Review Article - Journal of Pain Management and Therapy (2017) Volume 1, Issue 1
The effectiveness of exercise on function for adults with shoulder impingement syndrome (sis): a structured literature review.
Mussa El Mughrabi1, Adel El Alwani2, Naser Amein2 and Adel Almangoush3*
1Glasgow Caledonian University & Higher Institute of Medical Professions – Benghaz, Glasgow, United Kingdom
2Higher Institute of Medical Professions – Benghaz, United Kingdom
3Salford University, Salford, United Kingdom
- *Corresponding Author:
- Adel Almangoush
Salford University
United Kingdom
Tel: 00447979771883
E-mail: salford2013@gmail.com
Accepted date: November 14, 2016
Abstract
Objective: To examine the effects of exercise on the function of adults with shoulder impingement syndrome (SIS).
Design: A structured literature review of randomized controlled trials (RCTs).
Methods: Studies were identified from databases searched from 2007 to April 2016 MEDLINE, EMBASE, PEDro, Sports Discus, AMED and Cochrane Library, only one reviewer selected studies meeting inclusion criteria. The methodological quality of the included studies was independently assessed by the same reviewer using the PEDro quality assessment tool.
Results: Eight studies were included in the review and appraised for content. Five studies achieved a score of 6 or above indicating good quality, tree trials were rated as moderate quality. No study achieved lower <4 to indicate poor quality.
Conclusion: Due to the lack of a detailed description of the exercise protocols used, the current evidence is difficult to interpret in relation to use in clinical practice. Therefore, future RCTs studying exercise therapy should also concentrate on the effect of different exercise protocols, including the intensity, duration, frequency and load of the exercises.
Background
Description of the condition
Shoulder impingement syndrome (SIS) is a common disorder that results in the disability and functional loss for patients overall [1,2]. Around 1% of adults seek medical attention for shoulder pain each year. It is the third most common musculoskeletal reason for general practitioner consultations and estimates of its prevalence in the UK range from 7% to 26% [3]. Also, an epidemiological survey of this phenomenon based on job title and cumulative exposure found at the 95% confidence interval for slaughterhouse workers, indicating the prevalence of this condition amongst shoulder intensive positions [4,5]. There are a variety of interrelated pathologies that are present within Subacromial Impingement Syndrome; these include partial thickness of rotator cuff, tendinosis, subacromial bursitis and calcific tendinitis. Each of these can be categorized as SIS and can present in relatively similar manners through initial clinical investigation. Mostly, these pathologies would lead to rotator cuff injuries, which affect the supraspinatus superiorly, subscapularis anteriorly, the infraspinatus and tears minor posteriorly [5].
These lead to impingement syndrome in the shoulder and are common amongst those who raise their upper arm a shoulder level for extended periods of time and this is prevalent amongst those who play various sports. It is a lifelong process that culminates through three stages. In order for proper diagnosis, it is imperative that proper detection and quantification of rotator cuff tears must be provided to gauge the severity and create valuable prognosis for the patient and this would be contingent towards the proper treatment mechanisms that can strengthen and deter the advancement specifically of Stage I of SIS [6].
The pain caused by the SIS can significantly diminish the quality of life that patients endure [7,8]. It occurs in three stages based on severity and duration of the condition: Stage I is characterized by localized inflammation, swelling and is seen in patients under the age of 25 years old. This may be due to overusing the muscle or pain from acute trauma. Shoulder impingement at this stage is reversible [9]. Stage II is associated with a progression and tear in the rotator cuff. This condition is not reversible yet can be affected through rest and conservative precautions. Patients with stage II impingement may require surgical intervention [1]. Stage III SIS is demonstrated amongst those over the age of forty as a destruction of soft tissue and rupture of the rotator cuff. Physical and other surgical interventions are necessary frequently in this stage.
When shoulder symptoms are present for more than three months during the past year, it is possible to diagnose impingement. Magnetic Resonance Imaging (MRI) techniques allow differentiation to guide further physiological management [10].
Description of the intervention
There are numerous management techniques through physiotherapy that aim to assist symptoms of SIS. Exercise and manual mobilization are some common forms that have been proved efficacious [11,12]. Treatment is subjective to the dependence of training and requires careful evaluation. The common theme is an element of exercise that can benefit any physiotherapy program for SIS. Therefore, exercise is a valuable intervention that can potentially provide benefits to patients suffering from shoulder pain of this variety. Should exercise can promote strengthening, relief of pain and healing that can reverse conditions of abnormal muscle imbalance. These can restore a pain-free sate of motion [13]. Since Stage I of SIS can be reversed according to the proper management and exercise, it is possible that loaded exercise can demonstrate benefits towards the management of the disorder [14]. This disorder does not have to self-limiting as shoulder impingement can frequently be seen as refractory and patients can benefit from nonsurgical intervention. Therapeutic exercise programs can add value to patients with initial stages of impingement (McClure et al, 2004). This is due to the ability for physical exercise to restore mobility and stability through enhancement of glenohumeral and scapulothoracic muscular function. It has been demonstrated further that the incorporation of active exercise in combination with joint mobilization and other modalities of therapy can be beneficial towards healing shoulder impingement and limiting the pain that patients experience while assisting in reversal of the condition [14].
How the intervention might work?
