Research Article - Biomedical Research (2017) Volume 28, Issue 19
Study on detection of platelet membrane glycoprotein CD62p in patient with atrial fibrillation after radiofrequency ablation treatment
Feifei Tian1,2, Yongjun Mao3*, Shanglang Cai4 and Xiaofei Sun2
1Qingdao University, Qingdao, Shandong, PR China
2Department of Cardiology, Jining No.1 People's Hospital, PR China
3Department of Geriatrics, the Affiliated Hospital of Qingdao University, PR China
4Department of Cardiology, the Affiliated Hospital of Qingdao University, PR China
- *Corresponding Author:
- Yongjun Mao
Department of Geriatrics
The Affiliated Hospital of Qingdao University
PR China
Accepted date: September 18, 2017
Abstract
Objective: As a type of arrhythmia, Atrial Fibrillation (AF) seriously affects human health. Although Radiofrequency Catheter Ablation (RFCA) has been proved to be a safe and effective method for the treatment of AF, thromboembolism caused by this treatment limited its application. Our study aimed to investigate the effects of calcium channel blocker amlodipine on thrombosis-related factors after RFCA.
Methods: A total of 68 patients with AF underwent RFCA were selected from Jining No.1 People's Hospital from September 2015 to December 2016. Patients were randomly divided into groups A and B. Patients in group A received RFCA only, while patients in group B were treated with amlodipine for 3 consecutive days before RFCA. Elbow venous blood was extracted from each patient before intravenous catheterization, after electrophysiological examination and before RFCA, just after RFCA, 24 h after RFCA and 48 h after RFCA. Levels of CD62P, Thromboxane B2 (TXb2), Interleukin 6 (IL6), D-Dimer and protein C in plasma were detected by Enzyme-Linked Immunosorbent Assay (ELISA).
Results: Compared with preoperative levels, levels of CD62P, TXb2, IL6, D-Dimer and protein C in plasma of group A were significantly increased after RFCA (p<0.05), and then decreased. But no significantly differences were found between preoperative levels and levels at 48 h after operation. No significant differences in levels of CD62P, TXb2, IL6, D-Dimer and protein C in plasma were found between different time points in group B.
Conclusion: RFCA in the treatment of atrial fibrillation can increase the risk of thrombosis, while preoperative treatment with amlodipine can reduce the risk.
Keywords
Atrial fibrillation, Radiofrequency catheter ablation, Thrombosis, Amlodipine
Introduction
As one of the most common cardiac arrhythmias, Atrial Fibrillation (AF) affects more than 20% people during their lifetime world widely including China, and the incidence of AF is higher in men than in women [1]. It has been estimated that more than 33 million individuals are suffering from AF [2]. Serious complications of AFI include heart dementia, failure, stroke or even death [2,3]. Even worse, the incidence of AF is predicted to increase steeply in near future [4]. A variety of treatment strategies have been developed to treat AF. Among those treatments, Radiofrequency Catheter Ablation (RFCA) has been proven to be a safe and effective treatment for patients with AF. Significant improvements in quality of life and extremely incidence of complications were observed in majority of AF patients after RFCA [5]. However, in some rare cases, RFCA can cause thromboembolism, leading to the poor treatment outcomes [6]. Therefore, the development of treatment strategies which can be used to inhibit thrombosis after RFCA is always needed.
Calcium channel plays pivotal roles in the pathogenesis of various human diseases including thrombosis. A calcium sensor, which is called STIM1, has been proved to be an essential mediator of ischemic brain infarction and arterial thrombosis [7]. Based on this, different calcium channel blockers have been widely used in clinical practices to inhibit thrombosis caused by various factors. In the study of stent thrombosis, which is one of the severe complications of percutaneous coronary intervention, Nagano et al. reported that the use of calcium channel blockers could significantly reduce the incidence of stent thrombosis within 1 year after drugeluting stent implantation in Japanese patients [8]. In view of this, it will be reasonable to hypothesize that calcium channel blockers can also be used to inhibit thrombosis caused by RFCA in the treatment of patients with AF.
In this study, patients with AF were treated with calcium channel amlodipine before RFCA. Effects of amlodipine on levels of thrombosis-related factors in plasma were explored.
