Research Article - Biomedical Research (2017) Volume 28, Issue 11
The correlation between tissue Helicobacter pylori severity and the increase in serum neutrophil/lymphocyte ratio in patients with active chronic gastritis
Yahya Atayan1* and Hacisalihoglu P2
1Department of Gastroenterology, Gümüşhane State Hospital, 29100 Gümüşhane, Turkey
2Department of Pathology, Medical Faculty, Yeni Yüzyıl University, Gaziosmanpaşa Hospital, Turkey
Accepted on March 27, 2017
Abstract
Introduction: Helicobacter pylori are a microaerophile gram-negative bacteria and the most frequent factor of chronic gastritis. Recently, there has been an inclination to various non-invasive tests to determine the severity of H. pylori infection in the gastric tissue. The serum neutrophils/lymphocytes rate (NLR) is a simple, safe, non-invasive and active inflammation reagent. The purpose of this study is examining the correlation between the increase in the positivity/severity of H. pylori infection and the increase in the NLR.
Material and Method: 149 patients were included into the study by considering the Sydney criteria in accordance with H. pylori severity degrees in 3 groups; Mild (n=49), Moderate-Severe (n=67) and Severe (n=33). A Control Group was also formed (n=22) with negative H. pylori by three experienced pathologists.
Result: It has been determined that the severity has increased among the groups with H. pylori positive as regard to the increase in serum NLR (r: 0.295, p: 0.017), there has been a significant correlation has been determined between the Control Group and the Moderate-Severe patients (p:0.014), the Severe patients (p:0.002).
Conclusion: It is suggested that the serum NLR, which can be used in order to predict the severity of the H. pylori Infection in patients with chronic gastritis, can be a practical, inexpensive and non-invasive test.
Keywords
Helicobacter pylori, Serum neutrophils/lymphocytes rate, Chronic gastritis
Introduction
Currently H. pylori infection is prevalent in 50% of the world’s population [1]. Chronic gastritis associated with H. pylori infection is characterized histologically by the presence of lymphoid follicle hyperplasia, intestinal metaplasia and neutrophil infiltration to the lamina propria in varying degrees [2]. According to the Sydney Gastritis Classification System, the increase in neutrophil predominant inflammatory cells represents acute gastritis, while the increase in chronic inflammatory cells (lymphocytes and plasmacytes) represents chronic gastritis [3]. Due to the fact that Sydney Gastritis Classification System requires an invasive procedure, there is an inclination to various non-invasive tests in order to predict the severity of H. pylori infection. Serum neutrophil/ lymphocyte ratio (NLR) is a simple, safe, relatively noninvasive acute inflammation marker [4]. The aim of our study is to determine the correlation between the severity of H. pylori infection and active and chronic gastritis, and the increase in serum NLR in patients with chronic H. pylori gastritis.
Materials and Methods
We retrospectively reevaluated the histories, the complete blood count (CBC) test results and the pathology reports of 450 patients who had undergone gastroscopic examination due to dyspeptic complaints in our gastroenterology unit between 2014 and 2015. The endoscopic biopsies were taken from the gastric antrum by an experienced gastroenterologist and were interpreted by an experienced pathologist. Severity of active and chronic gastritis and H. pylori infection were scored using a 3 scale scoring system as “mild, moderate and severe” according to the Sydney Gastritis Classification System. Glandular atrophy and intestinal metaplasia were also noted in the pathology reports. 149 patients with active, chronic H. pylori gastritis without any other concomitant inflammatory disorders were included in our study. A control group consisting of 22 subjects with dyspeptic complaints who had undergone gastroscopic biopsy was also included. The subjects in the control group had no histopathologically determined H. pylori infection or gastritis nor did they have any other known inflammatory disorders. The serum NLRs of the 171 patients enrolled in our study were calculated according to the results of the CBC tests performed prior to the gastroscopic biopsy procedures. Using the SPSS 17 program, the Pearson Correlation Rates were performed and the statistical analysis of the patient and control groups was compared.
Results
Eighty (47.6%) of the 171 patients were male, and 91 (53.3%) were female. The average age of the male patients was 58, the female patients was 50. According to the histopathological examination, the gastritis activity score of 50 patients (33.6%) was determined to be mild, whereas that of 63 patients (42.3%) were moderate, and of 36 patients (24.2%) were severe. The severity of the H. pylori infection was determined to be mild in 49 patients (32.9%), whereas 67 patients (45%) were moderately, 33 patients (22.1%) were severely infected by H. pylori Forty patients (26.8%) had mild, 75 patients (50.3%) had moderate and 34 patients (22.8%) had severe chronic gastritis.