Shoulder pain can decrease as a result of strength through exercise. These changes are relevant to the improvement of functional activities such as simple forward reaching or overhead extension [6]. Exercise, especially in therapeutic forms can determine long-term benefits that result in optimal conditions for strengthening functions. In his way, exercise could contribute to increased pain-free range of motion as well as significant reduction in overall shoulder pain [14].
Since SIS has been managed with exercise, the results of particular mechanisms would be based on the unique protocol established by the particular exercise regime [15]. In demonstrating the three dimensional scapular kinematics, functional limitations and physical impairments that could be changed through exercise, it can be demonstrated that passive ranges of motion could increase for both internal and external rotation [14]. Exercise can potentially diminish pain, increase shoulder functions and related physical functions. Combined with proper education and effective strategies, simple exercise routines can contribute to patient expansion and understanding of the underlying improvement techniques and mechanisms. Since it is unclear how the specific nature of this modality works because of the highly diversified nature of clinical presentations and exercise regimes, further research and incorporation of specific assessments on the range of motion and other qualitative perceptions the patient may face is necessary to elucidate how the intervention will work [15].
Why It Is Important To Do This Review?
It is important to study the effect of exercise on shoulder impingement in order to review the validity of the intervention as well as comparisons regarding usual care amongst physiotherapy. By utilizing only randomized controlled trials (RCTs) it is possible to trials to assess the intervention group with regards the therapeutic exercise and combination exercises. In evaluating the effectiveness of exercise the purpose of this investigation will be identify functional improvement to the shoulder amongst adults.
Since it has been demonstrated that certain elements of patient discomfort can be managed through the use of exercise, exploring this review will provide a clear and useful explanation of the specific function that exercise can provide for SIS. Studying this area of treatment can help cultivate an understanding of the efficacy that certain exercise has for patients with clinical signs of SIS. While there are documented examples of the value that physiotherapist initiated and led programs have towards managing pain, there are significant areas of comparison that will illustrate the benefit of exercise in comparison to other non-surgical and surgical interventions alike [1]. Such an understanding can assist in creating physiotherapy plans that involve useful aspects for the diversified type of pain or condition that a patient experience. In such a way the modality of healing and improvement will be contingent on education and practice that a physiotherapist can involve within their practice for maximum efficacy and value towards patient healing. Previous reviews had a similar aim as the current review were constrained by the limited number of good-quality studies and available methodological quality was generally poor, with no sample size calculations, lack of detail on interventions and lack of blinding of outcome assessment [16,17].The uncertainty for the effects of exercises on function, pain, muscle strength and quality of life needs a recent review with up to date studies.
The objectives
To examine the effects of exercise on the function of adults with shoulder impingement syndrome. In this review the intervention will be compared with standard physiotherapy intervention.
Methods
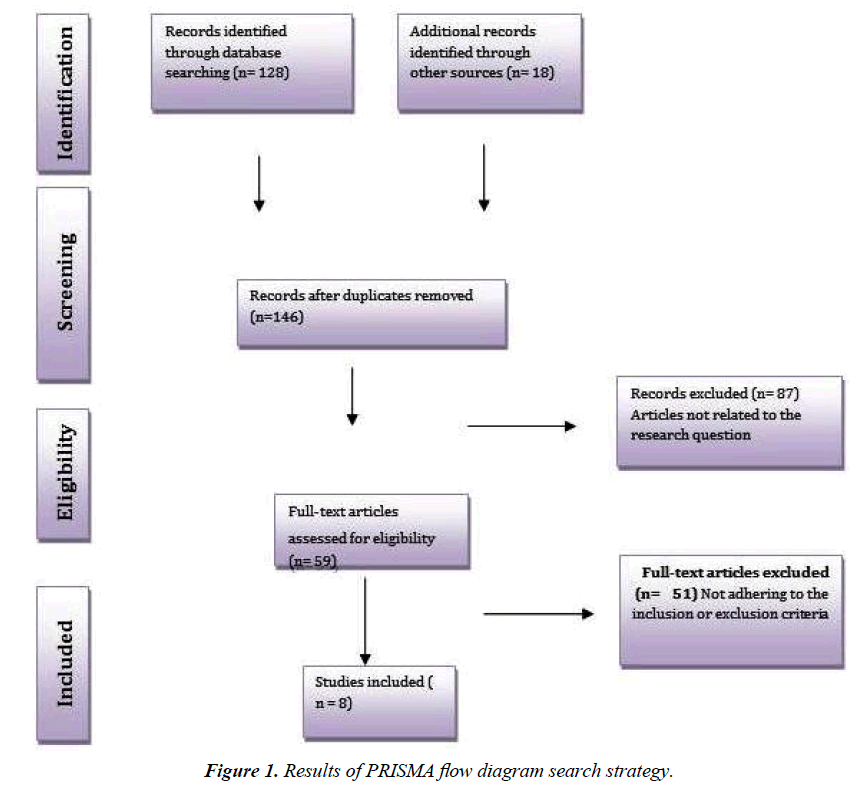
This review was conducted following the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines [18].
Criteria for considering studies for this review
The criteria of inclusion have been adopted because the study aims to be carried out with the minimum bias, and as many grounded conclusions as possible. According to Rochon et al., “one powerful strategy to minimize selection bias is to restrict inclusion in the study to those with a defined diagnosis or specific characteristics” [19].
