Research Article - Biomedical Research (2018) Artificial Intelligent Techniques for Bio Medical Signal Processing: Edition-II
Study of the relationship between EGFR mutation status and bone metastasis in advanced lung adenocarcinoma
Xiaoye Ai, Adalati Yasheng, Zhennan Zhangjia, Ying Tong and Bing Zhao*
Tumor Hospital Affiliated to Xinjiang Medical University, Urumqi, PR China
- *Corresponding Author:
- Bing Zhao
Tumor Hospital Affiliated to Xinjiang Medical University
Urumqi, PR China
Accepted date: July 02, 2017
DOI: 10.4066/biomedicalresearch.29-17-1489
Visit for more related articles at Biomedical ResearchAbstract
To investigate the relationship between EGFR gene status and bone metastasis in lung adenocarcinoma, we collected the data of 331 patients with advanced lung cancer, and the status of EGFR mutation was detected by RT-PCR. Follow-ups of these patients were performed. In these patients, the EGFR mutation rate was 52.2%. The incidence of bone metastases (54.9%) and brain metastases (29.4%) with EGFR mutant patients was higher than that of the wild-type EGFR patients. Compared with the number of metastases, EGFR mutant bone metastases were more than 2 and more, and the proportion of wild type single-site metastasis was more. The median survival of bone metastases in advanced lung adenocarcinoma was 14.7 months. Mutant EGFR group, bone metastasis group median survival in 18.2 months, no bone metastasis group median survival in 21.8 months. In the wild-type group, the median survival of the bone metastases group was 11.5 months, and the median survival in the non-bone metastases group was 15.5 months. EGFR mutations are more likely to develop bone metastasis and brain metastasis in patients with advanced lung adenocarcinoma.
Keywords
Lung adenocarcinoma, Epidermal growth factor receptor (EGFR), Bone metastasis
Introduction
In China, lung cancer has become the malignant tumor with the highest morbidity and mortality. Most patients are diagnosed with advanced lung cancer at the first-time consultancy and lose the chance to be cured by surgery. According to relevant statistics, the incidence of bone metastasis ranges from 41%-58% in patients with lung cancer [1,2].
The time interval between incidence of bone metastasis and occurrence of Skeletal-Related Event (SRE) is 9.5 months [2]. In lung adenocarcinoma of the Asian patients, gene mutations of the epidermal growth factor receptor occur in about 40%-60% [3-5]. It is reported in some researches that, the incidence rate of bone metastasis before occurrence of the Tyrosine Kinase Inhibitor (TKI) is 20% and increases to 27% after occurrence of TKI [2]. It means that the incidence rate of bone metastasis changes substantially along with the occurrence and utilization of TKI.
This study provides a retrospective analysis of correlation between EGFR mutation status and bone metastasis through collection of medical records and follow-ups of the patients treated in our hospital from 2013-2016 (Table 1).
| Mutant EGFR group | Wild-type EGFR group | P value | ||
|---|---|---|---|---|
| Bone Metastases (%) | 95 (54.91%) | 60 (37.97%) | 0.002 | |
| Number of Metastases | 1 | 16 | 21 | 0.015 |
| 2 | 36 | 23 | ||
| 3 or above | 43 | 16 | ||
| Alkaline phosphatase (mmol/L) | 136.8 | 113 | 0.011 | |
Table 1. The correlation between EGFR mutation status and incidence of bone metastasis.
Methods
Object of study and methods
The patients who confirmed with stage IV lung adenocarcinoma by pathology or cytology in the Xinjiang Tumor Hospital from 2013-2016 were selected as the objects of this study.
Relevant exclusion standards are: 1. Patients with incomplete general data; 2. The EGFR mutation status was unknown; 3. Patients with second primary tumor; 4. Patients without complete imaging data (including chest, abdomen, and pelvic cavity, skull and bone metastasis). The complete medical records of the above mentioned patients were collected, to whom the follow-up visits were performed through phone calls or medical records.
Diagnostic criteria
EGFR gene detection: Real-time quantitative fluorescent PCR technique is adopted for detection of gene status in tissues or blood of the patients.
Diagnosis of bone metastasis: With reference to the Expert Consensus on the Diagnosis and Treatment of Bone Metastasis in Lung Cancer (2014 version).
Statistical method
SSPS17.0 software is used for statistical analysis. Measurement data is represented by (x ± s), comparison among groups is provided with t-test, enumeration data is provided with χ2 test, survival analysis is provided with log-rank test, and statistical significance is recorded as P<0.05.
