Research Article - Biomedical Research (2017) Volume 28, Issue 7
The correlation study on vitamin D receptor ApaI gene polymorphism and gestational diabetes mellitus among pregnant women
Li-Ping Jin1*, Lin-Jie Shi2 and Wen-Ping Zhang3
1Department of Maternity, Peace Hospital of Changzhi Medical College, Changzhi, China
2Department of Urology, Peace Hospital of Changzhi Medical College, Changzhi, China
3Department of Cardiac Surgery, Peace Hospital of Changzhi Medical College Changzhi, China
- *Corresponding Author:
- Li-Ping Jin
Department of Maternity
Peace Hospital of Changzhi Medical College
China
Accepted date: November 26, 2016
Abstract
Purpose: The aim of this study was to explore the correlation between vitamin D receptor ApaI gene polymorphism and Gestational Diabetes Mellitus (GDM). Methods: 240 patients were divided them into GDM and non-GDM groups. DNA sampling was purified from peripheral blood and analysed by the PCR-RFLP for ApaI gene. BMI, Fasting Blood Glucose (FBG), and 1 h and 2 h Postprandial Glucose (PPG) were compared. Results: The genotype frequency of vitamin D receptor ApaI gene polymorphism significantly differed between two groups. Compared with AA genotype patients, the risk of gestational diabetes mellitus was significantly increased in those with CC genotype. Logistic regression analysis showed that there was no significant correlation between ApaI C allele and GDM. Conclusions: There was a significant correlation between vitamin D receptor ApaI gene polymorphism and GDM among pregnant women.
Keywords
Pregnant woman Vitamin D, ApaI, Gene polymorphism, Gestational diabetes mellitus
Introduction
Gestational Diabetes Mellitus (GDM) is defined as the normal glucose metabolism or potential impaired glucose tolerance before pregnancy, first discovery and diagnosis of diabetes in pregnancy. Epidemiologic study showed that its morbidity rate among pregnant woman is approximately 1%-14%, which is related to giant baby, birth injury, toxemia of pregnancy and even stillborn foetus. Typical clinical manifestations include insulin resistance, hyperglycaemia and adiposity [1-3]. The specific cause of GDM is still unclear, but inherent cause and life style play an important role in the pathogenesis and progress. It has been proposed that variants of the nuclear Vitamin D Receptor (VDR) gene are associated with a susceptibility to Type 2 Diabetes Mellitus (T2DM) and GDM. Partial genes possess polymorphism which could influence on the transcription and activity of protein. VDR is involved in the metabolism of insulin as one of the members [4]. A latest study showed that vitamin D could assist in regulating the growth, survive, inflammation of cells and the secretion of insulin. In addition, the related study also showed that there was a correlation between vitamin D deficiency, insulin resistance and the increased risk of GDM [5]. VDR gene encoding nuclear transcription factor contained four types of second gene polymorphisms with obvious characteristics: BsmI (A>G, rs1544410); ApaI (A>C, rs7975232); FokI (C N T, rs10735810) and TaqI (T>C, rs731236). The study showed that gene polymorphism of VDR was associated with the susceptibility of type I and II diabetes mellitus [6,7]. It is worth to note common features of glucose intolerance, insulin resistance and insulin secretion dysfunction between GDM and type II diabetes mellitus [8]. VDR principally mediates the anticancer activities of vitamin D. Many studies investigated the association between VDR gene ApaI polymorphism and multiple malignant tumors, but the relationship between VDR gene polymorphism and GDM susceptibility has been rarely investigated. So this study was designed to explore the correlation between vitamin D receptor ApaI gene polymorphism and GDM, aiming to provide reference and guidance for clinical diagnosis and treatment of GDM.
