Research Article - Current Pediatric Research (2024) Volume 28, Issue 6
Sub-optimal breastfeeding practices among women having 24-59 months age children in Dessie Zuria Woreda, Northwest Ethiopia
Muluken Genetu Chanie1, Wolde Melese Ayele2, Asnakew Molla Mekonen1*, Yitayish Diamtie3
1Department of Health Systems and Policy, School of Public Health, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
2Departments of Epidemiology and Biostatistics, School of Public Health, College of Medicine and Health Sciences, Injibara University, Injibara, Ethiopia
3Department of Reproductive and Family Health, School of Public Health, College of Medicine and Health Sciences, Injibara University, Injibara, Ethiopia
- Corresponding Author:
- Asnakew Molla Mekonen
Department of Health systems and Policy,
Wollo University,
Dessie,
Ethiopia
E-mail: amdessie2007@gmail.com
Received: 26-Jun-2023, Manuscript No. AAJCP-23-103967; Editor assigned: 28-Jun-2023, AAJCP-23-103967 (PQ); Reviewed: 12-Jul-2023, QC No. AAJCP-23-103967; Revised: 25-Aug-2023, Manuscript No. AAJCP-23-103967 (R); Published: 01-Sep-2023, DOI:10.35841/0971-9032.27.9.1988-1995
Abstract
Background: Sub-optimal breastfeeding practice is a very important contributor to new born and young child mortality in developing world including Ethiopia. Early and rapid quiting of breastfeeding, then by a commencement of unclean, unsound formula provision of children with very light milk contents is familiar in LMICs which results thousands of infant death. This study focused on assessing sub-optimal breastfeeding practice and determinant factors among women having 24-59 months age child in Dessie Zuria woreda, Northwest Ethiopia.
Methods: A community based cross-sectional study design was carried out from October 21 to November 25, 2019 in Dessie Zuria woreda data collected from a sample of 346 respondents using simple random sampling technique to select participants of the study. Binary and multivariable logistic regression model was used to identify predictors of suboptimal breast feeding practice using AOR with P-value <0.05 and at 95% CI.
Result: Three hundred forty six participants completed the questionnaire making the response rate 98%. The overall suboptimal breastfeeding was found 46.3% at 95% CI (42.3%-50.7%). Maternal illiteracy level, number of ANC visit, use of radio and counselling during ANC visit were found preventive factors for sub-optimal breast feeding practice in the study area.
Conclusion: The prevalence of sub-optimal breast feeding was found high magnitude. Four predictor variables that possibly reduce sub-optimal breastfeeding practice which demands an intervention by the policy makers, health care managers and health workers at each level of the health system.
Keywords
Sub-optimal, Children, Breastfeeding, 24-59 months, Dessie Zuria, Ethiopia wound management
Abbreviations:
ANC: Antenatal Care; BF/EBF: Breastfeeding/Exclusive Breastfeeding, GO: Governmental Organization; HE: Health Education; NGO: Non-Governmental Organization; WHO: World Health Organization
Introduction
Suboptimal breastfeeding practices refer to any behaviours or habits that may interfere with a mother's ability to provide her baby with the best possible nutrition. These practices include not breastfeeding exclusively, using a bottle too soon, not latching on correctly, not breastfeeding on demand or not breastfeeding for a long enough duration. All of these practices can lead to decreased nutrient intake for the baby, leading to poor growth and development [1-3] and as a result it is responsible for 45% of neonatal infectious deaths in the world, 30% of diarrheal based mortality and 18% of ARIs deaths [4,5].
WHO recommends that children should commence BF within 1 hour of delivery and be exclusively breastfed for the 1st 6 months of age, with timely start of optimal, clean and appropriate complementary foods while sustaining breastfeeding for up to 2 years of life or further [6,7].
Non optimal BF practice is identified from the predominant reason child malnutrition in Ethiopia that indicated in studies is only around half (52%) of the infants less than six months old were exclusively breastfed [8-10]. This practice is associated with higher rates of acquisition of infections like GIT, ARI diseases and conditions. Despite its obvious benefits, EBF duration in many countries including Ethiopia is lower than the international recommendation of exclusive breastfeeding for the first six months of life, especially in urban areas [11,12].