The control group consisted of 22 subjects with dyspeptic symptoms who had undergone gastroscopic examination and biopsy and revealed no active, chronic gastritis or H. pylori infection according to the histopathological interpretation. The mean serum NLR value of the patients who were mildly infected by H. pylori was 1.55. This rate was 2.04 in moderately infected patients, 2.15 in severely infected patients and 1.52 in the control group (Table 1). Our study determined a correlation between the increase in the severity of tissue H. pylori positivity (mild, moderate and severe) and the increase in serum NLRs of the patients (r:0.295, p:0.017, Table 2). There was no significant correlation between the increase in the serum NLRs of the control group and the mildly infected patients (p:0.3) however, we determined a statistically significant correlation between the increase in serum NLRs of the control group and the patients who were moderately and severely infected by H. pylori (p:0.014, p:0.002, respectively). We also determined a statistically significant correlation between the severity of H. pylori infection and gastritis activity and the chronicity scores of the patients in our study (r:0.309, r:0.226, p:0.0005, p:0.006, respectively) (Table 2).
| Patient groups | The number of patients | Mean NLR | Minimum | Maximum |
|---|---|---|---|---|
| Mild H. pylori infection | 49 | 1.5578 | 0.60 | 2.38 |
| Moderate H. pylori infection | 67 | 2.0458 | 0.70 | 4.9 |
| Severe H. pylori infection | 33 | 2.1512 | 1.00 | 5.6 |
| Control group (not infected with H. pylori ) | 22 | 1.5202 | 0.7 | 2.24 |
| H. pylori: Helicobacter pylori NLR: Neutrophil/lymphocyte ratio |
||||
Table 1. The correlation between the severity of H. pylori infection and serum NLRs of the active, chronic gastritis patients and the control group.
| Patient groups | Severity of H. pylori infection | Severity of active gastritis | Severity of chronic gastritis | Increase in serum NLR values | |
|---|---|---|---|---|---|
| H. pylori infection n: 149 |
P. Correlation (r) | - | 0.309 | 0.226 | 0.295 |
| p value | - | 0.0005 | 0.006 | 0.017 | |
| Active gastritis n: 149 |
P. Correlation(r) | 0.309 | - | 0.385 | -0.154 |
| p value | 0.0005 | - | 0.0005 | 0.061 | |
| Chronic gastritis n:149 |
P. Correlation(r) | 0.226 | 0.386 | - | -0.037 |
| p value | 0.006 | 0.0005 | - | 0.653 | |
| P. Correlation: Pearson correlation NLR: Neutrophil/lymphocyte ratio |
|||||
Table 2. The correlation between gastritis activity, chronicity scores, the severity of H. pylori infection and the increase in serum NLRs of the patients.
Discussion
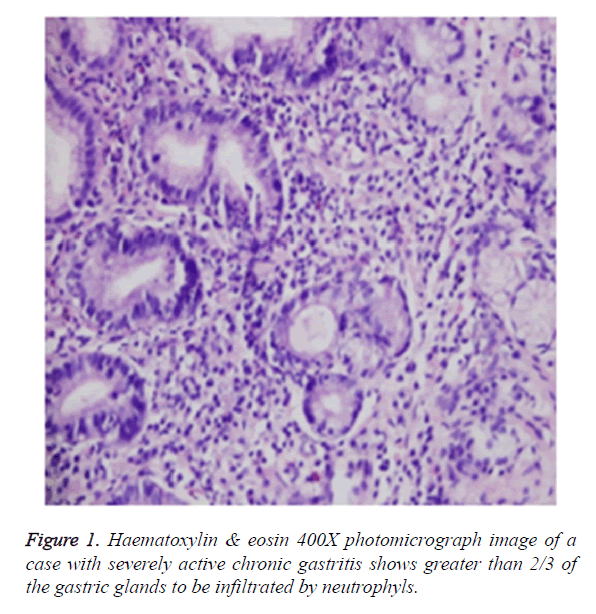
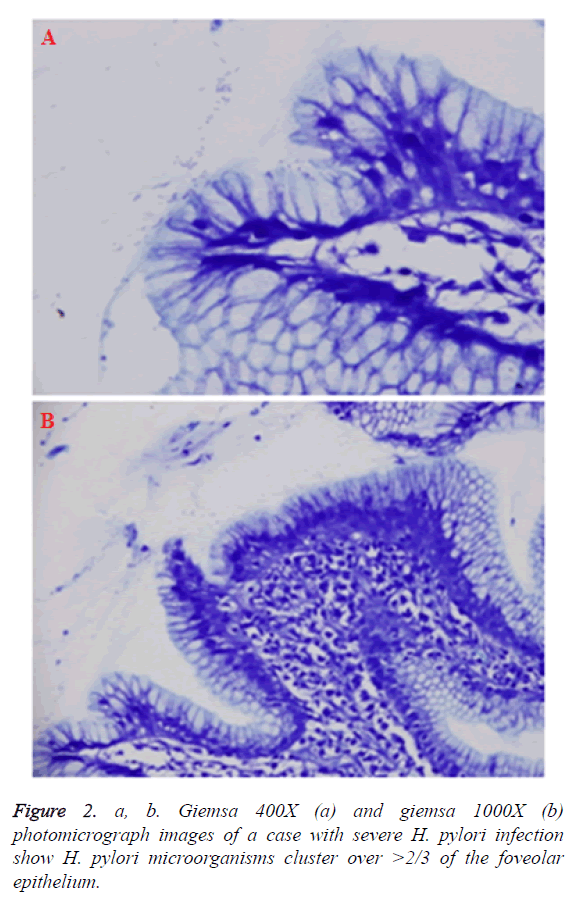
H. pylori is a microaerophilic gram-negative bacteria and the most common human pathogen in our century. It has been determined to be colonized in almost half of the world’s population [1]. H. pylori is the most common etiologic factor of chronic gastritis [5]. The bacteria have a predilection for the gastric antral mucosa because it can reproduce more easily in the mucus secreting areas of the stomach. H. pylori has virulence factors which play a role in the pathogenesis of the infection, such as kinase inhibitors, which also take part in the loss of polarity and elongation in the gastric epithelial cells. Additionally, proinflammatory cytokines are released, resulting the activation of