Materials and Methods
Baseline data
In this case-control study, all 240 patients admitted to our hospital from January, 2014 to June, 2015 were recruited. All participants divided into the GDM group (n=120) and non- GDM group (n=120). Baseline data of the patients in two groups could be found in Table 1, the diagnostic criterion of GDM was Oral Glucose Tolerance Test (OGTT) during 24-28 weeks gestation according to the standard of International Association of Diabetes and Pregnancy Study Group (IADPSG) (0 minute 5.1 mmol/l, 60 minutes 10.0 mmol/l, 120 minutes 8.5 mmol/l). It would be diagnosed as GDM when more than one glucose level exceeded a threshold value. If all plasma glucose indexes were lower than threshold values, the subjects were diagnosed as Normal Glucose Tolerance (NGT) or non-GDM.
Exclusion criteria
Patients with a medical history of diabetes mellitus, liver disease, kidney failure or functional disorder, thyroid diseases, toxemia of pregnancy, hyperandrogenism or those receiving anti-seizure and anti-depressive drugs, etc. All surgical procedures were in accordance with the ethics committee of our hospital.
The separation and gene detection of DNA
According to manufacturer's instructions, DNA purification kit (Sinaclon) of gene group was utilized for extracting DNA samples from venous blood, and then restored at-20°C. The polymorphism of vitamin D receptor was detected by using Polymerase Chain Reaction-Restriction Fragment Length Polymorphism (PCR-RFLP). With regards to the detection of VDR ApaI (A>C) polymorphism, primers were first used to amplify 745-bp fragment (forward primer: 5'- CAGAGCATGGACAGGGAGCAAG-3'; reverse primer: 5'- GCAACTCCTCATGGCTGAGGTCTCA-3'). The total PCR reactant was 25 μl, which contained 12.5 μl 2 × PCR mixture (Sinaclon), 1 ul primer (10 pmol/μl) and 1 ul DNA masterplate (100 ng/l); 30 circles (94°C for 45 seconds, 67°C for 45 seconds and then 72°C for 45 seconds), extended 10 minutes at 72°C. After PCR reaction, added 2.5 μ ApaI restricted enzyme (Fermentas) to an equivalent quantity of reaction product (10 μl) and kept reaction for 4 hours at 37°C. The genotype was defined as AA (745 bp), CC (528 and 217 bp) or CA (528, 217 and 745 bp). Processed cataphoresis for digestion products in 8% acrylamide gel on silver nitrate stained gel. The detection of serum glucose level was based on the method of glucose oxidase.
Statistical analysis
We used chi-square test to detect and analyse the differences in VDR genotype and abnormal frequency between the experimental and control groups. After adjusting age factor, logistic regression analysis was adopted to analyse Odds Ratios (ORs) of VDR genotype and 95% Confidential Interval (CIs). Biochemical data differences between two groups were analysed and compared by t-test or ANOVA. If p<0.05, then the differences had statistical significance.
Results
Baseline data
As illustrated in Table 1, baseline data of the study subjects were included in the experimental and control groups. There was no significant difference in the average age between two groups (p=0.0001). Compared with the control group, Fasting Blood Glucose detection (FBG), 1 h and 2 h PPG in the experimental group were significantly increased (all p<0.05). There was a significant increase in the risk of GDM in patients with a family history of type II diabetes mellitus (χ2=18.55, OR: 3.44, 95% CI: 1.89-6.01; p=0.001).
| Variable | Experimental group (n=120) | Control group (n=120) | P value |
|---|---|---|---|
| Age (years) | 29.54 ± 4.8 | 28.65 ± 3.89 | 0.072 |
| History of abortion | 0.35 ± 0.42 | 0.37 ± 0.35 | 0.661 |
| Family history of type II diabetes mellitus | 36.10% | 15.10% | 0.788 |
| BMI (kg/m2) | 29.63 ± 5.87 | 24.87 ± 4.21 | 0.001 |
| FBG (mg/dl) | 111.3 ± 29.3 | 81.2 ± 8.3 | 0.001 |
| 1 h PPG (mg/dl) | 170.5 ± 36.6 | 126.5 ± 29.7 | 0.001 |
| 2 h PPG (mg/dl) | 143.2 ± 36.4 | 99.5 ± 25.2 | 0.001 |
| Note: FBG: Fasting Blood Glucose Detection; PPG: Postprandial Glucose. | |||
Table 1: Baseline data of study subjects between two groups.
