Case Report - Biomedical Research (2017) Volume 28, Issue 6
Study on breast cancerous organs depth and coverage parameters via Debye and monostatic rader techniques with UWB-microstrip patch antennas
Sakthisudhan K1* and Anitha R2
1Department of Electronics and Communication Engineering, Adhi College of Engineering and Technology, India
2Department of Computer Science & Engineering, Adhi College of Engineering and Technology, India
- *Corresponding Author:
- Sakthisudhan K
Department of Electronics and Communication Engineering
Adhi College of Engineering and Technology, India
Accepted on November 12, 2016
Abstract
A 5 GHz class of Microstrip Patch Antenna (MPA) designed, simulated, fabricated and measured has been presented in this research paper. Furthermore, comparative study on existing Debye test bed and Monostatic radar techniques have been implemented for depth and coverage of cancerous organ parameters respectively via 2 × 2 array pattern of ΨU shaped UWB-MPAs. The proposed MPA offers enhanced design parameters and lesser complexity than existing 3GHz MPAs. For an example, the proposed UWB-MPAs prototype provides operating frequency of 4.53 GHz (15.99% of Fractional Bandwidth (FBW)) and complexity of 18.64 × 23.92 × 1 mm3. Hence, these MPAs have to analyse the vector dimensional and depth of cancerous organ has been presented in paper.
Keywords
Breast cancer diagnosis system, Debye test bed, Monostatic radar technique, Fractional bandwidth and UWB-MPAs.
Introduction
Breast cancer is a major challenge and health issue of the present society. The death rate has doubly risen in the past 30 years. The various diagnosis systems are authorized and followed to reduce the death rate. The Magnetic Resonance Imaging (MRI) and Positron Emission Tomography (PET) are the existing diagnosis trials. The X-ray mammography (XRM) is an efficient diagnostic tool but it has some limitations in the screening detection methods. They are, the heavy chemical dose applied on the human breast to affect ionization effects within the body and the harmful radiation effects during the clinical tests. Both of the above results provide in the injurious health issues. Normally, these radiology diagnostic trials do not offer the tissue’s sample based analysed report. These drawbacks of MRI, XRM and other existing techniques are recovered using the Microwave Imaging (MI) methods in [1]. The proposed test beds are able to conduct below 10 GHz range of microwave signals which requires the Specific Absorption Ratio (SAR) value of 4 W/Kg limitations. The microwave transmission of medical diagnosis has thermal and radiation effects. The thermal effect is used in therapy treatment which removes the cancerous organ. As the result of diagnosis, test beds provide the ionization and injurious effects. The radiation effect offers the non-ionization; cost effective, harmless effects and more number of clinical trials are possible to under the screening test. The Microwave Imaging (MI) methods provide the UWB based a radar approach which classifies the tumor resolution stages using scattered mapping algorithms. Consequently, efficient MPAs designs are required for breast cancer detection in UWB-MI diagnosis methods. The proposed UWB-MI diagnosis system and the drawbacks of prior diagnosis systems are discussed in the [1-3].
Materials and Methods
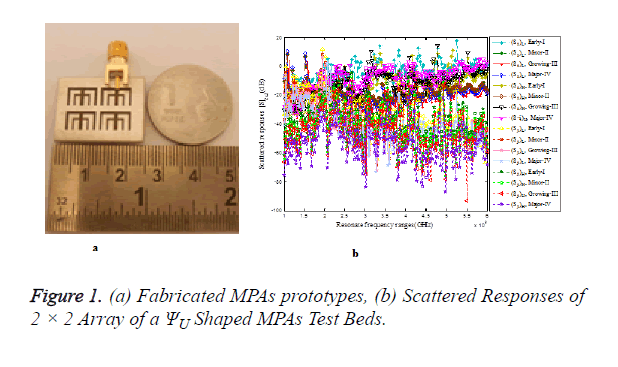
The compact size of 2 × 2 array pattern of MPAs with 5 GHz UWB band of operation and Industrial Scientific and Medicine (ISM) band of applications are presented in this section. The conductive patch strips propose to design a 2 × 2 array of four radiating elements. The proposed MPAs are design and simulated and fabricated procedures are followed in [3]. Furthermore, their complexity is lesser than existing design. Analyze of depth and coverage of parameters is justified in cancerous organ by existing test bed of [3]. The 5 GHz resonance class of 2 × 2 array patterns of MPAs and equivalent dielectric breast model are justified for depth of cancerous organ using different dielectric strengths of coupling materials. It has shown in Figure 1, the early time peak response of 25.75 dB has been obtained at 4.475 GHz. These scattered drops have clearly described the opposite values of dielectric strengths in the scattered responses. As the scattered drops of the higher dielectric strength offer above the 85 dB of scattered drops. These kinds of values are not reordered in the Agilent (N99917A) Microwave Analyzer with VNA. The healthy tissue module consisting of MPAs logically connects to wristband which is measured using Agilent (N99917A) Microwave Analyzer with VNA [3]. The return losses of 41.78 dB (Sii), 47.45 dB (Sjj) has been obtained at 2.414 GHz and 2.301 GHz. While, coupling losses (Sji=Sij) of 47.781 dB; 61.778 dB measured at 3.454 GHz to 3.812 GHz in the 2 × 2 array of a ΨU shaped MPAs based healthy tissue module respectively. Figure 1 show the subtracted scattered responses of the proposed MPAs respectively. The tumor information of 2.1 GHz to 4.834 GHz and early time responses are found at 2.53 GHz. These scattered responses are followed by previous test bed and derived from Equation [3]. The depth of the tumor of 2 × 2 array patterns of ΨU shaped MPAs based on Debye test model are compared with the MPAs based on Debye test model listed in the Table 1.