Materials and Methods
Patients
A total of 68 patients with Atrial Fibrillation (AF) who were willing to receive Radiofrequency Catheter Ablation (RFCA) were selected in Jining No.1 People's Hospital from September 2015 to December 2016. Among those patients, there were 36 males and 32 females, and the age ranged from 36 y to 72 y and the course of disease ranged from 4 months to 21 y. Patients with a history of thromboembolism or hemorrhagic disease were not included. All patients were prevented from treatment with antiarrhythmic drugs for more than 5 half-lives. Patients were randomly divided into groups A and B. Group A included 16 males and 18 female, and the age ranged from 36 to 71 y with an average age of 62.8 ± 5.2 y. Group B included 20 males and 14 females, and the age ranged from 38 y to 72 y with an average age of 66.6 ± 6.3 y. No significant differences in basic information were found between two groups (p>0.05). Patients in group A were only treated with RFCA (40 W for 60 s), while patients in group B were treated with calcium channel blocker amlodipine (5 mg daily, Pfizer, China) for 3 consecutive days before RFCA (40 W for 60 s). No obvious side effects were observed after amodipline treatment. This study was approved by the ethics committee of our hospital (number here), all patients signed informed consent.
Specimen collection
Elbow venous blood (about 5 m) was extracted from each patient before intravenous catheterization, after electrophysiological examination and before RFCA, just after RFCA, 24 h after RFCA and 48 h after RFCA, and 2.5 ml was injected into a tube containing anticoagulant (5% EDTA) , and the other 2.5 ml was injected into another tube containing sodium citrate (anticoagulant). Blood samples were centrifuged at 3000 rpm for 10 min to collect plasma.
Detection of related indicators
Plasma samples derived from the tube containing 5% EDTA were used to measure the contents of CD62P, TXb2 and IL6 using ELISA kits (catalog no. BBE6, catalog no. KGE011, catalog no. HS600B, R&D systems, USA). Plasma samples derived from the tube containing sodium citrate ere used to measure the contents of D-Dimer and protein C using ELISA kits provided by Nanjing Jin Yibai Biological Technology Co. Ltd. (catalog no. JEB-13891) and Shanghai Jingkang Biological Engineering Co., Ltd. (catalog no. JK-02819).
Statistical analysis
GraphPad Prism 5.0 statistical software was used for statistical analysis. All data were expressed as mean ± Standard Deviation (mean ± SD). Comparison between groups was performed by t test, and comparisons within groups were performed using paired t-test, p<0.05 was considered to be statistically significant.
Results
Comparison of plasma level of CD-62P between different time points in two groups of patients
Plasma level of CD62P significantly increased during RFCA in group A, and reached a peak at the time point just after RFCA, which was significantly higher than the preoperative level (p<0.05). CD62P level in group A gradually decreased after RFCA, and no significant difference was found between preoperative level of CD62P and the level of CD62P at 48 h after RFCA (p>0.05). No significant differences in level of CD62P were found between different time points in group B (p>0.05). Those data suggested that preoperative treatment with amlodipine could reduce the increased plasma level of CD62P caused by RFCA (Table 1).
| Time points | Plasma CD62P content | p | |
|---|---|---|---|
| Group A (ng/L) | Group B (ng/L) | ||
| Before intravenous catheterization | 5.32 ± 0.81 | 5.08 ± 0.92 | >0.05ii |
| After electrophysiological examination and before RFCA | 7.36 ± 0.46 | 5.67 ± 0.35 | >0.05i,ii |
| Just after RFCA | 13.58 ± 1.89 | 6.28 ± 1.22 | <0.05i,ii |
| 24 h after RFCA | 7.46 ± 1.26 | 5.67 ± 1.07 | >0.05i,ii |
| 48 h after RFCA | 5.69 ± 1.38 | 5.59 ± 0.75 | >0.05i,ii |
| Notes: icompared with the level before intravenous catheterization; iicomparison between groups at the same time point. | |||
Table 1: Comparison of plasma level of CD-62P between different time points in two groups of patients.