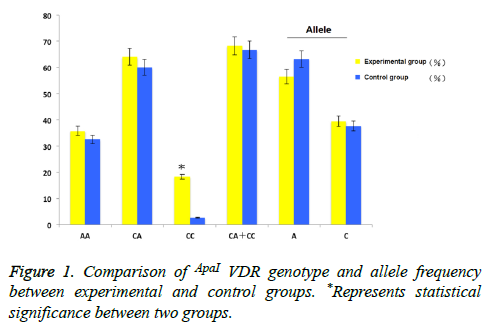
Correlation analysis between genotype and allele frequency
As demonstrated in Figure 1, showed the differences in VDR ApaI polymorphic genotype and allele frequency of two groups. There were significant differences in the genotype frequencies of ApaI VDR polymorphism between the two groups (χ2=8.2, p=0.013, Df=2). And CC genotype was more popular in the experimental group, the differences were obvious (18.3% vs. 2.7%, p=0.007). AA genotype was regarded as the reference, the GDM risk of the patients with CC genotype was higher (AA vs. CC, OR=2.876, 95% CI=1.245-8.117, P=0.006). Whereas there was no obvious correlation between other genotypes or combined genotypes (AA vs. CA, OR=0.933, 95% CI=0.538-1.663, P=0.6; AA vs. (CA+CC), OR=1.258, 95% CI=0.654-1.874, p=0.71). There was no significant difference in allele frequencies between two groups (χ2=2.39, p=0.16).
Logistic regression analysis showed no significant interaction between C ApaI allele and the risk of GDM. We further analysed the relationship between individual genotypes of VDR gene, population distribution and biochemical characteristics. The results showed there was no significant correlation (Table 2).
| ApaI | Experimental group | Control group | OR (95% CI) | χ2 |
|---|---|---|---|---|
| C | n (%) | n (%) | ||
| - | 14 (11.7) | 16 (7.3) | Reference | Reference |
| + | 70 (58.3) | 47 (39.2) | 1.47 (0.5-3.9, P=0.28) | 0.8 (df=1, P=0.42) |
| - | 41 (34.1) | 40 (33.3) | 0.94 (0.7-1.6, P=0.87) | 0.06 (df=1, P=0.77) |
| + | 45 (37.5) | 62 (28.2) | 0.85 (0.6-1.4, P=0.39) | 0.7 (df=1, P=0.42) |
Table 2: Logistic regression analysis of the correlation between Apal C allele genes and GDM risk between two groups.
Discussion
More and more attention should be paid to the research on common genetic variants of vitamin D receptor gene in diabetes mellitus, GDM and other diseases [4,9-11]. In this study, we mainly explored the correlation between ApaI VDR gene polymorphism and GDM and found there was a significant difference in genotype distribution between GDM and non-GDM counterparts. The comparison between CC and AA genotypes was more common. It was found that VDR ApaI allele polymorphism was associated with the incidence of GDM in this population. There was no significant difference in allele genes in the susceptibility of GDM between the experimental and control groups.
In current study, the relationship between the polymorphism of VDR gene and GDM has been rarely investigated [12-14]. Ghamdi et al. reported that there was a certain correlation between VDR Taql polymorphism and GDM. Aslandi et al. found that there was a significant correlation between the Fokl VDR polymorphism and the risk of GDM among Iran population. Tawfeek et al. reported that there was a significant correlation between VDR Bsml polymorphism and the risk of GDM. The correlation between the ApaI gene polymorphism and GDM has not been reported.
VDR is a nuclear factor which can mediate physiological metabolic activity of a majority of vitamin D. Vitamin D plays a role by regulating the level of extracellular calcium in beta cells, and promotes the secretion of insulin. Similar to type II diabetes mellitus, typical features of GDM include insulin resistance and related functional activity damage in target organ tissues. The latest study showed that there was a certain correlation between vitamin D and cancer, disseminated sclerosis, asthma and diabetes mellitus, etc. [15-18]. Multiple epidemiologic studies detected serum vitamin D level in GDM and non-GDM population, and found that there was a certain correlation between vitamin D deficiency and the incidence of GDM [19].