BF provides numerous health benefits through promoting and protecting maternal and child health from several infections. Optimal breastfeeding is one of the very crucial components of child health but ineffectively practiced leading to exposure of diarrheal and respiratory diseases which may kill the child [13]. Globally, sixty percent of the infants and young child mortality happened because of child feeding problems and where 2/3 of these deaths are attributed to sub-optimal breastfeeding actions. These action have a detrimental effect on the child health and development, specifically in LMICs the accessibility and availability of essential health service is not properly established. In Ethiopia, 57% of under five children death is associated with malnutrition primarily as a result of hunger, poor family and low health care access. Malnourished child that can survive are more frequently get sick and attacked the life-long effects of developmental problems. Child feeding is a complex issue that has implications on nutritional, health, psychological and developmental issues.
According to WHO, EBF mean the practice of breast milk feeding alone (including expressed breast milk) and no other liquids or solids with the exception of drops or syrups consisting of vitamins, mineral supplements or medicine. Globally, several complex interactions of socio-cultural outlooks targeting on the standards of child feeding strategies are observed. The problem between infant BF views and the WHO recommendations is widening in LMICs where sociocultural, economic and traditional norms have significant effects on BF and infant caring practices. Early and fast stopping of breastfeeding, and then replacing by a start of untidy, unsound formula feeding of children with very light milk content is common in LMICs. This is why; under five children are highly susceptible to infections for the variety of agents since their body nutrient store is not well developed [14]. Evidences showed that traditional and cultural ways of life related to child feeding have bad effects on the practice of breastfeeding recommended in LMICs. In some societies, water, butter and other food contents are given for neonates, while colostrum is avoided as dirty milk, assuming to start BF when the milk becomes clearer after a few days of fore coming milk removal hoping this practice as a preventive measure of neonates against diseases. Globally, less than 35% of mothers give EBF to their child during the first months of life and the problem is widely rising in SSC [15]. The Ethiopian Demographic and Health Surveys (EDHS 2005, 2016) data showed that 96% of <5 children (urban and rural), have ever been breastfed in their lives; however, it was found not optimal. Although, in Ethiopia, 69.1% of neonates are given breast milk within one hour of birth and less than 80% of two months old infants are put on EBF, this proportion rapidly falls to 38% at the age of six months [16].
Even though optimal breastfeeding is one of the targets of Primary Health Care (PHC) initiatives of Ethiopia, a wide range of cultural infant feeding practices are seen and documented even after the implementations of IYCF recommendations.
Actions to protect, promote and support EBF are demanded at the national, health facility and community levels. This study was aimed to determine the magnitude of suboptimal breastfeeding practices and the potential factors attributed to the practice among women having 24-59 months age children in Dessie Zuria woreda.
Materials and Methods
Study setting and period: The study was conducted in Dessie Zuria district, South Wollo zone, Ethiopia. The district is located around 480 Km from Bahirdar, the seat of Amhara region and 401 Km from Addis Ababa, the capital city of Ethiopia, to the North direction.
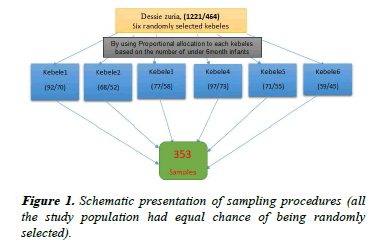
The district is established with 26 Kebeles. There are 6 health centers and 27 health posts intended to provide health services to the population in this district. Total population of the district was 62,230 where 29,440 were females and from the females 13,419 women were in the reproductive age group. There are 1,972 under five children, where 1,221 children were from 24-59 months age who was the target population of this study with their mothers/caregivers. This study was conducted from October 21 to November 25, 2019.
Study design and population: In this study community based cross-sectional study design. All mothers who had children of age between 24-59 were considered as a source population, but those children whose age 24-59 months in those randomly selected six kebeles of Dessie Zuria district were used as a study population for this study duration.
Inclusion and exclusion criteria: All mothers having 24-59 months age children during the study period were included for the data collection while mothers who are on exclusive complementary feeding, mothers living with HIV and feeding their child in ways mixed or complementary feeding were excluded.
