tubes, 9 μl of double distilled water was added into the tubes, 0.5 μl each of both forward and reverse primer of rP were added after which 2.5 μl of mater mix was added. The PCR tubes containing the mixture were then loaded into the PCR machine.
PCR Nest 2 reaction
The product of the PCR nest 1 reaction was used for the nest 2 reaction. With the use of a micro pipette, 2 μl of the PCR nest 1 products were put into a new set of PCR tubes, 9 μl of double distilled water was added into each of the tubes, 0.5 μl each of both forward and reverse primer of rPf were added after which 2.5 μl of mater mix was added.
Agarose gel (2%) was prepared, after preparation of the agarose gel; the gel was placed in an electrophoresis tank. Six micro liter (6 μl) of DNA ladder (molecular weight marker) was loaded into every first wells on the gel, while the 10 μl of positive control (positive for P. falciparum) was loaded in every second wells and 10 μl of negative control (negative for P. falciparum) was loaded in every third well. In subsequent wells, 10 μl of each PCR Nest 2 products were loaded (in sequential other following the serial number at which each of the samples were labeled).
After loading the wells, the electrophoresis tank was connected to power source of 100V for 40 minutes. The DNA ladder, positive controls and other DNA samples migrated towards the positive terminal of the tank (since the DNA samples were negatively charged). After disconnecting from the power source, the gel tray was brought out from the electrophoresis tank; the gel was carefully removed from the tray and then placed under ultra violet (UV) transilluminator for viewing. The image of the gel under the UV transilluminator was captured and saved (Table 1) [23].
| Species | Primer | Sequence (5_–3_) | PCR Conditions | Size (Base pair, bp) |
Reference |
|---|---|---|---|---|---|
| Plasmodium (Nest 1) | rP: Foward Reverse |
CCTGTTGTTGCCTTAAACTTC TTAAAATTGTTGCAGTTAAAACG |
Intial denaturation, 950C for 3min; 30 cycles of 950C for 30s, 580C for 30s, 720C for 1min; final elongation 720C for 5 min and post hold at 80C. | 1,100 | [23] |
| P. falciparum (Nest 2) | rPf: Foward Reverse |
TTAAACTGGTTTGGGAAAACCAAATATATT ACACAATGAACTCAATCATGACTACCCGTC |
Intial denaturation, 950C for 3min; 30 cycles of 950C for 30s, 600C for 30s, 720C for 45s; final elongation 720C for 5 min and post hold at 80C. | 205 | [23] |
Table 1. PCR primer, sequence conditions and base pair for Molecular screening.
Statistical Analysis
Prevalence was calculated using the formula;
The data generated were analyzed using the Statistical Package for the Social Sciences (SPSS) version 19. The statistical parameter that was used for the analysis of the data was the Pearson’s Chi-Square Test, P at 0.05.
Results
A total of 140 symptomatic patients were screened for malaria parasite during this study. Result from the microscopy screening revealed that 100 (71.43%) of the patients were positive for the parasite. Thin film of the microscopic analysis revealed that all the positive patients were positive for Plasmodium falciparum. Using a Rapid Diagnostic Test kit specific for P. falciparum for malaria screening, of all the 140 patients screened, 91 (65%) of the patients were positive for the parasite. However, molecular analysis carried out on the samples revealed that 103 (73.57%) patients were positive for the parasite. Statistical analysis revealed that there was no significant difference from the data obtained from the three diagnostic methods (P=0.265) (Table 2).
| Results | Diagnostic Technique | ||
|---|---|---|---|
| Microscopy | Rapid Diagnostic Test | Molecular | |
| Positive | 100 (71.43%) | 91 (65%) | 103 (73.57%) |
| Negative | 40 (28.57) | 49 (35%) | 37 (26.43%) |
| Total | 140 | 140 | 140 |
χ2= 2.653, df= 2, P= 0.265
Table 2. Result of Malaria screening among patients using Microscopy, Rapid Diagnostic Test and Molecular Techniques.