Comparison of plasma level of TXb2 between different time points in two groups of patients
Plasma level of TXb2 significantly increased during RFCA in group A, and the peak was reached at the time point just after RFCA, which was significantly higher than the preoperative level (p<0.05). TXb2 level in group A gradually decreased to normal level after RFCA. No significant differences in level of TXb2 were found between different time points in group B (p>0.05). Those data suggested that preoperative treatment with amlodipine could reduce the increased plasma level of TXb2 caused by RFCA (Table 2).
| Time points | TXb2 (ng/L) | p | |
|---|---|---|---|
| Group A | Group B | ||
| Before intravenous catheterization | 85.23 ± 2.58 | 86.64 ± 1.23 | >0.05ii |
| After electrophysiological examination and before RFCA | 87.06 ± 1.40 | 85.09 ± 2.29 | >0.05ii |
| Just after RFCA | 131.26 ± 5.87 | 90.68 ± 2.94 | <0.05i,ii |
| 24 h after RFCA | 95.33 ± 6.32 | 90.96 ± 1.71 | >0.05i,ii |
| 48 h after RFCA | 90.46 ± 2.56 | 87.53 ± 1.27 | >0.05i,ii |
| Notes: icompared with the level before intravenous catheterization; iicomparison between groups at the same time point | |||
Table 2: Comparison of plasma level of TXb2 between different time points in two groups of patients.
Comparison of plasma level of D-dimer between different time points in two groups of patients
In group A, plasma level of D-dimer significantly increased during RFCA, and the peak value of D-dimer in plasma was detected just after RFCA, which was significantly higher than the level before intravenous catheterization (p<0.05). D-dimer level in group A gradually decreased to normal level after RFCA. In group B, no significant differences in level of D-dimer were found between different time points (p>0.05). Those data suggested that preoperative treatment with amlodipine could reduce the increased plasma level of D-dimer caused by RFCA (Table 3).
| Time | D-dimer (µg /L) | p value | |
|---|---|---|---|
| Group A | Group B | ||
| Before intravenous catheterization | 578 ± 232 | 603 ± 237 | >0.05ii |
| After electrophysiological examination and before RFCA | 967 ± 265 | 662 ± 309 | >0.05ii |
| Just after RFCA | 1886 ± 682 | 751 ± 383 | <0.05i,ii |
| 24 h after RFCA | 981 ± 339 | 681 ± 254 | >0.05i,ii |
| 48 h after RFCA | 821 ± 235 | 623 ± 189 | >0.05i,ii |
| Notes: icompared with the level before intravenous catheterization; iicomparison between groups at the same time point | |||
Table 3: Comparison of plasma level of D-dimer between different time points in two groups of patients.
Comparison of plasma level of protein C between different time points in two groups of patients
As shown in Table 4, no significant differences in level of protein C were found between different time points in both groups A and B (p>0.05). Those data suggested that protein C was not affected by RFCA.
| Time | Protein C (ng/L) | p value | |
|---|---|---|---|
| Group A | Group B | ||
| Before intravenous catheterization | 4.35 ± 0.26 | 4.23 ± 0.31 | >0.05ii |
| After electrophysiological examination and before RFCA | 4.69 ± 0.25 | 4.46 ± 0.09 | >0.05ii |
| Just after RFCA | 4.66 ± 0.82 | 4.68 ± 0.85 | >0.05i,ii |
| 24 h after RFCA | 4.87 ± 0.39 | 4.87 ± 0.48 | >0.05i,ii |
| 48 h after RFCA | 4.69 ± 0.35 | 4.58 ± 0.89 | >0.05i,ii |
| Notes: icompared with the level before intravenous catheterization; iicomparison between groups at the same time point | |||
Table 4: Comparison of plasma level of protein C between different time points in two groups of patients.
Comparison of plasma level of IL-6 between different time points in two groups of patients
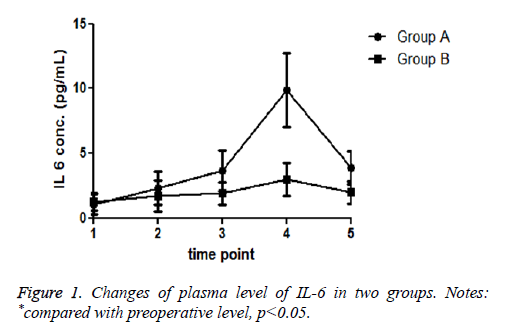
Compared with preoperative value, plasma level of IL-6 significantly increased during RFCA in group A, and the peak value of IL-6 in plasma was detected 24 h after RFCA, which was significantly higher than the level before intravenous catheterization (p<0.05). After that, IL-6 level in group A gradually decreased to normal level. In group B, no significant differences in level of IL-6 were found between different time points (p>0.05). Those data suggested that preoperative treatment with amlodipine could reduce the increased plasma level of IL-6 caused by RFCA (Figure 1).