Sample size determination and sampling technique: The sample size for the descriptive objective was calculated using single population proportion formula considering the following assumptions: Proportion of suboptimal breast feeding (P=29.8%) (1), expected margin of error (d) of 0.05, at 95% confidence level (Zα/2) and 10% contingency for non-response rate.
Thus, n=((Zα/2)2 × P(1-P))/d2 n=((1.96)2 × (0.298)× (0.702))/(0.05)2 =321
So, by adding 10% for non-respondents the calculated sample size was=353
For factors of suboptimal breast feeding the sample size was determined by using double population proportion formula using selected three key predictors (2, 3) according to the following assumptions and computed by Epi-info version 7 software (Table 1).
| S. no | Factors | Assumptions | Final sample size |
|---|---|---|---|
| 1 | Educational status | Odds Ratio=2.86, ratio 1:1, power =80%, at 95% confidence level and 10% for non-response rate | 323 |
| 2 | Antenatal care | Odds Ratio=1.75, ratio 1:1, power =80%, at 95% confidence level and 10% for non-response rate | 293 |
| 3 | Income | Odds Ratio=2.589, ratio 1:1, power =80%, at 95% confidence level and 10% for non-response rate | 178 |
Table 1. Determination of sample size for the factors of suboptimal breast feeding practice among women having 24-59 months age children using Epi-Info software v.7 in Dessie Zuria Woreda, South Wollo, Northeast Ethiopia, 2019.
Finally, the minimum adequate sample size for this specific study was 353 participants taken from the sample size determined in the first objective.
A simple random sampling technique was applied after taking all registered mothers from health posts that have children age 24-59 months from local health extension workers, for each kebele as shown below (Figure 1).
Study variables
The outcome variable for this study was sub-optimal breastfeeding practice (Suboptimal/Optimal) while the independent variables used were thematized in the following as Socio-demographic factors, maternal related factors, breastfeeding practices and maternal knowledge and attitude related factors.
Operational definitions
Early initiation of breastfeeding: The proportion of children 24-59 months of age who were put to the breast within one hour of birth.
Exclusive breastfeeding: The proportion of children 24-59 months of age who received breast milk as the only source of nourishment (but allows oral rehydration solution, drops or syrups of vitamins and medicines) during their infancy upon six months of age.
Suboptimal breast feeding: Is the practice of breastfeeding of infants/children below the WHO recommendation level per day. It was measured using the WHO tools on those concepts: Early initiation of breastfeeding, EBF, continuity of BF upon 24 months of child age. Finally, this was dichotomized to suboptimal breastfeeding practices and not.
Data collection tools, quality control and analysis
Participant administered structured questionnaires were developed from different literatures to collect data on suboptimal breast feeding practices and determinate factors.
To assure the quality of data, questionnaires were first prepared in English language then translated to Amharic and, back to English to keep its consistency among data collectors and respondents. Three data collectors (qualified diploma nurses) and two supervisors (BSc nurses) were assigned for data collection and supervision respectively. One day orientation was given for data collectors and supervisors about the objectives and processes of data collection by the principal investigator. Pre-test was conducted on 10% (36 samples) of total sample size where the area was not included in the main study (Kalu district). Additionally, all completed questionnaires were collected and examined by the principal investigator on daily basis.
Data were cheeked and cleaned for completeness, organized and entered into Epi-info version 7 and then exported to SPSS version 25 software for cleaning, cross-checking, and analysis. Tables and graphs were used to present the results. Descriptive statistical analysis such as frequencies and percentages were used to describe the sample characteristics and the responses to the questioner items. Both binary and multivariable logistic regression model were used to identify factors that result suboptimal breast feeding practice. Those variables with pvalue <0.25 in binary logistic regression was fitted to multivariable logistic regression model for controlling the possible effects of confounders. Finally, the variables that were statistically significant with suboptimal breast feeding practice were identified on the basis of odds ratio (AOR), with 95% CI and at p <0.05.