Result
Comparison of general data of the mutant EGFR group and the wild-type EGFR group
331 cases of patients from 2013-2016 are collected, 173 cases of patients with EGFR mutation and 158 cases of patients with wild-type, the EGFR mutation rate was 52.2%. The comparison of the two groups of patients is as shown in Table 2. In the mutant EGFR group, male patients account for 47.4%, and female patients account for 52.6% at the average age of 59.9 y old. Patients who smoke account for 29.5% and those who don’t smoke account for 70.5%. In first-time diagnosis, patients with intrapulmonary metastases account for 49.1%, patients with brain metastases account for 29.4%, patients with bone metastases account for 54.9% patients with liver metastases account for 19.7%, patients with pleural metastasis account for 43.4%, patients with adrenal metastasis account for 9.8%, and patients with metastases in other sites account for 9.2%. Patients with mutations in 19 exon deletions account for 52.6%, patients with mutations in 21 exon deletions account for 39.3% and patients with other type of mutations account for 8.1%. In the wild-type EGFR group, male patients account for 63.9%, and female patients account for 36.1% at the average age of 59.9 y old. Patients who smoke account for 52.2% and those who don’t smoke account for 47.5%. In first-time diagnosis, patients with intrapulmonary metastases account for 43.7%, patients with brain metastases account for 20.9%, patients with bone metastases account for 38.0% patients with liver metastases account for 13.3%, patients with pleural metastases account for 34.8%, patients with adrenal metastases account for 18.48%, and patients with metastases in other sites account for 11.4%. The incidence rate of brain metastases and bone metastases in the mutant EGFR group is higher than that of the wild-type EGFR group. The incidence rate of adrenal metastases is higher than that of the mutant EGFR group (P<0.05 with statistical significance).
| EGFR mutant group | Wild-type EGFR group | Total | P value | |
|---|---|---|---|---|
| Sex | ||||
| Male | 82 (47.4%) | 101 (63.9%) | 183 | 0.003 |
| Female | 91 (52.6%) | 57 (36.1%) | 148 | |
| Average age | 59.9 ± 11.8 | 59.6 ± 11.3 | - | 0.76 |
| (24-68) | (28-84) | |||
| Smoking history | ||||
| With | 51 (29.5%) | 83 (52.5%) | 134 | 0 |
| Without | 122 (70.5%) | 75 (47.5%) | 197 | |
| Metastasis site | ||||
| Inside the lungs | 85 (49.1%) | 69 (43.7%) | 154 | 0.32 |
| Brain | 51 (29.4%) | 33 (20.9%) | 78 | 0.043 |
| Bone | 95 (54.9%) | 60 (38.0%) | 155 (46.8%) | 0.002 |
| Liver | 34 (19.7%) | 21 (13.3%) | 55 | 0.12 |
| Pleura | 75 (43.4%) | 55 (34.8%) | 130 | 0.112 |
| Adrenal gland | 17 (9.8%) | 29 (18.4%) | 46 | 0.025 |
| Other | 16 (9.2%) | 18 (11.4%) | 34 | |
| EGFR mutation | ||||
| 19 | 91 (52.6%) | - | 91 | |
| 21 | 68 (39.3%) | - | 68 | |
| Others | 14 (8.1%) | - | 10 | |
| Wild-type | - | 158 | 158 | |
| Total | 173 (100%) | 158 (100%) | 331 | |
Table 2. Comparison of general data, metastasis site and EGFR gene status of the two groups of patients.
The relationship between EGFR mutation and incidence rate and number of bone metastases
The incidence rates of bone metastasis are 54.91% and 37.97% of the mutant EGFR group and wild-type EGFR group respectively (P<0.05 with statistical significance). In terms of the number of metastases, patients with two or above bone metastases in the mutant EGFR group take a larger proportion and most of the patients in the wild-type EGFR group are with single-site metastasis. The difference between the two groups is of statistical significance (P<0.05). Meanwhile, with regard to biochemical indicators, alkaline phosphatase in the mutant EGFR group and the wild-type EGFR group reaches 136.8 mmol/L and 113.0 mmol/L respectively, which indicates the difference is of statistical significance (P<0.05).
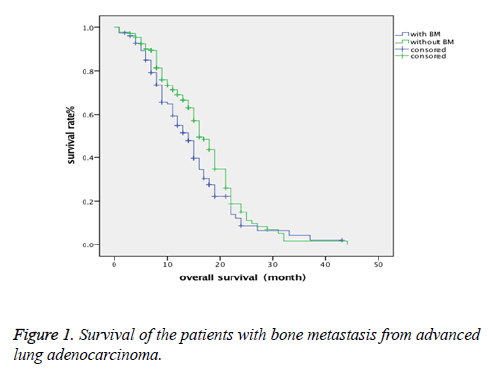
Survival situation of the patients with bone metastasis from advanced lung adenocarcinoma
Follow-up visits were paid to the 331 patients, of whom the survival analysis is given in Figure 1. The median overall survival of the patients is 14.7 months and 16.8 months respectively of those with and without bone metastasis. P=0.022<0.05, which means the difference is of statistical significance.
