Research Article - Biomedical Research (2017) Volume 28, Issue 3
The effect of Rhizoma Panacis Japonici ethanol extracts on protein caspase 3 and Drp-1 in MCAO rats
Xiachan Chen1, Ge Zheng2, Mingli Pan2 and Peng Chen3*1Department of Neurology, Ruian People’s Hospital, Wansong Road 108, Ruian City, Zhejiang Province, China
2Department of Paediatrics, Ruian People’s Hospital, Wansong Road 108, Ruian City, Zhejiang Province, China
3Department of Neurosurgery, Ruian People’s Hospital, Wansong Road 108, Ruian City, Zhejiang Province, China
- *Corresponding Author:
- Peng Chen
Department of Neurosurgery
Ruian People’s Hospital, China
Accepted date: September 13, 2016
Abstract
Objective: The effect of Rhizoma Panacis Japonici ethanol extracts on protein caspase 3 and Drp-1 in MCAO rats.
Methods: Sixty male SD rats were randomly divided into 4 groups, the sham operation group (s group), ischemia and reperfusion group (I/R group), Rhizoma Panacis Japonici Ethanol extracts low dose group (10 mg/kg/d, RPJEL) and Rhizoma Panacis Japonici Ethanol extracts high dose group (30 mg/kg/d, RPJEH) with 15 rats in each group. After intragastric administration of 1 W, the middle cerebral artery occlusion method preparation of focal cerebral ischemia model, ischemia 2 hrs and reperfusion for 24 hrs, postoperative 24 hrs monitoring the brain ischemic area middle cerebral artery blood flow changes, the Triphenyltetrazolium Chloride (TTC) method to measure the volume of cerebral infarction was used to detect the apoptosis of brain cells level, immunohistochemistry and Western blot Drp-1, Caspase 3 protein expression.
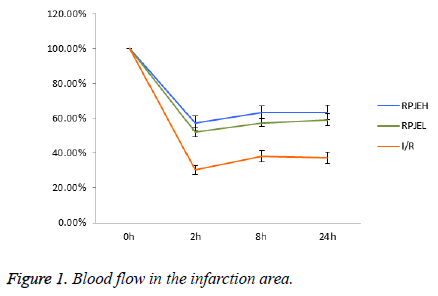
Results: Compared with I/R group, both of RPJEL and RPJEH groups could significantly decrease the Drp-1 and Caspase 3 protein level, and also minimize the infarct volume. Two hours after the infarct model established, the blood flow of I/R group were changed to 30.26% ± 1.58%, and the blood flow of the RPJEL and RPJEH groups were decreased to 52.1% ± 2.94%57.3% ± 4.21%.
Conclusions: RPJE could effectively inhibit the nerve cell apoptosis and mitochondria. The action mechanism may be related to the decreased levels of Drp-1 and Caspase 3.
Keywords
Rhizoma Panacis Japonici ethanol extracts; Ischemia reperfusion; Drp-1; Caspase 3.
Introduction
Mitochondria are an important place for energy metabolism in cell, and also the most possible organelles in the early phase of ischemia. Studies have shown that Drp-1 is important executive mediated mitochondrial fission molecular [1]. Caspase 3 is a sensitive index of the cell apoptosis and the key enzymes of Caspase cascade and executives [2]. Rhizoma Panacis Japonici has root dry, strong body, promoting blood circulation and removing blood stasis, relieve swelling and pain and so on [3]. In recent years, studies showed that cell apoptosis and necrosis ischemic was finished through the two way, quite part of the vessels could recanalized after treatment, the neuron apoptosis is the main form of ischemia half dark belt damaged, the reperfusion injury is inevitable, infarction and expanding, the main reasons may be caused by Drp-1, Caspase 3 and other regulatory factors. But Rhizoma Panacis Japonici ethanol extracts aimed to inhibit the neuron was few reported. In recently, the important clinical therapy of cerebral infarction was early thrombolysis treatment.
Materials and Methods
Operations and the pre-treatment
Sixty male rats was purchased from the Anhui Medical University Animals Center, weight from 250 ~ 300 g, and were randomly divided to four groups, sham group, Infraction/ reperfusion group, and Rhizoma Panacis Japonici Ethanol extracts group including low dose group (10 mg/(kg/d)) and high dose group (10 mg/(kg/d)).