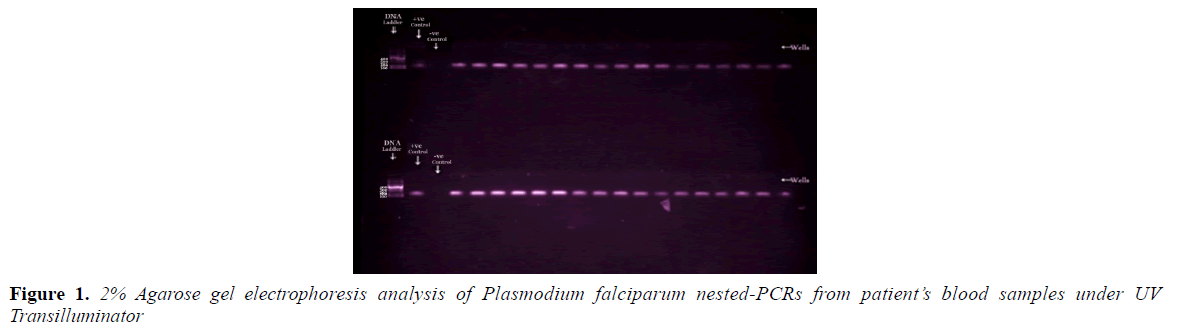
The gel image in Figure 1 shows distinctively separated bands of varying bands/base pairs. DNA Ladder of 100 bp was loaded at the first well; the second wells loaded with control positive samples showed bands that separated from the well to a base pair of 205 bp, while the third wells loaded with control negative samples did not separate from the well. Some of the PCR Nest 2 products loaded in subsequent wells showed bands at the same level with the positive control bands at 205 bp indicating that the samples were positive for Plasmodium falciparum, while those that did not separate from the well indicated that they were negative for P. falciparum. The same processes were carried out for all other PCR Nest 2 products.
Discussion
Three different diagnostic methods (microscopy, Rapid Diagnostic Test and molecular assay) were used for screening of symptomatic patients. During the study, the only species of Plasmodium found was P. falciparum which has been known to be the major cause of malaria in Africa [24]. Molecular assay of the samples also confirmed positive all positive samples from both microscopy and Rapid Diagnostic Test diagnoses. This is similar to previous reports that Molecular assay is highly sensitive when compared to both microscopy and Rapid Diagnostic Tests [15,7].
The prevalence of P. falciparum obtained from the sampled patients ranges from 65% to 73.57%, this prevalence is high when compared to the 36.0% prevalence reported by [7] in Luanda, Angola. The high prevalence of 71.43% revealed by microscopic analysis 65% prevalence recorded by Rapid Diagnostic Test also disagrees with the report of [7] where the microscopic analysis revealed 34.7% and Rapid Diagnostic Test 44.44%.
Molecular assay revealed the highest prevalence (73.57%) of malaria infection than the microscopy (71.43%) and Rapid Diagnostic Test (65%). This result agrees with the findings of [25] in their study in Imo state, Nigeria and [26] in their study in Kano, North-Western, Nigeria where their microscopic analysis presented higher prevalence than the Rapid Diagnostic Test. It has been discovered by several researchers that molecular assay has higher sensitivity that microscopy and Rapid Diagnostic Tests [15,7]. The highest prevalence recorded by molecular assay could be that some of the patients were having very low parasitemia level in which only molecular assay that has a very high sensitivity can detect, it can detect as low as 1-5 parasite per microliter of blood [27]. Reported that microscopy has an average sensitivity of about 50-100 parasites per microliter of blood while Rapid Diagnostic Tests are not sensitive to detect parasitemia intensity of less than 100 parasites per microliter of blood. From this fact, using the molecular technique as a reference technique, some of the patients, 12 (11.65%) positive for malaria parasite had very low parasitemia level which Rapid Diagnostic Test was not sensitive enough to detect. Low parasitemia level in these patients could be as a result of self-medication in which the patients might have taken some antimalarial drugs or herbs without doctor’s prescription before coming to the Health centre for malaria test which could have wiped out significant amount of the parasite from the blood.
However, it was observed that the microscopy technique revealed a prevalence (71.43%) which was almost the same as the molecular assay (73%). This indicates that microscopic method of screening of malaria parasite is very reliable.
Conclusion
This study has compared different diagnostic methods of screening falciparum malaria in the study area. The Molecular and Microscopy analyses revealed the highest prevalence of the infection, however molecular assay is expensive and requires a very standard laboratory with well trained personnel. The Rapid Diagnostic Test revealed the lowest prevalence of the infection which could probably be as a result of its inability to detect parasites when counts are very low but it is very quick and convenient to use. Therefore, use of microscopy method for malaria screening is recommended due to its sensitivity, cheap cost and low technicality compare to the use of molecular method.
Conflict of Interest Statement
Authors declare that there is no conflict of interest.
Acknowledgement
Authors are grateful to Dr. T. S Awolola and entire staff of the Molecular Entomology and Parasitology Laboratory, NIMR for their effort towards the accomplishment of this study. Appreciation goes to the entire staff and corp members of the Medical Laboratory of FUTA Health Centre for their support. Also appreciation goes to Mr. Adesina Oluwafemi for the statistical analysis.
References
- Tangpukdee N, Duangdee C, Wilairatana P, et al. Malaria diagnosis: a brief review. Korean J Parasitol. 2009;47(2):93-102.
- Caraballo H. Emergency department management of mosquito-borne illness: malaria, dengue, and West Nile virus. Emerg Med Pract. 2014;16(5):1-23.