neutrophils which play a major role in the active inflammation [6,7]. While neutrophils play a role in the active inflammation in acute gastritis; lymphocytes and plasma cells accompany the inflammatory process in chronic gastritis [8]. According to the Sydney Gastritis Classification and Rating System, the severity of the inflammatory activity in acute gastritis is assessed by the infiltration of neutrophils into the gastric crypts, and the severity of chronic inflammation is determined by the infiltration of lymphocytes into the lamina propria.
The severity of H. pylori infection is assessed by the infiltration of the microorganisms in the gastric foveolar epithelium [3]. In our study, the severity of H. pylori infection is scored by a triple scale as “mild, moderate and severe”, according to the Sydney Gastritis Classification System (Figures 1 and 2). In a study of Stolte et al. [9], conducted with 240 patients with chronic H. pylori gastritis, a statistically significant correlation is determined between the increase in the tissue H. pylori colonization and activity of gastritis. In a study of Duarte et al. [10], including 261 patients with chronic gastritis, it was determined that there was a significant correlation between the severity of H. pylori colonization and chronic inflammation. Additionally, in another study, Faigel et al. [11], stated that the presence of acute and/or chronic gastritis is correlated with the presence of H. pylori in gastric antral mucosal tissue. Similarly, in a study conducted by Fareed et al. [12], among 150 patients with chronic gastritis, it was reported that there was a significant correlation between the tissue H. pylori intensity and neutrophil activity. In another study, Tanka et al. [13], determined that the intensity of H. pylori colonization is significantly correlated with the neutrophil activity and chronic inflammation. In our study, consistent with the literature, we determined that there is a statistically significant correlation between the severity of H. pylori infection and the severity of active and chronic gastritis (r: 0.309, 0.226; p: 0.0005, 0.006, respectively) (Table 2).
Due to the fact that Sydney Gastritis Classification System is associated with an invasive procedure, in recents studies, relatively non-invasive tests have started to be used to determine the severity of H. pylori infection in gastritis patients. In previous years, Karttunen et al. [14], stated that mucosal inflammation due to H. pylori infection is reflected in the amount of peripheral blood leucocytes. In 2004, serum NLR is determined to be an economic, relatively non-invasive acute inflammation marker by Avanzas et al. for the first time, in acute myocardial infarction patients [4]. Later on, in 2014, in a study conducted by Farah et al. [15], it was determined that there was a statistically significant difference between the serum NLRs of the patients with chronic H. pylori gastritis detected by urea breath test and the gastritis patients without H. pylori infection. Jafarzadeh et al. [16], stated that elevated serum leucocyte counts and NLR can be a marker of inflammation and infection among H. pylori infected peptic ulcer patients. The authors found a significant difference between the mean serum neutrophil count and serum NLRs of the peptic ulcer patients infected by H. pylori and the H. pylori negative control group.