Intragastric administration for one week, and according to the reported files, we make a two hour ischemia model and reperfusion for 24 hours. For the sham group, we instructed the same operation however we didn’t put the embolus in to the middle cerebral artery. According to the Longa score standard [4], we agreed that 0 score were without neurological signs; 1 score: animals cannot fully extend left fore; 2 score: the animals walk to the left circle; 3 score: animal fall in the line to the left side, 4 score: no spontaneous activity, conscious disorder. Neural function defect scale in 1 ~ 3 is divided into the model successfully, 0 score and 4 score, random added in the experiments, ensure that each group of animal number remains the same. Loss score in 1-3 is divided into the model successfully, 0 and 4, randomly added in the experiments, the guarantee animal number remains the same in each group.
The observation of blood flow of MCA [5]
This experiment detected using laser Doppler blood flow of right middle cerebral artery blood supply area changes. Rats prone position and fixed on the operating table, to the top of the head, cut along the line begins at the top of the skin until the skull, used as a starting point to the right anterior fontanelle 5 mm, 3 mm back. Damage the cranial with dental drill plate, the optical fiber probe with biological glue vertical fixed to the skull opening. To test 24 h after surgery on the right side of the brain artery ischemia in the surrounding area (ischemia half dark band) of cerebral blood flow, reduce blood flow was calculated. After the measurement, stitches head incision.
24 h after ischemia, killed and then TTC was conducted. The percentage of the total cerebral infarction group weight equalled to the degree of cerebral infarction. Groups of rats after 24 h was killed and the brain will be put in rats section moulding, starting from the frontal pole 2 mm in, sterile operation section once upon a time in the future for coronary serial section, each piece of 2 mm thickness. Put in brown bottle containing 2% TTC solution, 37°C avoid light incubation for 30 min, white as infarcts, rose red as normal brain tissue, 4% paraformaldehyde fixed fluid, neat order, according to the brain slices vertically, digital camera taking pictures. According to the color separation infarction group and normal tissues carefully after the surgery, weighing respectively. Cerebral infarction volume (%)=pale area weight/ weight (pale area+the pale section weight) × 100%.
The Drp-1, Caspase 3 expression with immunohistochemical methods [6,7]
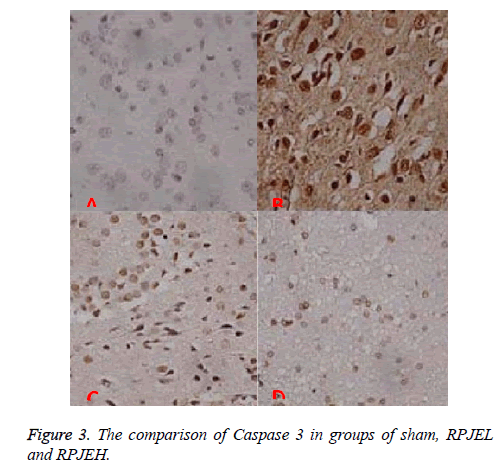
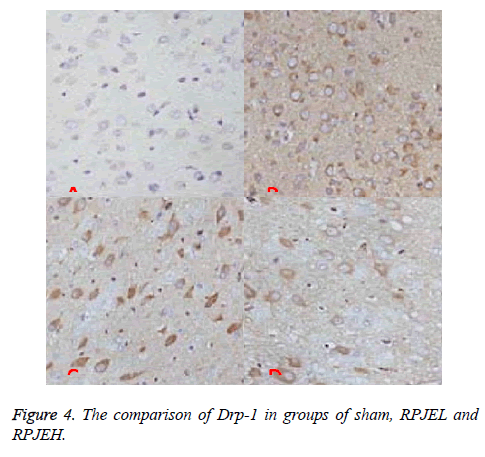
The protein extracted was analysed by immunohistochemistry method, and calculate the total number of positive cells of the percentage of the total number of cells, for targeted protein expression. Randomly selected from each group of rats at five areas of the frontal and parietal cortex, each sample in PBS solution instead of a fight, as the negative control group, the figure in the cytoplasm and (or) nuclei in tan granule cell meter for Drp-1 and Caspase 3 protein positive expression cells. Areas in positive cells randomly selected five non-overlapping horizons at high magnification, the calculation of Caspase 3 and Drp-1 percentage of the number of positive cells. Positive rate (%)=positive cells number/(positive cells number +negative cells number) by 100%.