| Proposed mpas based debye test beds | Resolution stages/tumor size | Depth of major stage frequency fmajor (GHz) | Depth of early stage frequency fearly (GHz) | Travelling time δt (ns) | Analysed in proposed test beds Parameters | Fear et al. analysed in existing Debye test beds parameters | Physical Distance between the tumor with MPAs (cm) |
|||||
| Dielectric strength of tumor | Velocity of propagation (mm/s) |
Depth of tumor by numerical analysis (mm) | Dielectric strength of tumor | Velocity of propagation (mm/s) |
Depth of tumor by numerical analysis (mm) | |||||||
| Early-I 1 cm |
3.3 | 5.89 | 0.36 | 48.5 | 4.3 ´ 1010 | 30.96 | 9 | 1011 | 72 | 129.8 | ||
| Minor-II 2 cm |
2.55 | 5.49 | 0.34 | 48.5 | 4.3 ´ 1010 | 29.24 | 9 | 1011 | 68 | 127.4 | ||
| Growing-III 2.5 cm |
2.56 | 5.45 | 0.34 | 48.5 | 4.3 ´ 1010 | 29.24 | 9 | 1011 | 68 | 109.2 | ||
| Major-IV 3 cm |
3.65 | 5.49 | 0.53 | 48.5 | 4.3 ´ 1010 | 45.58 | 9 | 1011 | 106 | 110.4 | ||
| Proposed MPAs analysed in the existing test beds | Kiruthika et al. | 5 mm Tumor Size | 3.3 | 5.89 | 0.36 | 21.3 | 6.5 ´ 1010 | 46.8 | 9 | 1011 | 72 | 129.8 |
| 10 mm Tumor Size | 2.55 | 5.49 | 0.34 | 21.3 | 6.5 ´ 1010 | 44.2 | 9 | 1011 | 68 | 127.4 | ||
| 15 mm Tumor Size | 3.65 | 5.45 | 0.53 | 21.3 | 6.5 ´ 1010 | 68.9 | 9 | 1011 | 106 | 110.4 | ||
| Salvador Et al.. |
1 cm Tumor Size | 2.55 | 5.49 | 0.34 | 20 to 40 | 5.3 ´ 1010 | 36.04 | 9 | 1011 | 68 | 129.4 | |
| 2 cm Tumor Size | 3.65 | 5.49 | 0.53 | 60 to 80 | 3.1 ´ 1010 | 32.86 | 9 | 1011 | 106 | 109.2 | ||
Table 1. Comparison of the depth of the tumor in the 2 × 2 Array of a ΨU shaped MPAs and the existing MPAs based on Debye test beds [4-7].
It can be described that the perfectly matched tumor depth with a physical distance from phantom breast model has reliable accuracy with the Debye breast tumor model. The 2 × 2 array of ΨU shaped MPAs based Debye test beds are made up of two way duplex transmissions which is used for detection of dielectric equivalent of tumor materials placed in dielectric equivalent of the breast phantom model. Based on Debye test bed setup results are followed and determined in the two way monostatic radar modelling of Equations [3] are used to find out the detection of tumor resolution stages along the cancerous organ which are examined in Table 2.