Meantime, some evidences showed partial risk factors which coexist in both GDM and type II diabetes mellitus patients, such as genetic risk, etc. [20-22]. A meta-analysis study demonstrated that eight genes associated with type II diabetes mellitus are correlated with GDM susceptibility. Several scholars have detected a partial correlation between VDR gene polymorphism and the susceptibility of diabetes mellitus. Nosratabadi et al. reported that Taql polymorphism in Iran population was associated with the morbidity of type II diabetes mellitus. Oh et al. also found a significant correlation between ApaI polymorphism and type II diabetes mellitus in American population (p=0.058) [23]. Wang et al. conducted a meta-analysis study and reported that Bsml polymorphism was associated with type I diabetes mellitus in Asian population, whereas Fokl polymorphism was related to type II diabetes mellitus [24]. Bonakdaran et al. reported the effect of BsmI, FokI, VDR ApaI and TaqI gene polymorphisms on patients with type I diabetes mellitus and they found the genotype frequency of AA, FF and Bb was significantly increased. Mohammadnejad et al. found that VDR Taql gene polymorphism was significantly associated with type I diabetes mellitus [25]. Bilge et al. evaluated the insulin resistance and quality of life in obese subjects and non-obese counterparts and demonstrated that it would be a rational approach to identify routine serum 25 (OH) D levels of obese patients and administer a treatment to patients with a low level of vitamin D [26]. Obesity might be one of the risk factors of the incidence of GDM. In this study, we found the average BMI of GDM patients was obviously higher than that of the normal controls. Hence, further research was urgently needed to confirm the conclusion. In this study, we only detected VDR ApaI polymorphism and the sample size included in the study was relatively limited. In conclusion, there was a significant correlation between vitamin D receptor ApaI gene polymorphism and GDM among pregnant women.
References
- Rahmannezhad G, Mashayekhi FJ, Goodarzi MT, Rezvanfar MR, Sadeghi A. Association between vitamin D receptor ApaI and TaqI gene polymorphisms and gestational diabetes mellitus in an Iranian pregnant women population. Gene 2016; 581: 43.
- Al-Shoumer KA, Al-Essa TM. Is there a relationship between vitamin D with insulin resistance and diabetes mellitus? World J Diabetes 2015; 6: 1057-1064.
- Aslani S, Hossein-Nezhad A, Mirzaei K, Maghbooli Z, Afshar AN. VDR FokI polymorphism and its potential role in the pathogenesis of gestational diabetes mellitus and its complications. Gynecol Endocrinol 2011; 27: 1055-1060.
- Ben-Haroush A, Yogev Y, Hod M. Epidemiology of gestational diabetes mellitus and its association with Type 2 diabetes. Diabet Med 2004; 21: 103-113.
- Zhang MX, Pan GT, Guo JF, Li BY, Qin LQ, Zhang ZL. Vitamin D deficiency increases the risk of gestational diabetes mellitus: A meta-analysis of observational studies. Nutrients 2015; 7: 8366.
- Gur EB, Karadeniz M, Genc M, Eskicioglu F, Yalcin M. Relationship between mean platelet volume and vitamin D deficiency in gestational diabetes mellitus. Arch Endocrinol Metab 2015; 59: 448-454.
- Pleskaatova A, Bartakova V, Pacal L, Kuricova K, Balobradkova J. Vitamin D status in women with gestational diabetes mellitus during pregnancy and postpartum. Biomed Res Int 2015; 2015: 260624.
- Díaz L, Diaz-Munoz M, Garcia-Gaytan AC, Mendez I. Mechanistic effects of calcitriol in cancer biology. Nutrients 2015; 7: 5020-5050.
- Dilmec F, Uzer E, Akkafa F, Kose E, van Kuilenburg AB. Detection of VDR gene ApaI and TaqI polymorphisms in patients with type 2 diabetes mellitus using PCR-RFLP method in a Turkish population. J Diabetes Complications 2010; 24: 186-191.