Discussion
As one of the most frequent supraventricular arrhythmias, AF is considered to be a malignant disease that can cause various complications. For instance, the risk of stroke in patients with AS was reported to be 5 times higher than that of people with normal sinus rhythm [9]. In addition, AF was also found to be responsible for the increased risk of dementia and cognitive decline [10]. Various treatment strategies have been developed to treat AF. However, most of the treatments including pharmacological therapies failed to provide satisfactory outcomes due to individual responses. RFCA has been proved to be a safe and effective way to treat AF for patients who failed to tolerate medication. A comparison study carried out by Reynolds et al. has shown that RFCA is more effective in maintaining sinus rhythm compared with antiarrhythmic drugs [11], and this conclusion is further confirmed by Mont et al. [12]. However, in some extreme cases, RFCA can lead to the occurrence of thrombosis. According to the retrospective studies and worldwide surveys, the incidence of symptomatic thromboembolic complications in patients with AF ranged from 0.5% to 0.9% after RFCA [13]. Therefore, how to prevent thrombosis has become a focus for studies on the application of RFCA in the treatment of AF.
It has been reported that calcium channel plays pivotal roles in thrombosis [7], which indicates that calcium channel blockers may have therapeutic effect on thrombosis. Previous studies have shown that, nifedipine, as an L-type calcium channel blocker, can achieve its antiplatelet function by activating PPAR-β/-γ- mediated signaling pathways to inhibit thrombosis [14]. In the study of stent thrombosis, Nagano et al. reported that the use of calcium channel blockers could significantly reduce the incidence of stent thrombosis caused by drug-eluting stent implantation [8]. In another study which focused on arterial hypertension, Liakos et al. found that calcium channel blockers could reduce thrombotic response caused by acute exercise, which in turn inhibited exercise-induced acute phase response [15]. Those previous studies suggest that calcium channel blockers may also have therapeutic effects on thrombosis caused by RFCA.
The progression of thrombosis is a complex process, within which platelet activation plays a key role. The activation of platelet including aggregation, expression of procoagulant activity, secretion and shape change are closely related to the changes in level of intraplatelet Ca2+, which is associated with the translocation of CD62P (P-selectin) from membrane of α- granule to platelet membrane, where CD62P promote the interaction between platelets and various types of cells including leukocyte and monocyte, eventually leading to thrombosis [16]. As a platelet activating factor, the level of TXb2 is usually increased during the activation of platelet to contribute to thrombosis [17]. The activated platelets can increase the release of proinflammatory cytokine IL-6, which in turn induces the activation of the coagulation cascade through the interaction with TF pathway [18]. D-Dimer is a circulating marker, and the level of D-Dimer is usually significantly increased during the acute phase of the disease [19]. Consistent with previous studies, in our study, plasma levels of CD62P, TXb2, IL6 and D-Dimer were significantly increased after RFCA in patients without preoperative treatment of calcium channel blocker amlodipine, indicting the existing of thrombotic responses caused by RFCA. With amlodipine treatment, no significant differences in the plasma levels of CD62P, TXb2, IL6 and D-Dimer were found between different time points. Those results suggest that amlodipine treatment can significantly reduce the thrombotic responses caused by RFCA. The progression of thrombosis is also regulated by anticoagulant pathways, within which the protein C system with protein C as the main component can regulate both hemostatic and inflammatory systems [20]. It has been reported that the activation of protein C can induce the degradation of essential coagulation cofactors Va and VIIIa through its cofactor protein S, which in turn alleviates blood coagulation [21]. In our study, no significant differences in plasma level of protein C were found in both groups between different time points. Those results suggested that protein C was not activated by RFCA, and protein C is also involved in the inhibitory effects of amlodipine on thrombosis.