Results
Socio-demographic characteristics of the study participants
A total of 346 mothers of children age 24-59 months were completed the study making a response rate of 98%. Mothers’ mean age was 26.6 years (SD ± 5.8) and ranged from 18-45 years. The mean age of children were 34 months (SD ± 4.3) and ranged from 24 to 59 months. Almost half (50.5%) of the mothers were in the age group of <24 years (Table 2).
| S. no | Variable | Category | Frequency (n) | Percentage (%) |
|---|---|---|---|---|
| 1 | Age (in years) | <24 | 175 | 50.5 |
| >25 | 171 | 49.5 | ||
| 2 | Age child (in months) | 24-35 | 94 | 27 |
| 36-47 | 154 | 44.5 | ||
| 48-59 | 98 | 28.5 | ||
| 3 | Child gender | Male | 152 | 43.9 |
| Female | 194 | 56.1 | ||
| 4 | Number of U5 children | 1 | 64 | 18.5 |
| >=2 | 282 | 81.5 | ||
| 5 | Parity | 1-2 | 36 | 10.4 |
| 3-4 | 147 | 42.5 | ||
| >4 | 163 | 47.1 | ||
| 6 | Birth order | First | 45 | 13 |
| 2-3 | 185 | 53.4 | ||
| >=4 | 116 | 33.6 | ||
| 7 | Postnatal care | Yes | 98 | 28.3 |
| No | 248 | 71.7 | ||
| 8 | Types of delivery | Vaginal | 205 | 59.2 |
| Cesarean | 141 | 40.8 | ||
| 9 | Place of delivery | Home | 211 | 61 |
| Health facility | 135 | 39 | ||
| 10 | Counseling on BF at ANC visit | Yes | 302 | 87.3 |
| No | 44 | 12.7 | ||
| 11 | ANC Visit | Yes | 245 | 70.8 |
| No | 101 | 29.2 | ||
| 12 | Number of ANC Visit | None | 101 | 29.2 |
| 1-3 | 201 | 58.1 | ||
| >=4 | 44 | 12.7 |
Note: ANC: Antenatal Care
Table 2. Socio-demographic characteristics of respondents in Dessie Zuria, South Wollo, Ethiopia, 2020 (n=346).
Characteristics of mothers with children aged 24-59 months
In this study, around sixty percent (58.1%) of mothers had at least one to three antenatal care visits. In this study 12.7% of mothers attended four and above ANC visits. Among those who attended ANC visits, 87.3% received counselling about breast feeding practices. More than half 61% of the mothers gave birth at home. Two hundred eighty two (81.5%) of the mothers had >= 2 under five child (Table 1).
Maternal knowledge about breast feeding practices
Majority, 231 (66.7%), of the study participants were found to have awareness on early initiation of breast feeding within one hour after delivery, and 254 (73.4%) knew the recommended months to start complementary feeding (Table 3).
| Variable | Category | Frequency (n) | Percent (%) |
|---|---|---|---|
| Economic status of household (ETB) | <1000 | 112 | 32.3 |
| 1000-2000 | 95 | 27.4 | |
| >2000 | 139 | 40.3 | |
| Ownership of radio | Yes | 78 | 22.5 |
| No | 268 | 77.5 | |
| Breast feeding imitation | Within 1 hour | 231 | 66.7 |
| After 1 hour | 115 | 33.3 | |
| Given colostrum | Yes | 312 | 90.2 |
| No | 34 | 9.8 | |
| Pre-lacteal feeding | Yes | 257 | 74.3 |
| No | 89 | 25.7 | |
| Exclusively BF | Yes | 132 | 38 |
| No | 214 | 62 | |
| Timely complementary feeding | Yes | 254 | 73.4 |
| No | 92 | 26.6 | |
| BF frequency | <8 times | 302 | 87.3 |
| >= 8 times | 44 | 12.7 | |
| Aware about importance of early initiation of breast feeding | Yes | 241 | 69.6 |
| No | 105 | 30.4 | |
| Aware about importance of feeding colostrum. | Yes | 195 | 56.4 |
| No | 151 | 43.6 | |
| Aware about importance of exclusive breast feeding | Yes | 201 | 58 |
| No | 145 | 42 | |
| Aware about continuity of breast feeding for 2 years and above | Yes | 218 | 63 |
| No | 128 | 37 | |
| Know when to start complementary feeding | Yes | 251 | 72.5 |
| No | 95 | 27.5 |
Note: BF: Breast Feeding; ETH: Ethiopian Birr
Table 3. Suboptimal breastfeeding factors description of respondents in Dessie Zuria, South Wollo, Ethiopia, 2020 (n=346).