Types of studies include
Only randomised controlled trails (RCTs) which test the effects of exercise interventions on people with shoulder impingement syndrome (SIS) were included in this review. The participants of the included trails were randomized to the following:
• Intervention group: who will experience a single exercise intervention or a multiple exercise intervention, versus
• Control group: who will experience usual activities, usual health care, electrotherapy, or activities (such as attending recreational or educational activities or groups) that received the same attention (number of attendances at classes or contact with the research team) as the exercise group.
Trials that compare two or more exercise interventions and a control group were also included.
Types of participants
Participant characteristics of interest included adult patients diagnosed with signs and symptoms of SIS Stage 1 or 2. Studies which included participants with SIS stage three, or painful/ stiff shoulder is associated with other diagnoses, e.g. frozen shoulder, or postsurgical patients were excluded.
Type of interventions
Exercise interventions designed to improve SIS were defined as those in which participants exercise their muscles (and neuromuscular responses) against an external force as an outcome of voluntary movement. This was also defined as loaded (against gravity or resistance) exercise or active free exercises (unloaded exercises) as a component of the intervention. Examples of exercise interventions include: functional static and strengthening exercises.
There are different places where the exercise interventions can take place: home, institutions, local community, or at the clinic. They can also be self-monitored by using exercise sheets and video, or they can be monitored by individuals or groups. Different persons can play the role of supervisor: the patients themselves, the patines’ peers, or physiotherapist or any healthcare.
A comparison was made with control groups who performed the usual activities, the usual health supervision, attending different types of activities which are group-related or educational. These activities gain the same attention as the exercise group in terms of the number of attendances or being connected with research team. The studies which include combined interventions were carried out.
Type of outcome measures
The result measures are very significant in any study. The use of the outcome data and investigation will guarantee the strength and validity of the study and it will support it. It will also ascertain that the data has reliability and authority.
Primary outcomes of interest included: Measures of function, such the disability of the arm, shoulder and hand (DASH), patient- reported function (PRF) and quality of life.
Secondary outcomes were: pain and upper limb muscle strength.
Subgroup analysis and investigation of heterogeneity
The data mentioned in the included studies did not enable the researcher to do the following subgroup analysis that was planned a priori: Gender, athletic or not, duration and intensity of exercises sitting of the delivered interventions and types of supervisions.
Search Strategy
To achieve the goal of maximising the relevance of as many types of physiotherapy exercises interventions as possible because of the possibility, because there is a possibility that papers might have been missing through the searches of database, and also to identify different materials and documents. So, a hand search took place for all the relevant articles and reviews. Papers published 2008-2016 were exclusively included. The reason why only these papers were included is that the research studies before those times were assessed in previous reviews Table 1 [20].
| No. | Criteria | Details |
|---|---|---|
| 1 | Database utilized | MEDLINE, Cochrane Library (systematic reviews and controlled trials registers), EMBASE, CINAHL, Science Direct, EBSCO, Physiotherapy Evidence Database (PEDro) & LILACS. |
| 2 | Search used | #1 -(" Shoulder Impingement Syndrome"[Mesh]) (which includes rotator cuff syndrome, bursitis, and tendonitis) #2 -(" Physical Therapy Modalities"[Mesh]) (limited to any type of exercise therapy) |
| 3 | Boolean Operators | AND, OR |
| 4 | Search String with Booleans | ("Shoulder Impingement Syndrome"[Mesh]) AND ("Physiotherapy OR Physical Therapy Exercise Modality" [Mesh] OR "Physical Therapy Specialty"[Mesh]) OR "Exercise"[Mesh]) |
| 5 | Limits | |
| a | Published date | From April 2008 to April 2016 |
| b | Humans/Animals | Humans only |
| c | Type of Studies | Randomised controlled trials (RCTs) |
| d | Language | English |
Table 1. Details of search strategy.
Key words used to extract the relevant articles for
Terms were used to conduct the search “Shoulder Impingement Syndrome” OR “subacromial impingement” AND “physiotherapy exercise intervention” OR "stage I" Or "stage II", musculoskeletal injuries of the shoulder, tendon injuries, preventing sports injuries, stretching, injury (strain, sprain and tendonitis) adult, upper limb, upper extremity, overuse and shoulder injury, to ensure a detailed and comprehensive search strategy Table 2.
| Search term | Limited to | |
|---|---|---|
| 1 | Shoulder pain or shoulder impingement or shoulder tend or shoulder burs or rotator cuff or subacromial impingement or subacromial burs or supraspinatus or impingement or contractile dysfunction or painful arc | Title & abstract |
| 2 | Rotator cuff/shoulder pain/shoulder impingement syndrome | MeSH |
| 3 | 1 or 2 | |
| 4 | Exercise or eccentric or concentric or loaded or resistance or muscle or physiotherapy or physical therapy or rehabilitation or conservative management | Title & abstract |
| 5 | Exercise/resistance training/physiotherapy/physiotherapy or physical therapy specialty/rehabilitation/muscle strength/exercise therapy | MeSH |
| 6 | 4 or 5 | |
| 7 | Randomized controlled or randomised controlled or controlled trial or randomized or placebo or randomly or quasi controlled trial | |
| 8 | Humans NOT Animals | |
| 9 | 3 and 6 and 7 not 8 |
Table 2. An example of the search strategy that was performed on MEDLINE search strategy. This strategy was modified for use on the other electronic databases with support from a librarian.