- Duman NB. Frequency of gestational diabetes mellitus and the associated risk factors. Pak J Med Sci 2015; 31: 194-197.
- Goral A, Brola W, Kasprzyk M, Przybylski W. The role of vitamin D in the pathogenesis and course of multiple sclerosis. Wiad Lek 2015; 68: 60-66.
- Kendrick JM. Screening and diagnosing gestational diabetes mellitus revisited: implications from HAPO. J Perinat Neonatal Nurs 2011; 25: 226-233.
- Hartling L, Dryden DM, Guthrie A, Muise M, Vandermeer B. Screening and diagnosing gestational diabetes mellitus. Evid Rep Technol Assess (Full Rep) 2012; 1-327.
- Haussler MR, Jurutka PW, Mizwicki M, Norman AW. Vitamin D receptor (VDR)-mediated actions of 1 ± 25 (OH) vitamin D: genomic and non-genomic mechanisms. Best Pract Res Clin Endocrinol Metab 2011; 25: 543-559.
- Hossein-Nezhad A, Maghbooli Z, Vassigh AR, Larijani B. Prevalence of gestational diabetes mellitus and pregnancy outcomes in Iranian women. Taiwan J Obstet Gynecol 2007; 46: 236-241.
- Huerta-Chagoya A, Vazquez-Cardenas P, Moreno-Macias H, Tapia-Maruri L, Rodríguez-Guillen R, Lopez-Vite E. Genetic determinants for gestational diabetes mellitus and related metabolic traits in Mexican women. PLoS One 2015; 10: e126408.
- Jain R, von Hurst PR, Stonehouse W, Love DR, Higgins CM. Association of vitamin D receptor gene polymorphisms with insulin resistance and response to vitamin D. Metabolism 2012; 61: 293-301.
- Kerley CP, Elnazir B, Faul J, Cormican L. Vitamin D as an adjunctive therapy in asthma. Part 2: A review of human studies. Pulm Pharmacol Ther 2015; 32: 75.
- Khan IA, Movva S, Shaik NA, Chava S, Jahan P. Investigation of Calpain 10 (rs2975760) gene polymorphism in Asian Indians with gestational diabetes mellitus. Meta Gene 2014; 2: 299-306.
- Kirwan JP, Hauguel-De Mouzon S, Lepercq J, Challier JC, Huston-Presley L. TNF-alpha is a predictor of insulin resistance in human pregnancy. Diabetes 2002; 51: 2207-2213.
- Maghbooli Z, Hossein-Nezhad A, Karimi F, Shafaei AR, Larijani B. Correlation between vitamin D3 deficiency and insulin resistance in pregnancy. Diabetes Metab Res Rev 2008; 24: 27-32.
- Malecki MT, Frey J, Moczulski D, Klupa T, Kozek E. Vitamin D receptor gene polymorphisms and association with type 2 diabetes mellitus in a Polish population. Exp Clin Endocrinol Diabetes 2003; 111: 505-509.
- Oh JY, Barrett-Connor E. Association between vitamin D receptor polymorphism and type 2 diabetes or metabolic syndrome in community-dwelling older adults: the Rancho Bernardo Study. Metabolism 2002; 51: 356.
- Wang Q, Xi B, Reilly KH, Liu M, Fu M. Quantitative assessment of the associations between four polymorphisms (FokI, ApaI, BsmI, TaqI) of vitamin D receptor gene and risk of diabetes mellitus. Mol Biol Rep 2012; 39: 9405-9414.
- Mohammadnejad Z, Ghanbari M, Ganjali R, Afshari JT, Heydarpour M. Association between vitamin D receptor gene polymorphisms and type 1 diabetes mellitus in Iranian population. Mol Biol Rep 2012; 39: 831-837.
- Bilge U, Unalacak M, Unluoglu I, Ipek M, Celer O, Akalm A. Relationship between 1, 25 dihydroxy vitamin D levels and homeostatic model assessment insulin resistance values in obese subjects. Nig J Clin Pract 2015; 18: 377-380.