Factors associated with delayed initiation of breast feeding
On binary logistic regression, age of women, educational status, family size, number of under five year children, number of antenatal care visits, counselling on breastfeeding during antenatal care visits, and listening for radio were found to have statistically significantly associated with suboptimal breastfeeding. However, after controlling for possible confounders on multivariable logistic regression analysis, women educational status, number of antenatal care visits, counselling on breast feeding during antenatal care visits, and listening for radio were found to be significant predictors of suboptimal breastfeeding practice. Mothers who had radio were found to be 69% less likely to sub optimally breastfeed her child than those with no radio (AOR=0.31; 95% CI (0.04, 0.96)). On the contrary, Mothers who had no formal education (illiterate) were nearly two times more likely to practice sub- optimal breastfeed to their child than those who were literates mothers (AOR: 1.74; 95% CI (1.17, 2.59)); and those mothers who had no ANC visit were 1.3 times more likely to delay initiation of breastfeeding than those with two and more children (AOR=1.3; 95% CI (1.19, 2.90)).
| Variable | Category | Suboptimal BF | COR: 95% CI | AOR: 95% CI | |
|---|---|---|---|---|---|
| Yes n (%) | No n (%) | ||||
| Age mother | 18-24 | 28 (9.1) | 15 (5.3) | 0.62 (0.38, 1.01) | 0.52 (0.27, 1.00) |
| 25-34 | 64 (23.5) | 34 (16) | 0.55 (0.34, 0.88) | 0.61 (0.35, 1.05) | |
| >= 35 | 111 (41.8) | 67 (31) | 1 | 1 | |
| Maternal education | Illiterate | 67 (23.7) | 54 (18) | 1.28 (1.10, 2.08) | 1.74 (1.17, 2.59)* |
| literate | 151 (52.3) | 76 (29) | 1 | 1 | |
| Having radio | Yes | 78 (32) | 38 (15) | 0.76 (0.13, 0.96) | 0.31 (0.04, 0.96) * |
| No | 142 (47) | 67 (28) | 1 | 1 | |
| Number of ANC visit | None | 140 (43.5) | 35 (12) | 1.72 (0.82, 3.61) | 1.30 (1.19, 2.90)* |
| 1-3 | 37 (16) | 65 (25) | 3.01 (2.15, 4.22) | 2.40 (1.68, 3.43) | |
| >= 4 | 54 (18) | 71 (28) | 1 | 1 | |
| Breastfeeding counseling at ANC visit | Yes | 184 (61) | 91 (30) | 2.15 (1.56, 2.95) | 1.69 (1.19, 2.4)* |
| No | 38 (16) | 26 (9) | 1 | 1 | |
Note: AOR: Adjusted Odds Ratio, COR: Crude Odds Ratio, CI: Confidence Interval
Table 4. Factors associated with suboptimal breastfeeding among 24-59 months old child in Dessie Zuria, South Wollo, Ethiopia, 2020 (n=346).
Discussion
This study assessed the prevalence of sub-optimal breastfeeding practice and predictor factors among women having children of age 24-59 months in Dessie Zuria. The prevalence of sub-optimal breast feeding in this study was 46.3% (CI: 39.4-57.2).
Among those who breastfed their child sub-optimally, 33.3% had delayed initiation of breast feeding, 62% fed breast none exclusively, and 9.8% discarded colostrum. This finding is lower than the study conducted in Jimma, Arjo district (75.4%) [17]. This might be due to the difference in the context (sociocultural difference) and the implementation of the maternal and child health programs. The prevalence of sub-optimal breast feeding in this study area remains high mainly due to cultural beliefs. Similarly, the prevalence of delayed initiation of breast feeding (after the first hour of birth) was found to be 49.4% (95% CI: 46.8-52.3). This finding is consistent with the 2011 Ethiopian Demographic and Health Survey’s (EDHS) report (48%), Jimma, Arjo district (37%), Goba Woreda (47.6%), Enagu, Nigeria (47%) [18] and in Africa (50%).