Study selection process
It is desired that more than one reviewer applies the selection criteria in order to minimise bias in the study selection process [21]. Due to the circumstances of the current study (being a Master degree dissertation with limited time and size), only one investigator took part in the application of the previously determined selection criteria, because it was not possible or easy to have more than one reviewer for the literature review.
The minimization of bias
There can be found bias during the production of a literature review. While the review was being conducted every effort was made to eliminate the following: publication bias, bias in location of studies and biased inclusion criteria [22].
A large number of databases were used in an attempt to guarantee a comprehensive search of articles regardless of type, so as to avoid publication bias. As far as possible, studies conducted in different contexts and environments were sought to avoid bias in the location of studies. Finally, to achieve the goal of eradicating bias in the inclusion criteria, all possible ways were adopted not to select studies on this basis. Articles were instead chosen according to their relatedness to the main question of the review. Each included study was scored independently by the same reviewer, using the criteria made by PEDro critical appraisal tool [23].
Data Extraction
It is advisable to have at least two analysts for extracting and investigating the information in order to prevent extracting information and the inclination to dissect. Anyhow, it was not possible in this review as specified previously. The aim of this procedure was to extract the findings in a consistent manner from each qualified study. The data extraction form underlined the major elements of each study, which is related to the review aim. The data extracted from selected studies were: the authors details, purpose of trial, participant characteristics (mean age, duration of symptoms), type of exercise intervention, outcome measurements and findings.
Methodological quality of articles
The aim of the scholar was to answer the questions of the PEDro chick listed questions. Each one of the papers was read with care and scrutinised twice. In the first time, papers were read quickly using simple approach that is time saving in order to obtain the relevant data. This was done by dividing the checklist which contained 11 items into 4 sections which were highlighted:
• study population study sample
• intervention,
• measurement of effect measuring the outcome
• statistical validity statistical credibility
So, the authors completed answering the questions in a sensible, organised way. Recording related answer in the same colour was found to be time saving, and it also allowed answers to be ready for analysis.
Methodological quality assessment
There is a need that the evidence resulted by the study should be systematically evaluated in order to create strength, reliability and relevance for the research. This should take place before findings are used to make a decision regarding practice and it should be a crucial component in a clinical practice that is based on evidence. The evaluation supports empowering the research understanding and it will also show the interrelatedness between theory and practice that will lead to a more improved healthcare quality [24].
The PEDro critical appraisal tool was used for the assessment of the quality of every single study’s methodology). This is an easy to administer 11-item tool giving information about the internal validity and reporting the statistical outcomes of a RCT (PEDro, 1999). Truthfulness and credibility of the PEDro-scale has been tested by a large numbers of studies and it is commonly accepted as a compatible tool for categorizing RCTs in systematic reviews [23,25]. Data recorded by this outcome measure are descriptions of: eligibility criteria, random allocation, concealed allocation, comparability of groups at baseline, blinding of subjects, blinding of therapists, blinding of assessors, measurement of key outcome in at least 85% of initially allocated participants, intention to treat analysis, statistical comparison between groups and point and/ or variability measure. The only case where discretionary points are granted in the trial is when the information required is evaluated as it is described in the information about additional rating that is provided. Scores for RCTs as rated on the PEDroscale (PEDro, 1999): Excellent quality 9-11; Good quality 6-8; Moderate quality 4-5; any scores below 4 were low quality. This assessment was taken by the same investigator as mentioned above.
The relevant information regarding PEDro criterion was collected by usig all the articles and assessed in accordance to the scoring criteria established by the PEDro database (PEDro, 1999). In order to achieve a lucid comparison of ratings were gathered together on a single spread sheet. The ratings were performed by the author because this study is a requirement of the MSc dissertation; however, this method was confirmed as a possible reason for bias. In order to achieve a lucid comparison of ratings were gathered together on a single spread sheet.
Best evidence synthesis
Best-evidence synthesis criteria were adopted in summarizing the clinical interrelatedness of the qualitative results. Synthesis criteria as presented by [26], which were modified to reflect items that were relevant for trials involving exercise. Consequently, threats to bias were inadequate randomization, inadequately concealed treatment allocation, non-blinding of assessors, no intention-to-treat analysis, and no measurement of compliance with the exercise intervention. In order to summarise the veracity of evidence for each outcome, the PEDro quality classifications were added to the criteria in Figure 1.
Data analysis and synthesis
A meta-analysis is a statistical methodological tool which provides a straightforward estimate of the overall effectiveness of exercise on SIS and increases the power of the analysis [21]. Because outcome measurements and intervention of included studies were heterogeneous, it was not possible to include metaanalysis.
Therefore, a narrative way which uses depiction was adopted for analysis and comparison of findings yielded by the included trials. Recording of problematic effects and dropout rates was done.
Dealing with missing data
In the case when some missing data were found during data extraction, it was attempted to contact the original investigators of the study to request the missing information.