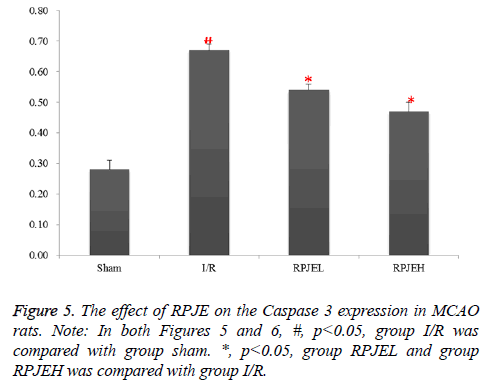
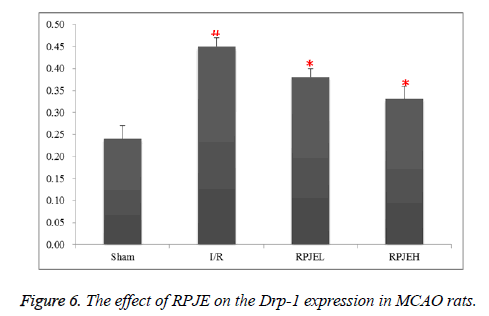
Drp-1 and Caspase 3 expression by Western blot [8,9]
24 h after each surgery, respectively, 10% chloral hydrate was injected into abdominal cavity to get a quick fast anaesthesia. The rat was killed and taken right lateral cortical tissue with injury. Protein lysis fluid was added, grinded cracked for 30 min at 4°C, then transferred to the EP, 13000 g centrifugal 5 min, supernatant was taken for total protein concentration detection with BCA. The protein concentration of Drp-1 and Caspase 3 (Figures 5 and 6).
Statistical methods
SPSS17.0 statistical software analysis was used and the data was expressed with average value ± SE, multigroup comparison was analysed with single factor analysis of variance (F) test. SNK method was applied to pairwise comparison.
Results
Blood flow in the infarction area
24 h after infarction established, the blood flow was decreased to 30.26% ± 1.58% quickly, and the data were also increased to 52.1 ± 2.94%,57.3% ± 4.21% in the both RPJEL and RPJEH. Comparison was conducted in RPJE group and I/R group, we found that there was a significant difference between them. Samely, this difference was also existed in other three time including 2 h, 8 h, 24 h after infarction onset. However, no difference was found in both RPJEL group and RPJEH group, may be we should refined the concentration of the RPJE to get an optimized concentration (Figure 1).
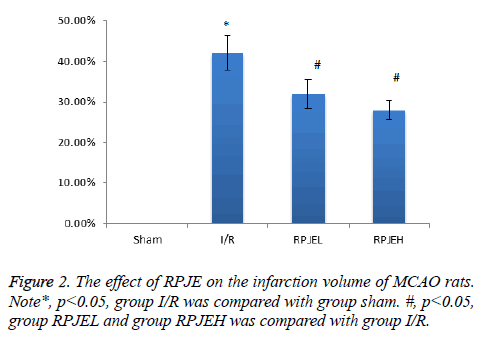
The effect of RPJE on the infarction volume
There was obvious infarction 24 h after the ischemia onset in the I/R group. Compared with the I/R group, the RPJE group including both low dose and high dose both had a great decrease in the infarct volume (p<0.05), however, no difference was existed in the both RPJE group, seen in Figure 2.
Caspase 3 protein positive expression is located in the nucleus, Drp-1 protein positive expression in the cytoplasm, tan grains. Sham group has few positive cell including Caspase 3 (6.05 ± 1.53)Drp-1 (4.52 ± 0.82). Compared with I/R group, the Caspase-3 and Drp-1 cell in RPJE group was decreased significantly. The number decreased in RPJEH was higher than that in RPJEL group, seen in Figure 3.
However, in the sham group, there was little expression, compared with sham group; the level of Drp-1 protein was higher in I/R group. In RPJEL and RPJEH group, was decreased significantly, and also the ratio was bigger in RPJEH group (Figure 4).
The Drp-1 and Caspase 3 protein expression with western blot
Few caspase 3 and Drp-1 protein was expressed in sham group, however, that was higher in I/R group. Samely, in the RPJEL and RPJEH group, the number of caspase 3 and Drp-1 was decreased gradually. The change was most obvious in RPJEH group (Figures 5 and 6).
Discussion
In this research, we could found that RPJE group could effectively decrease the volume of infarction in MCAO rats, then may improve the neurological function, at the same time, it could also decrease the cell apoptosis, this was approved by before studies. The possible action mechanism mainly related to the inflammation reaction and oxidative stress injury after the ischemic reperfusion [10,11], decreased the Ca2+ overload [12].
In the research of effect of Drp-1 on the outer membrane of mitochondria, the over-expression Drp-1 could accelerate the mitochondria lysis [13]; after gene knockout of Drp-1, the expression of endogenous Drp-1 was inhibited, in turn, reduced the lysis of the mitochondria, that meaned Drp-1 was a necessary molecules in mitochondria lysis process.