On the other hand, this finding is higher than the finding of the study conducted in the rural part of Ethiopia (31.1%), Debre Berhan (17.5%), Bishoftu (28.2%) and Arbaminch Zuria (42.8%) [20]. However, it is lower than the findings of the studies conducted in Nigeria (62%), (53.9%), and Pakistan (72.7%). According to EDHS reports, the prevalence of delayed initiation of breastfeeding was increased from (31%) to (48%) between 2005 and 2011. This implies that early initiation of breastfeeding did not show significant improvement despite the efforts to improve child health. The possible explanations for this difference could be difference in socio-demographic characteristics of the respondents and the place where the study was conducted [19].
This study showed that suboptimal breastfeeding was more likely to be practiced among mothers who did not attend formal education than mothers who were literates. This finding is similar with the finding of the studies conducted in Jimma, Arjo district and Nigeria. Moreover, another study conducted in Goba district, Southeast Ethiopia, also showed that mothers who had formal education were observed to practice early initiation of breastfeeding within the first hour of delivery. This might be related to the fact that mothers who attended formal education were more informed about timely initiation of breastfeeding.
In addition, mothers who had no radio were more likely to breastfeed sub-optimally than mothers who had radio at home. This finding is consistent with the study done in Nigeria. The possible explanation for this finding is that mothers with radio had more chance of listening and learning experience of breast feeding practice.
Moreover, mothers who had no ANC visit were 1.3 times to breastfeed sub-optimally compared with mothers who had four and more ANC visits. This finding had agreement with the study conducted in Nigeria in which frequent ANC visit was associated with early initiation of breast feeding. However, this finding is inconsistent with the finding of a study conducted in a rural part of Ethiopia in which sub optimal breast feeding was not affected by the number of ANC visits. This inconsistency could be due to the difference in the sample size and study setting [20].
Mothers who were not counselled about breastfeeding during ANC visits were more likely to breast feed sub optimally. This finding is similar with findings of studies conducted in a rural part of Ethiopia and a study on factors that influence breast feeding. This might be due to the fact that mothers did not receive breast feeding counselling at the appropriate time and were not aware of when to initiate breast feeding. Nonexclusive breast feeding practice was found to be 13.4% (95% CI: 11.6-15.4) among mothers having infants aged 24-59 months. This finding is lower than the findings of studies conducted in East Ethiopia (28.3%), Enderta Woreda (29.8%), Debre Markos (39.2%), Gondar Town (47.5%), EDHS 2011 (48%) (9), Debre Berhan (49.8%), Arbaminch Zuria (44.4%), Bishoftu (65.9%), Ethiopia (51%) (28), Nigeria (86%), Mecha District (52.9%), Enagu, Nigeria (65.5%), Pakistan (62.9%) and developing countries (61%).
Conclusion
Generally, this study revealed that the prevalence of suboptimal breast feeding was significantly high that indicates it is one of the reason for high magnitude of under-five mortality. Few numbers of mothers tend to introduce pre-lacteal foods and discarded colostrum. Not attending formal education, lack of breast feeding counselling, lower number of or no ANC visits, having no radio were found to be aggravating factors of sub optimal breast feeding practice.
Health extension workers should address the traditional and cultural belief relating to discarding colostrum, delayed initiation of breast feeding, non-exclusive breast feeding and create awareness on benefits of optimal breast feeding practices. Healthcare workers should counsel women about optimal breast feeding practice during ANC visits, delivery and postnatal care services. The district administration should give emphasis to increase the formal education enrolment of women. The federal ministry of health and non-governmental organizations working on infant and young child feeding programs should focus on factors that cause sub optimal breast feeding practice.
Limitations of the Study
This study was a cross-sectional study; the cause effect relationship of different variables with sub optimal breast feeding was not assessed. Maternal skills of breastfeeding practice (positioning and attachment) were not measured.
To generate more information from the study participants, it would have been good if qualitative data collection approaches were considered besides the quantitative one. Recall bias was another challenge during this study.
Ethical Considerations
The actual data collection was carried out after getting ethical approval from the ethical review committee of Wollo university, college of medicine and health sciences with the date and reference number of the approval letter was: CMHS 715/02/11 on 08/02/2011. In addition, the official letter of cooperation was submitted to local authorities and informed written consent was obtained from each respondent prior to enrollment. Each participant was informed about the aim of the study and respondent who are not willing to participate in the study had full right to refuse or even withdraw from participation. They were also informed that all data obtained from them would be kept confidential by assigned codes instead of using name and other personal identifiers and the information is used only for the purpose of the study.