Selection of Studies
146 papers that may be relevant were the result of primary search of the websites as well as hand searches of the list of references. 87 studies were excluded because they did not meet the criteria of inclusion and exclusion. The remaining articles were downloaded with the full texts that were screened as well. However, even the remaining 59 articles were subject to recording and removal of duplicates. In this case, only 8 full texts were maintained and analysed in accordance with the criteria of inclusion and exclusion.
Included Articles
The selection criteria of inclusion that have been adopted allowed only 8 RCTs to be selected. This is a small number but that is what the inclusion criteria permitted the researcher. However, these 8 papers are relevant and valuable because they include relevant) information concerning the effectiveness of exercises on function for adults with shoulder impingement syndrome. The RCTs included in this review were conducted in different places across the world: Norway [27,28], Sweden [29], Brazil [30], UK [31], USA [32], Canada [33] and Belgium [2].
Assessment of Risk of Bias
PEDro scale was used to assess the methodological quality of the included studies. These studies were assessed for bias. The PEDro scale is a rating system which consists of 11items. This system is used for the evaluation of internal validity of RCTs (PEDro 1999). It is a developed and advanced copy of the Delphi list originated by Verhagen et al (1998) and based on ‘the consensus of expert (PEDro, 1999). PEDro scales are considered to be the only one way to evaluate the methodological quality of papers: it is, however, a very common one used to evaluate RCTs included in systematic reviews that looked at physiotherapy intervention. Its use thereby increases the comparability of findings with those of other articles.
The information on eligibility criteria for subjects included and randomization process was provided clearly by 5 of included studies [27-29,31]. Only two trials [31,32] comparing between experimental and control group did not take place and the two groups were not specified. The studies included were all too high to measure the effects for 85% of the patients who were allocated at an initial stage. The intension-to-treat analysis was used in 5 of the included studies. All the studies clearly included between-group comparisons of findings as well as measures of variability Table 3.
| PEDro criteria | Lombardi et al., 2008 | Cloke et al., 2008 | Kachingwe et al., 2008 | Szczurko et al., 2009 | Østerås et al., 2009 | Engebretsenet al., 2009 | Holmgren, et al., 2012 | Maenhut et al., 2013 |
|---|---|---|---|---|---|---|---|---|
| 1. Eligibility criteria | U | Y | N | N | Y | Y | Y | Y |
| 2. Random allocation | Y | U | N | Y | U | Y | Y | Y |
| 3. Concealed allocation | Y | Y | U | Y | N | Y | U | Y |
| 4. Comparable baseline | Y | U | N | Y | Y | Y | Y | Y |
| 5. Subjects blinded | N | N | N | N | U | N | N | N |
| 6. Therapists blinded | N | N | N | N | N | N | N | N |
| 7. Assessors blinded | Y | U | Y | Y | N | Y | Y | N |
| 8. Outcomes for 85% of initial participants | Y | Y | Y | Y | Y | Y | Y | Y |
| 9. Intention-to- treat analysis | Y | N | U | U | Y | Y | Y | Y |
| 10. Between group stat comparison | Y | Y | Y | Y | Y | Y | Y | N |
| 11. Point & variability measures | Y | U | Y | U | U | U | N | N |
| Total score | 8 | 5 | 4 | 6 | 5 | 8 | 7 | 6 |
Table 3. Overview of all PEDro rating performed by the author (Y=yes; N=No; U=Unsure).
Quality of Evidence
Based on the previously determined PEDro scale, five studies were considered to be of good quality [27-29,31]. No study achieved lower <4. The remaining tree trials were rated as moderate quality trials.
Study characteristics
In order to mitigate the effect resulted from the fact that the similarities and differences between the included studies were not uniform, it was suggested that a narrative summation of the results to be used as the most workable way for presenting extracted data Table 4.
| The study |
Interventions | Outcome Measure | Findings |
|---|---|---|---|
| Lombardi et al. 2008 | Intervention group: Progressive exercise resistance training for twice a wk/ 2 mo: Resisted extension/flex/MR/LR, exercise achieved by Multi-pulley muscle building equipment Control group: No treatment |
Function: DASH 3and DASH 2 Pain: VAS 10 cm. QoL: SF-36. Strength: Isokinetic evaluation Timing tests: 0 & 2 mo |
Exercise group displayed significant reduction during movement (P= 0.001), and in pain at rest (P=0.001) and patient reported function and strength and improved QoL, |
| Cloke et al. 2008 |
Exercise parameters up to 6 sessions for 18 wk No additional information given |
Function: OSS. QoL: SF-36 Timing tests: 0 & 18 wk and 1 yr |
No statistically significant between-groups difference at base line or 1-year follow-up. |
| Kachingwe et al. 2008 | Exercise group (1): Posterior capsular exercise & stretching. Exercise group (2): as group 1 plus Mobilizations (GH joint). Exercise group (3): as group 1 plus (Mulligan mobilizations). Control group (4): advice only. Frequency: From 1to 3 groups 1/wk for 6 wk. |
Function: SPADI Pain: 10 point VAS. Timing tests: 0 & 6 wk |
The pain intensity was reduced significantly in all groups. Exercise groups changed clearly on SPADI. |
| Szczurko et al. 2008 | Exercise group: exercise (AROM & passive) & Placebo tablets. once weekly/ 30 minutes/12 wk. Naturopathic group: anti-inflammatorydiet & Acupuncture. (no further detail given) | QoL: SF-36 Pain & disability: VAS & SPADI Timing tests: 0, 4, 8, & 12 wk |