In our study, in consistence with the literature, we determined a statistically significant correlation between the severity of H. pylori infection in mild and moderately scored patient groups, and the increase in their serum NLRs (r:0.295, p:0.017, Table 1) however, we did not find a significant difference in the increase in serum NLRs between the patients who had moderate and severe H. pylori infection. Similarly, in terms of increase in serum NLR, we found no significant difference between the mildly infected patients and the control group but we determined a significant difference between that of the patients with moderate and severe H. pylori infection and the control group. (p:0.3, p:0.014, p:0.002 respectively). As a conclusion of our study, we suggest that serum NLR may be used to predict the severity of H. pylori infection in patients with chronic gastritis during and at the end of the therapy periods and it can be a practical, safe, inexpensive and a relatively non-invasive method.
References
- Haghazali M, Molaei M, Mashayekhi R, Zojaji H, Pourhoseingholi MA, Shooshtarizadeh T, Mirsattari D, Zali MR. Proinflammatory cytokines and thrombomodulin in patients with peptic ulcer disease and gastric cancer, infected with Helicobacter pylori. Indian J Pathol Microbiol 2011; 54: 103-106.
- Bodger K, Wyatt JI, Heatley RV. Gastric mucosal secretion of interleukin-10: relations to histopathology, Helicobacter pylori status, and tumour necrosis factor alfa secretion. Gut 1997; 40: 739-744.
- Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol 1996; 20: 1161-1181.
- Avanzas P, Quiles J, López de Sá E, Sánchez A, Rubio R, García E, López-Sendón JL. Neutrophil count and infarct size in patients with acute myocardial infarction. Int J Cardiol 2004; 97: 155-156.
- Liu J, He L H, Aesebrouck F. Prevalence of Coinfection with Gastric Non-Helicobacter pylori Helicobacter (NHPH) Species in Helicobacter pylori-infected Patients Suffering from Gastric Disease in Beijing, China. Helicobacter 2015; 20: 284-290.
- McGee DJ, Mobley HL. Pathogenesis of Helicobacter pylori infection. Curr Opin Gastroenterol 2000; 16: 24-31.
- Yamaoka Y. Mechanisms of disease: Helicobacter pylori virulence factors. Nature Rev Gastroenterol Hepatol 2010; 7: 629-641.
- Lee EL, Feldman M. Gastritis and Gastropathies. Sleisenger and Fordran’s Gastrointestinal and Liver Disease. Pathophysiology/Diagnosis/Management. Saunders Elsevier. 2006; 1: 1067-1088.
- Stolte M, Stadelmann O, Bethke B, Burkard G. Relationships between the degree of Helicobacter pylori colonisation and the degree and activity of gastritis, surface epithelial degeneration and mucus secretion. Z Gastroenterol 1995; 33: 89-93.
- Duarte I, Schultz M, Chianale J, Bravo R. Semiquantitative histopathologic analysis of chronic gastritis: extension and grading score. Rev Med Chil 1996; 124: 1200-1206.
- Faigel DO, Furth EE, Childs M, Goin J, Metz DC. Histological predictors of active Helicobacter pylori infection. Dig Dis Sci 1996; 41: 937-943.
- Fareed R, Abbas Z, Shah MA. Effect of Helicobacter pylori density on inflammatory activity in stomach. J Pak Med Assoc 2000; 50: 148-151.
- Tanko MN, Manasseh AN, Echejoh GO. Relation between Helicobacter pylori, inflammatory (neutrophil) activity, chronic gastritis, gastric atrophy and intestinal metaplasia. Niger J Clin Pract 2008; 11: 270-274.
- Karttunen TJ, Niemelä S, Kerola T. Blood leukocyte differential in Helicobacter pylori infection. Dig Dis Sci 1996; 41: 1332-1336.
- Farah R, Khamisy FR. Association of Neutrophil to Lymphocyte Ratio With Presence and Severity of Gastritis Due to Helicobacter pylori Infection. J Clin Lab Anal 2014; 28: 219-223.
- Jafarzadeh A, Akbarpoor V, Nabizadeh M, Nemati M, Rezayati MT. Total leukocyte counts and neutrophil-lymphocyte count ratios among Helicobacter pylori-infected patients with peptic ulcers: independent of bacterial CagA status. Southeast Asian J Trop Med Public Health 2013; 44: 82-88.