- World Health Organization. World Health Organization expert committee report on malaria: 20th report; 2000. World Health Organization, Geneva, Switzerland. 2000;p:71.
- Chotivanich K, Silamut K, Day NPJ. Laboratory diagnosis of malaria infection – a short review of methods. N Z J Med Lab Sci. 2007;61(1):4-7.
- www.who.int/ith/diseases/malaria/en/
- Federal Ministry of Health. A road map for malaria control in Nigeria, a bridged version, Abuja. Strategic plan 2009-2013. Yahian Press Ltd. 2010;p:155.
- Pembele GN, Lázara RR, Jorge F. Detection and species identification of malaria parasites by Nested-PCR : comparison with light microscopy and with SD BIOLINE malaria Ag Test in Luanda, Angola. Int J Trop Dis Health. 2015;10(1):1-13.
- Wongsrichanalai C, Barcus MJ, Muth S, et al. A review of malaria diagnostic tools: microscopy and rapid diagnostic test (RDT). Am J Trop Med Hyg. 2007;77:119-27.
- Iglesias N, Subirats M, Trevisi P, et al. Performance of a new gelled nested PCR test for the diagnosis of imported malaria: comparison with microscopy, rapid diagnostic test, and real-time PCR. Parasitol Res. 2014; 113(7):2587-91.
- McMorrow ML, Aidoo M, Kachur SP. Malaria rapid diagnostic tests in elimination settings-can they find the last parasite? Clin Microbiol Infect. 2011;17(11):1624-31.
- De Monbrison F, Angei C, Staal A, et al. Simultaneous identification of the four human plasmodium species and quantification of plasmodium DNA load in human blood by real-time polymerase chain reaction. Trans R Soc Trop Med Hyg. 2003;97(4):387-90
- Proux S, Suwanarusk R, Barends M, et al. Considerations on the use of nucleic acid based amplification for malaria parasite detection. Malar J. 2011;10:323.
- Fuehrer HP, Noedl H. Recent advances in detection of Plasmodium ovale: implications of separation into the two species Plasmodium ovale wallikeri and Plasmodium ovale curtisi. J Clin Microbiol. 2014;52(2):387-91.
- Taylor BJ, Howell A, Martin KA, et al. A labon- chip for malaria diagnosis and surveillance. Malar J. 2014;13:179.
- Golassa L, Enweji N, Erko B, et al. Detection of a substantial number of submicroscopic Plasmodium falciparum infections by polymerase chain reaction: a potential threat to malaria control and diagnosis in Ethiopia. Malar J. 2013;12:352.
- World Health Organization. A global strategy for malaria control Geneva, World Health Organization. 1993.
- Kesinee C, Kamolrat S, Nicholas PJD. Laboratory diagnosis of malaria infection-a short review of methods. N Z J Med Lab Sci. 2007;61(1):4-7.
- Kipanga PN, Omondi D, Mireji PO, et al. High-resolution melting analysis reveals low Plasmodium parasitaemia infections among microscopically negative febrile patients in western Kenya. Malar J. 2014;13:29.
- Pembele GN, Da Silva F, Ferreira C, et al. Evaluación de la calidad del diagnóstico de la malaria por microscopía óptica en laboratorios provinciales de la República de Angola. Rev Cub Med Trop. 2014;66:191-201.
- Giemsa G. Technique for thick blood film, Zbl. Bakt. Ref. 1902.
- Dacie JV, Lewis SM. Preparation and staining methods for blood and bone marrow films: laboratory aspects of blood transfusion. Practical Haematology (9th Edn). Churchill Livingstone, Edinburgh, London 2001;19-46;471-92.
- www.jenabioscience.com/images/PDF/pp-213.pdf. 2015
- BMRL (Biomedical Research Laboratoy). Molecular detection of malaria Parasites manual. Faculty of Medical Laboratory Sciences, University of Khartoum. 2010.
- Mordi RM, Borke ME. The prevalence of malaria in Edo State, Nigeria. Nigerian J Parasitol. 2013;34(2):41-6.
- Umeh SI, Enwuru CP, Egbuobi RC. Diagnosis of malaria in pregnancy: a comparison of microscopy with rapid diagnostic tests. Microbiol Res Int. 2013;1(3):35-9.
- Mohammed Y, Dabo NT, Kawo AH, et al. Comparison of microscopic examination and rapid diagnostic tests used to diagnose malaria among pregnant women in Kano, North–Western, Nigeria. Int J Sci Technol. 2015;5(2):47-52.
- Färnert A, Arez AP, Babiker HA, et al. Genotyping of Plasmodium falciparum infections by PCR: a comparative multicentre study. Trans R Soc Trop Med Hyg. 2001;95:225-32.