Significantly improvements in QoL & shoulder pain indices for two groups. Naturopatihc group improved significantly in SPADI & disability scores. |
| Osteras et al. 2009 | Frequency: 3 PT sessions/wk12 wk Progressive resistance, Resisted shoulder & elbow (flexion & extension). Group (1) a high-graded exercise therapy (HD), Group (2) a low-graded exercise therapy (LD) |
Function: SRQ Strength: strength (Isometric). Pain: VAS. Timing tests: 0 & 3 mo |
Improvement in function, less pain and significantly greater isometric strength were showed in HD group. |
| Engebretsen et al. 2009 | Exercise group: 1 PT sessions a week for 12 wk. Sling suspension exercises. Shockwave therapy group. |
Function: 7-point rating scale. Pain and disability: SPADI. Pain: 9-point rating scale. Timing tests: 0, 6, 12 & 18 wk |
SPADI scores was significantly different at 6, 12, and 18 wk. in exercise group only. |
| Holmgren et al. 2012 | Weights and resistance bands 3 sets x 15 reps 2x day for 8 weeks then 1x day for 4 weeks 12 weeks pain monitoring Mode Group (1) specific exercise Group (2) control exercise |
Function: DASH Questionnaire EQ 5D and EQ VAS VAS. Constant Murley Score Timing tests: 0 & 3 mo |
The exercise group showed significantly higher DASH & improved significantly in constant Murley Score & VAS. EQ 5D significantly higher at 3 months in the exercise group. |
| Maenhout, et al. 2013 | Abductors Standing, full can, thumb up, abduction in scapular plain. Dumbbells (Heavy load) 3 sets x 15 Reps 2x day, 7 days/week 12 weeks Pain monitoring mode. Group (1) Traditional training rotator cuff Group (2) Eccentric training |
SPADI questionnaire Isometric strength measured using a handheld dynamometer Subjective perception of improvement of shoulder pain (5-point scale SPADI questionnaire. Timing tests: 0, 6 & 12 wk |
Treatment and eccentric training group showed a 15 higher gain In abduction strength at 90° than the treatment group. Both groups showed a significant improvement in SPADI scores over time; No significant differences in patient self-rated perception of shoulder pain Improvement between treatment and exercise groups |
Table 4. Study Characteristics.
Study Population
Diagnostic
A positive (painful) Neer test for the diagnosis of shoulder impingement syndrome and a positive painful Hawkins- Kennedy impingement test were used. The clinical sign of painful arc was considered positive if there was pain originating from the subacromial region of the shoulder during arm active abduction against gravity without resistance and was used only by [31]. Limitation with the functional movement patterns of hand-behind-back or hand-behind-head used by Kachingwe et al. [32]. Also, Speeds, Apprehension, and Subscapularis Lift tests were used by Szczurko et al. [33]. Humerus abducted 90 degrees in the maximal passive inward rotation should give you bacromial pain applied by Østerås et al. [27]. Dysfunction or pain on abduction normal passive glenohumeral range of motion, pain on two of three isometric tests (abduction at 0°or 30° external or internal rotation) used by Engebretsen et al. [28]. Finally, a positive result on Jobes test and positive result on Patte’s manoeuvre were applied by Holmgren et al. [29] and Maenhout et al. [2].
Study size
Sample sizes ranged from a total of 33 participants [32] to 112 in [31]. Østerås et al. and Maenhout et al. studied a sample of 61 participants. Lombardi et al. included 60 participants. Szczurko et al. included 85 patients, Engebretsen et al. studied 104 and Holmgren et al. included 97 participants. With the exception of that conducted by Maenhout et al. a power calculation was not employed in any of the studies to determine the sample size. All articles did not mention the patient’s professions or their physical activities except the study done by Szczurko et al. [33] stated that they involved a member of postal employees. All the studies were ethically approved apart from Szczurko et al. [33] and Engebretsen et al. [28], the status of their study, in this regard, not being stated.
Age, weight and body mass index were reported to be determinants of baseline characteristics. The authors stated that the baseline measurement was significant when assessing a point of departure to which the later measurements can be compared [31,32].
In all the studies under consideration, the age of the patients varied with the youngest being 18 years in the studies and the oldest being 88 years in the study by Cloke et al. [31].The mean age with standard deviation (SD) were not stated in any included studies. All studies included males and females, with no comparison between them as shown in Table 5(a).
| No | Study | No of participants | Age (years) Range Mean (SD) |
|---|---|---|---|
| 1 | Lombardi et al. 2008 | 60 patients; 46 women & 14 men. | Experimental group (mean age 56.3 yr). Control group (mean age 54.8yr). |
| 2 | Cloke et al. 2008 | 112 patients; 64 Women & 48 men. | Age 22 to 88 yr old. |
| 3 | Kachingwe et al. 2008 | 33 patients; 17 men, 16women. | Aged 18-74 yr. |
| 4 | Szczurko et al. 2008 | 85 patients; 50 Women & 35 men. | Aged 18-65 yr. |
| 5 | Osteras et al. 2009 | 61 patients, 51 women & 10 men. | Aged 18-60 yr. |
| 6 | Engebretsen et al. 2009 | 104 patients: 52 Women & 52 men. | Age 18-70 yr. |
| 7 | Holmgren et al. 2012 | 97 participants: 36 female & 61 male | Age 30-65 years |
| 8 | Maenhout, et al. 2013 | 61participants: 16 Female &15 males. | Group 1 means=age 40.2 years. Group 2 means: Age 39.4 years. |
Table 5(a). Participants.