References
- Jackson KM, Nazar AM. Breastfeeding, the Immune Response and Longterm Health. JAOA. 2006;106(4):203-07.
[Google Scholar] [PubMed]
- WHO: Global Strategy for Infant and Young Child Feeding. Geneva, Switzerland: A joint WHO/UNICEF statement. Geneva, WHO; 2003.
- WHO: Report of the global consultation on Summary of guiding principles for complementary feeding of the breastfed child. Geneva: World Health organization; 2001.
- Federal Ministry of Health: National Strategy for Child Survival in Ethiopia. Family health department; 2005.
- Mary Arimond, Marie TR. Food and Nutrition Technical Assistance Project (FANTA): Summary Indicators for Infant and Child Feeding Practices. From the Ethiopia Demographic and Health survey 2000. Academy for Educational Development. Washington, DC, USA. 2002.
- Central Statistical Agency/Ethiopia and ORC Macro.. Ethiopia Demographic and Health Survey 2005. Addis Ababa, Ethiopia: Central Statistical Agency/Ethiopia and ORC Macro; 2006.
- Kruger R, Gericke GJ. A qualitative exploration of rural feeding and weaning practices, knowledge and attitudes on nutrition in South Africa. Public Health Nutr. 2002;6(2):217-23.
[Crossref] [Google Scholar] [PubMed]
- Shirima M, Gebre Medhin, Greiner T. Information and socioeconomic factors associated with early breastfeeding practices in rural and urban Morogoro, Tanzania. Acta Paediatr. 2001; 90:936-42.
[Crossref] [Google Scholar] [PubMed]
- Steve IO. nutritional status and feeding practices of infants among low income nursing mothers in Ondo state, Nigeria. Int J Trop Med. 2006;1(3):123-9.
- Semega Janneh IJ, Bohler E, Holm H, et al. Promoting breastfeeding in rural Gambia: combining traditional and modern knowledge. Health Policy Plan. 2001;16(2):199-205.
[Google Scholar] [PubMed]
- Ludvigsson JF. Breastfeeding in Bolivia. BMC Pediatr. 2002;3:4.
[Crossref] [Google Scholar] [PubMed]
- Engebretsen IM, Wamani H, Karamagi C, et al. Low adherence to exclusive breastfeeding in Eastern Uganda: A community-based cross sectional study comparing dietary recall since birth with 24-hour recall. BMC Pediatr. 2007; 7:10.
[Crossref] [Google Scholar] [PubMed]
- Jolly N, Tumwine JK, Ashild S, et al. Community based peer counsellors for support of exclusive breastfeeding: Experiences from rural Uganda. Int Breastfeed J. 2006; 1:19.
[Crossref] [Google Scholar] [PubMed]
- Ergenekon Ozelci N, Elmaci M, Ertem, et al. Breastfeeding beliefs and practices among migrant mothers in slums of Diyarbakir, Turkey. European Journal of Public Health. 2006;16(2):143-48.
[Google Scholar] [PubMed]
- Kori B, Flower, Michael, et al. Understanding breastfeeding initiation and continuation in rural communities. Maternal Child Health J. 2008;12(3):402-14.
[Crossref] [Google Scholar] [PubMed]
- Tewodros A, Jemal H, Dereje H. Determinants of exclusive breastfeeding practices in Ethiopia. Ethiop JHealth Dev. 2009; 23(1):12-8.
- Tamiru D, et al. Sub-optimal breastfeeding of infants during the first six months and associated factors jimma Arjo woreda. BMC Public Health. 2012;1-9.
[Crossref] [Google Scholar] [PubMed]
- Shifraw T, et al. Factors associated exclusive breastfeeding practices of urban women in Addis Ababa public health centers. Int Breastfeed J. 2015;10(1):1-6.
[Crossref] [Google Scholar] [PubMed]
- Ogbo FA, et al. Determinants of suboptimal breastfeeding practices. BMC Public Health. 2015;15(1):1-2.
[Crossref] [Google Scholar] [PubMed]
- World Health Organization, UNICEF. Global nutrition target 2025 breast feeding policy brief. Geneva: WHO/UNICEFI, 2014.