Up to now, there was no report about the Drp-1 expression in the MCAO rats. Then we made a research design to utilize the Traditional Chinese Medicine the pre-treat the SD rats, than make a MCAO model on it, we found that the expression of Drp-1 in I/R group was higher than that in sham group. Thus this result could demonstrate that Drp-1 participate the process of ischemic reperfusion process in MCAO model.
At the same time the Drp-1 content in both RPJEL and RPJEH group was decreased gradually, the reduction of infarction volume, they all illustrated that RPJE may involve in the antiapotosis on Drp-1. Previous studies showed that in the ischemic-reperfusion model, other related gene of apotosis like bcl-2 could also inhibit the Caspase-3 activation to protect the stabilization of mitochondria cell membrane, and then could decrease the neuron apoptosis [14].
Currently there was no evidence about the inhibition of Drp-1 in protecting the neuron. However the studies have showed that the increased Drp-1 from the neuronal cytoplasm transit to the mitochondria, and activated caspase system, much important proteins and organelles in the mitochondria were damaged, eventually mitochondrial were broken [15]. And the result of this research was the same with above, also demonstrated that Drp-1 actually participated the process of blood flow improvement.
References
- Qi W, Xiaobo L. The role of mitochondria in innate immunity and mechanism. Chinese J Immunol 2016; 6: 920-929.
- Sheng C, Xiyong X, Xingguagn Z. The effect of penehyclidine on the cytochrome and Caspase 3 expression in a acute complete cerebral ischemia-reperfusion injury in rats. J Wuhan Uni Nat Sci 2009; 1: 47-51.
- Qiushuang W, Ping C, Qingwen Z. The chemical constituents, pharmacological activity and analysis methods of Rhizoma Panacis Japonici development. Molecules 2016; 6: 46-54.
- Longa EZ, Weinstein PR, Carlson S. Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke 1989; 20: 84-91.
- Kim SS, Lee BH. Measuring cerebral hemodynamic changes during action observation with functional transcranial Doppler. J Phys Ther Sci 2015; 27: 1379-1381.
- Zhao XF, Liu YH, Han ZM, Xu YU. Effect of erythropoietin on the expression of dynamin-related protein-1 in rat renal interstitial fibrosis. Exp Ther Med 2015; 9: 2065-2071.
- Guo WC, He XF, Li YH. The effect of sequential transcatheter arterial chemoembolization (TACE) and portal venous embolizations (PVE) vs. TACE or PVE alone on rabbit VX2 liver carcinoma and on liver regeneration. Eur Rev Med Pharmacol Sci 2016; 20: 3186-3193.
- Olianas MC, Dedoni S, Onali P. Protection from interferon-β-induced neuronal apoptosis through stimulation of muscarinic acetylcholine receptors coupled to ERK1/2 activation. Br J Pharmacol 2016.
- Zuo W, Yang PF, Chen J. Drp-1, a potential therapeutic target for brain ischaemic stroke. Br J Pharmacol 2016, 173: 1665-1677.
- Jiang Q, Yu T, Huang K, Lu J, Zhang H, Hu S. Remote ischemic post-conditioning ameliorates the mesenchymal stem cells engraftment in reperfused myocardium. PLoS One 2016; 11: e0146074.
- Shimouchi A, Yokota H, Ono S. Neuroprotective effect of water-dispersible hesperetin in retinal ischemia reperfusion injury. Jpn J Ophthalmol 2016; 60: 51-61.
- Li LH, Tian XR, Hu ZP. The key target of neuroprotection after the onset of ischemic stroke: secretory pathway Ca (2+)-ATPase 1. Neural Regen Res 2015; 10: 1271-1278.
- Xiao X, Hu Y, Quiros PM, Wei Q, Lopez Otin C, Dong Z. OMA1 mediates OPA1 proteolysis and mitochondrial fragmentation in experimental models of ischemic kidney injury. Am J Physiol Renal Physiol 2014; 306: 1318-1326.
- Zhang X, Xue X, Xian L, Guo Z, Ito Y, Sun W. Potential neuroprotection of protodioscin against cerebral ischemia-reperfusion injury in rats through intervening inflammation and apoptosis. Steroids 2016; 113: 52-63.
- de Quadros T, Schramm H, Zeni EC. Developmental effects of exposure to ultraviolet B radiation on the freshwater prawn Macrobrachium olfersi: Mitochondria as a target of environmental UVB radiation. Ecotoxicol Environ Saf 2016; 132: 279-287.