Dropouts
Dropout rates ranged from 5% half of them 2.5% from exercise group Engebretsen et al. [28] to 20% (7 active & 10 control) did not complete the study Szczurko et al. [33]. As shown in Table 5(b). Of the reasons included, one can mention, failure to do it again because of injury, being ill or having to do something else.
| Power Calculation | Ethically Approve | Outline baseline characteristics | Dropouts | |
|---|---|---|---|---|
| Lombardi et al. 2008 | Not reported | yes | yes | 13% |
| Cloke et al. 2008 | Not reported | Yes | Not reported | 20% |
| Kachingwe et al. 2008 | Not reported | Yes | Not reported | Not reported |
| Szczurko et al. 2009 | Not reported | Not reported | Yes | 20% |
| Osteras et al. 2009 | Not reported | Yes | Yes | 8% |
| Engebretsen et al. 2009 | Not reported | Not reported | Yes | 5% |
| Holmgren et al. 2012 | Not reported | Yes | Yes | 8% |
| Maenhout, et al. 2013 | Yes | Yes | Yes | 18% |
Table 5(b). Dropout rates, ethical approvals and power calculation.
Blinding
Participants
It is not easy to be certain that participants are blinded during the studies of exercise intervention. All trials are through and assumed to have a high risk of bias for this item. One study is an exception: it is the study that was rated as not to have clear bias [27]. Another study also attempted to reduce bias by using only the advice of the physician as far as the control group was concerned [32].
Assessors
A total of 5 studies reported that the person who assessed the outcomes was blinded when it came to deal with the allocation of groups [28-30,32,33]. However, 2 studies reported that the assessor was not blinded and there was one study where it was unclear from the translation [27,31].
Interventions
The progressive resistance training (resisted flex/extension) was applied to an exercise groups in two studies [27,30]. While, Cloke et al. applied exercise parameters, Szczurko et al. applied passive and active range of movement (AROM) exercises. Engebretsen et al. used sling suspension exercises with education sessions on anatomy of the shoulder. Holmgren et al. used weights and resistance bands, Maenhout et al. used abductors standing, full can, thumb up, abduction in scapular plain. Finally, Kachingwe et al. had three intervention groups: group one: supervised exercise: exercises and stretching (posterior capsular), group two: supervised exercises as group 1 plus (Mulligan mobilizations) and group three: supervised exercise as group 1 plus joint mobilizations [28,29,31-33].
Exercise delivery
The period of time for the exercise programmes was 6 weeks Kachingwe et al. to a maximum of 18 weeks Cloke et al. with the most frequent being three m12 weeks Szczurko et al.; Østerås et al. Engebretsen et al., Holmgren et al.; Maenhout et al. The individual sessions took place as often as 1-3 sessions a week (Kachingwe et al., Szczurko et al., Holmgren et al. to three sessions a week Østerås et al., in two of the studies, there were two sessions every week Lombardi et al., Maenhout et al. One of the studies reduced the frequency of sessions from twice a week to once a week two months after the intervention had started. Only one study reported the duration of each session; it was a 30-minute session Szczurko et al. [30-33].
Comparison Interventions
Only four trails included a programme of exercise only [27,28,30-33], six other trials included exercise as combined with another type of treatment such as education sessions on anatomy of shoulder [28]. Comparison was made between the exercise interventions and control group. There was no treatment in the control group, injection treatment, anti-inflammatory diet and acupuncture, control exercise, a Shockwave therapy group and traditional training rotator cuff. A low-graded exercise therapy group was compared with low-graded exercise therapy group in Østerås et al. It was not clear that the control group participated in the study conducted by Kachingwe et al. [2,30-33].
Outcome Measures Used
These studies used a multi-outcome measures for function DASH Questionnaire [29], DASH 2 and DASH 3[30] , a selfadministered questionnaire of 12 item 'OSS' [31] shoulder pain and disability index 'SPADI' [2,31,32], SRQ [27] and 7-point rating scale [28]. For pain: 10-point VAS [32], 10 cm VAS [30], 100 mm VAS [27], VAS 0-7 cm [33], 9-point rating scale [28], VAS Constant Murley Score [29] and a handheld dynamometer subjective perception of improvement of shoulder pain (5-point scale SPADI questionnaire) [2]. For Quality of life 'QoL': SF- 36 used by. Finally, strength: Isokinetic evaluation. Isometric strength [2,30-33].
Results of studies (effects of treatments)
A reduction in pain at rest with statistical significance (P=0.001) and during movement (P=0.001) was demonstrated in study carried out by Lombardi et al. All groups in Kachingwe et al. Decreases in pain level before and after the treatment had statistical significance. Also, in Szczurko et al. the two groups participated in the study displayed reduction in shoulder pain and QoL idices. NC group improved significantly over the PE group in SPADI total, pain, and disability subcategory scores NC group demonstrated more improvement than the PE group in SPADI total pain and disability scores. 12 wk: PE group VAS scores prepost test: 4.85 (1.48) to 4.05 (1.69) (P=0.0431). Both groups showed a significant improvement in SPADI scores over time [2]. There was a significant difference between groups (P0.05) in Osteras et al. study. HD group underwent less pain and made improvement and better isometric ABD and ER strength. There was a significant statistical difference of exercise group for SPADI scores at 6, 12, and 18 week which was reported in Engebretsen et al. [28].