| Coupling mediums | Tumor resolution stages | Target gain factor | Space path loss αGσdB | Received power at target PrdB | Maximum target coverage RMaxdB | Maximum sensitivity MOS | Total gain GrdB |
|---|---|---|---|---|---|---|---|
| Lower Dielectric Strength | Early-I 1 cm |
129.89 | 164.43 | 297.57 | 41.49 | -45.5 | 175.39 |
| Minor-II 2 cm |
140.77 | 169.52 | 306.67 | 83.13 | -49.5 | 190.27 | |
| Growing-III 2.5 cm |
147.356 | 172.34 | 308.29 | 80.79 | -76.86 | 224.2 | |
| Major-IV 3 cm |
153.186 | 175.33 | 313.94 | 79.38 | -78.3 | 231.48 | |
| Higher Dielectric Strength |
Early-I 1cm |
129.67 | 164.2 | 297.52 | 86.54 | 43.48 | 172.7 |
| Minor-II 2 cm |
141.97 | 170.73 | 305.3 | 82.49 | 76.28 | 218.25 | |
| Growing-III 2.5 cm |
147.53 | 172.51 | 308.57 | 80.83 | 77.3 | 224.8 | |
| Major-IV 3 cm |
153.186 | 175.33 | 314.05 | 79.79 | 64.94 | 218.13 |
Table 2. Analysis of the Maximum Target Detection of 2 × 2 Array of a ΨU shaped mpas based debye test beds.
Conclusion
The proposed MPAs have been concluded that the 1 × 2 array of ΨU shaped MPA is FBW of 31.7 % greater than 3 GHz class of UWB-MPAs [3]. Therefore, Sakthisudhan et al. [3] prototypes are not clearly defined as UWB types of MPAs prototypes. However, ΨU shaped MPA provides enhanced FBW, UWB of bandwidth than other UWB-MPAs. A 2 × 2 array of ΨU shaped MPAs offer the resonance of 5.26 GHz, wide band of 4.5 GHz to 5.5 GHz and FBW of 19.60. These 2 × 2 array of MPAs and equivalent dielectric breast model are validated using higher and lower dielectric strength of coupling medium which are obtained from the different tumor resolution stages. Therefore, the results are experimentally analysed in the selection of different tumor dielectric equivalent material. For experimental purpose, these test bed results are compared with healthy tissue modules. Hence, the cancer resolution stages are described by scattered mapping algorithms. These proposed MPAs based Debye test beds have been numerically analyzed using two way monostatic radar approach. This method provides the maximum sensitivity, maximum target of coverage and other related parameters. Hence, the 2 × 2 array of ΨU shaped MPA is a more efficient antenna design than other MPAs for UWB-MI system and it suitable for breast cancer diagnosis system [3,8-11].
References
- Sakthisudhan K, Thangaraj P. Survey of Radiology Clinical Methodologies for Breast Cancer’s Symptoms Detection. Res J Biotech 2015; 10: 63-71.
- Sakthisudhan K, Tamilselvan GM, Thangaraj P. Non-invasive Breast Cancer Detected by Patch Antenna Design. Res J Biotech 2014; 9: 85-91.
- Sakthisudhan K, Saravana Kumar N. Certain Study on Improvement of Bandwidth in 3GHz Microstrip Patch Antenna Designs and Implemented on Monostatic Radar Approach for Breast Cancer Diagnosis in Microwave Imaging System. J Circuit Syst Comput 2016; 25: 1-29.
- Fear EC, Stuchly MA. Microwave Detection of Breast Cancer. IEEE Transact Microwave Theor Tech 2000; 48: 1854-1863.
- Fear EC, Li Xu, Hagness SC, Stuchly MA. Confocal Microwave Imaging for Breast Cancer Detection: Localization of Tumors in Three Dimensions. IEEE Transact Biomed Eng 2002; 49: 812-822.
- Fear EC, Hagness SC, Meaney P, Okoniewski M, Stuchly MA. Enhancing Breast Tumor Detection with Near-field Imaging. IEEE Microw Mag 2002; 3: 48-56.
- Fear EC, Sill J, Stuchly MA. Experimental Feasibility Study of Confocal Microwave Imaging for Breast Tumor Detection. IEEE Microw Mag 2003; 51: 887-892.
- Salvador SM, Vecchi G. Experimental Tests of Microwave Breast Cancer Detection of Phantoms. IEEE Trans Antennas Propag 2009; 57: 1705-1712.
- Kiruthika N, Sharma SK. An Investigation on Microwave Breast Cancer Detection by Ultra-Wideband Microstrip Slot Antennas. IEEE Int Symposium Antennas Propagat 2011; 3385-3388.
- Thonglyvong D. Implementation of Active Microwave Imaging Methods to Improve Early Signs of Breast Cancer Detection. Connections Module 2007.
- Meaney PM, Fanning MW, Li Dun, Poplack Steven P, Paulsen KD. A Clinical Prototype for Active Microwave Imaging of the Breast. IEEE Transact Microwave Theor Techn 2000; 48: 1841-1853.