In summary, in this study we found that RFCA can induce thrombosis by upregulating the levels of CD62P, TXb2, IL6 and D-Dimer in plasma, while amlodipine can inhibit RFCAinduced thrombosis by downregulating the plasma levels of those factors. Protein C is not involved in either process. Our study is still limited by the small sample size. Future studies with bigger sample size are still needed to further confirm our conclusions.
References
- Christophersen IE, Rienstra M, Roselli C. Large-scale analyses of common and rare variants identify 12 new loci associated with atrial fibrillation. Nat Gene 2017; 49: 946-952.
- Chugh SS, Havmoeller R, Narayanan K. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation 2013.
- January CT, Wann LS, Alpert JS. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2014; 64: 2246-2280.
- Kirchhof P, Benussi S, Kotecha D. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 2016; 37: 2893-2962.
- Kalla M, Sanders P, Kalman JM. Radiofrequency catheter ablation for atrial fibrillation: approaches and outcomes. Heart Lung Circulation 2017.
- Gaita F, Caponi D, Pianelli M. Radiofrequency catheter ablation of atrial fibrillation: a cause of silent thromboembolism. Circulation 2010; 122: 1667-1673.
- Varga-Szabo D, Braun A, Kleinschnitz C. The calcium sensor STIM1 is an essential mediator of arterial thrombosis and ischemic brain infarction. J Exp Med 2008; 205: 1583-1591.
- Nagano M, Hokimoto S, Nakao K. Relation between stent thrombosis and calcium channel blocker after drug-eluting stent implantation: Kumamoto Intervention Conference Study (KICS) registry. J Cardiol 2015; 66: 333-340.
- Benjamin EJ, Wolf PA, Dagostino RB. Impact of atrial fibrillation on the risk of death. Circulation 1998; 98: 946-952.
- Vermeer SE, Prins ND, den Heijer T. Silent brain infarcts and the risk of dementia and cognitive decline. N Engl J Med 2003; 348: 1215-1222.
- Reynolds MR, Walczak J, White SA. Improvements in symptoms and quality of life in patients with paroxysmal atrial fibrillation treated with radiofrequency catheter ablation versus antiarrhythmic drugs. Circ Cardiovasc Qual Outcomes 2010; 3: 615-623.
- Mont L, Bisbal F, Hernandez-Madrid A. Catheter ablation vs. antiarrhythmic drug treatment of persistent atrial fibrillation: a multicentre, randomized, controlled trial (SARA study). Eur Heart J 2013; 35: 501-507.
- Verma A. Atrial-fibrillation ablation should be considered first-line therapy for some patients. Curr Opin Cardiol 2008; 23: 1-8.
- Chou TC. New mechanisms of antiplatelet activity of nifedipine, an L-type calcium channel blocker. Bio Med 2014; 4.
- Liakos CI, Vyssoulis GP, Michaelides AP. The effects of angiotensin receptor blockers vs. calcium channel blockers on the acute exercise-induced inflammatory and thrombotic response. Hypertens Res 2012; 35: 1193-1200.
- Labios M, Martínez M, Gabriel F. Cytoplasmic free calcium mobilization in platelets, expression of P-selectin, phosphatidylserine, and microparticle formation, measured by whole blood flow cytometry, in hypertensive patients. Effect of doxazosin GITS. Thromb Res 2006; 117: 403-409.
- Wu H, Lei Z, Gao S. Yiqi Huoxue decoction and its constituents inhibit the activation of platelets and thrombosis for the prevention and treatment of cardiovascular diseases. FASEB J 2017; 31: 677.
- Levi M, van der Poll T, Buller HR. Bidirectional relation between inflammation and coagulation. Circulation 2004; 109: 2698-2704.
- Righini M, Van Es J, Den Exter PL. Age-adjusted D-dimer cut-off levels to rule out pulmonary embolism: the ADJUST-PE study. JAMA 2014; 311: 1117-1124.
- Rezaie AR. Regulation of the protein C anticoagulant and antiinflammatory pathways. Curr Med Chem 2010; 17: 2059-2069.
- Levi M, van der Poll T. Inflammation and coagulation. Crit Care Med 2010; 38: 26-34.