In study patients in the extension only group were reported to make more improvement of QoL than those in the control group. Three intervention groups were reported to have a significant change on SPADI [30]. Group 1 and 2 experienced higher changes on all the measures of pain in comparison with the group of exercise alone [32]. Mean score of significant change in the DASH was higher in the specific exercise group. A greater improvement was reported by the specific exercise group according to Murley Score. Mean score changed in VAS at night in a significant way in the specific exercise group. After 3 months, 5D was significantly higher in specific exercise group [29]. Treatment and eccentric training group demonstrated a gain which is 15 higher in abduction strength at 90° than the treatment.
In Cloke et al. there were not significant between- groups differences at the end of intervention or 1 year later. However, according to the outcome of power calculation, 110 patients will need an arm each. Likewise, Kachingwe et al. [32] reported no significant between group differences. No significant differences were reported of VAS activity and rest EQ Holmgren et al. [29]. No significant differences in patient self-rated perception of shoulder pain Improvement between treatment and exercise groups. At the level of patient self-reported perception of shoulder pain Improvement, also there were no significant differences stated.
Discussion
The present review provided data on the evidence for the effectiveness of exercise therapy and several usual care interventions for SIS. Following evaluation of the studies it can only be suggested that exercise is effective in relieving pain and improving function in SIS. The quality of information relating to the type of exercise, duration, intensity, repetitions and progression varied substantially in the included studies. On the basis of the information provided, it would be possible to repeat the exercise programme from only five of the included investigations.
We were able to come to a number of conclusions on the basis of the 8 studies we analyzed. All, however, are accompanied by caveats. First, the over-all results of the qualitative synthesis suggest that exercise is effective at reducing pain and improving function for the 6 to 12-week period following treatment, with this assessment being accepted with caution because it is supported by only 6 and 4 medium/high-quality RCTs, respectively Second, there is strong evidence that the improvements in function are maintained at long-term follow-up. Again this conclusion is accepted cautiously because it is supported by only 2 high-qualities RCTs. Third, there is moderate evidence that exercise is effective in terms of improving short-term strength. Despite descriptions of the exercise protocols, prevented definitive conclusions about which types of exercises and exercise parameters are associated with better outcomes. However, common types of exercise used in high- and medium-quality articles, and associated with decreased pain and increased function, were scapular stability exercises and rotator cuff strengthening exercises using pulley equipment or elastic band resistance and progressing through range to 90° abductions. These were conducted in supervised sessions 1 to 2 times per week and in daily home exercise programs.
Moderate evidence was found in favour of patients who received exercise therapy when compared with patients who had placebo or other physiotherapy modalities. Unfortunately, because of the lack of detailed description of baseline characteristics and exercise protocols used (e.g., intensity, duration, frequency and load), the current evidence is not fully validated and difficult to interpret in relation to use in clinical practice.
Appropriately designed and analysed randomised placebo controlled trials are considered to be the most rigorous study design to assess the effectiveness of a clinical investigation. Due to the diversity of study inclusion criteria, interventions, types of exercise, outcome measurements, follow-up times, and home versus clinic-based programmes, it was considered inappropriate to attempt to pool the results.
It is arguable that, on the basis of the findings, the effect at present should only be considered as modest. It is also not possible to determine if it is exercise alone or exercise in combination with other interventions that offers the greatest benefit. In addition, guidance as to the most appropriate exercise therapy, including duration, intensity and number of repetitions, remains speculative. There is also uncertainty as to when to start and how to progress the exercise programme. There is also no guidance to follow to inform clinicians whether the exercise needs to be specific or general in nature. Additionally, it is unclear why the exercise may be having a beneficial effect. Uncertainty exists regarding the advice a clinician should offer patients concerning the benefit of exercise therapy.
Appropriately designed randomised clinical investigations that address the areas identified as deficiencies in our knowledge base as a result of this review would help to address this lack of understanding and provide clinicians with better and more appropriate information to present to patients to help inform discussions and decisions regarding management and care pathways. For these studies to provide meaningful information, it is imperative that appropriate and validated impairment and disability outcome measures are incorporated into the design. To be able to pool the results from future randomised controlled trials, these studies should endeavour to use the same validated outcome measures.
Implications for Research
Most of the existing studies in this area were found to be poorly reported and lacking sufficient and useable data for the purposes of secondary analyses and summary. Future work in this field needs to conform to the standards laid out in the revised CONSORT statement. Future studies need to consider their choice of outcome measurement so as to ensure clinical relevance. Furthermore, particular consideration should be given to the use of valid and reliable methods for collecting adverse event data. Finally, studies of longer duration are required to establish the necessary length of treatment and longer term outcomes, and studies involving a diverse range of ethnic and cultural groups would ensure greater generalizability of findings.
The benefits of exercise interventions on SIS may be relatively small, so the sample sizes reporte