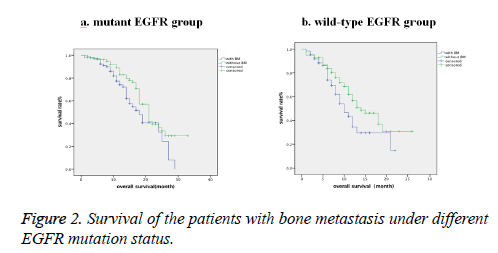
Survival situation of the patients with bone metastasis from mutant EGFR and wild-type EGFR advanced lung adenocarcinoma
Follow-up visits were paid to the patients in two group, the mutant EGFR group and wild-type group, of which, the survival analysis is as shown in Figure 2 and Table 3. In the mutant EGFR group, the median overall survival is 18.2 months and 21.8 months respectively of those with and without bone metastasis. P=0.029<0.05, which means the difference is of statistical significance. In the wild-type EGFR group, the median overall survival is 11.9 months and 15.5 months respectively of those with and without bone metastasis. P=0.04<0.05, which means the difference is of statistical significance.
| OS | With bone metastasis (month) | Without bone metastasis (month) | P value |
|---|---|---|---|
| Mutant EGFR group | 18.2 | 21.8 | 0.029 |
| Wild-type EGFR group | 11.9 | 15.5 | 0.04 |
Table 3. Survival situation of the patients with bone metastasis in the mutant EGFR group and wild-type EGFR group.
Discussion
According to the latest statistics, China is expected to have 4.292 million new cases of patients with tumor including 2.814 million cases of patients who are dead. Among all the patients, lung carcinoma is with the highest incidence rate and mortality rate [6]. Most of the patients are already in terminal stage at confirmed diagnosis, and of whom, the five-year survival rate is less than 15% [7]. With the constant advancement in genetics and genomics, it have been gradually found and proved that the key factor leading to lung cancer is gene mutation. Among those with lung adenocarcinoma, driver genes are detected in 60% to 70% of the patients [8]. These driver genes include EGFR, KRAS, HER2, PIK3CA, BRAF, MET mutations and ALK, ROS1 and RET gene rearrangement. EGFR is a kind of cell-surface membrane protein receptor and a member of the epidermal growth factor ErbB family. When EGFR is connected with corresponding signal molecule, dimers would form among the receptor molecules, and at the same time, mutual phosphorylation of intracellular tyrosine kinases is started and intracellular cascade signalling pathways are activated, thus, a series of intracellular morphological changes are caused [9]. It is shown by relevant studies that, excessive expression of EGFR genes is closely related to proliferation, invasion and metastasis of lung cancer [10].
According to relevant statistics, EGFR mutation rate is as high as 40%-60% of Asian patients with lung cancer. EGFR-TKI treatment helps prolong the overall survival of advanced lung cancer to 21.6-21.6 months [11,12]. In the study in this paper, 331 cases of patients were collected, among whom, the EGFR mutation rate was 52.2%, which means the data are basically identical with the that obtained by Liu et al. [13,14]. Among all the objects of the study, female patients and non-smoking patients are the advantaged group, which is similar to the previous research results. It is also found the patients in the mutant EGFR group are more likely to develop bone metastases (54.9%) and brain metastases (29.4%).
The incidence rate of bone metastasis has changed since the clinic application of EGFR-TKI treatment. In the study in this paper, the incidence rate of bone metastasis is 46.8% and 54.9% in the mutant EGFR group, which is higher than that of the wild-type EGFR group. In addition, most of the patients in the mutant EGFR group are with multi-sites metastases and a larger proportion of the patients in the wild-type EGFR group are with single-site metastasis. However, the reason is still unknown at present, maybe EGFR signals play an important role in the process of tumor metastasis. In terms of lung cancer, EGFR signals are closely related to MET, which plays an very important role in angiogenesis and regulation of cell proliferation and haematogenous metastasis [15,16].
The median overall survival of the patients with bone metastasis is 14.7 months, which is shorter than that of the patients without bone metastasis. Thus, it can be seen that, bone metastasis often leads to poorer life quality and shorter period of survival of patients. The skeletal-related events caused by bone metastasis and the pain brought by treatment jointly severely affect the life quality of patients. On this ground, it is especially important to actively prevent and cure bone metastasis and skeletal-related events while controlling primary disease.
In EGFR mutation group, the median overall survival of the patients with bone metastasis and without bone metastasis is 18.2 months and 21.8 months respectively. In the wild-type EGFR group, the median overall survival of the patients with bone metastasis and without bone metastasis is 11.9 months and 15.5 months respectively. It is regarded that such result may have something to do with utilization of the TKI drugs which prolong survival of the patients in the mutant EGFR group.
Conclusion
To sum up, patients with bone metastasis of lung cancer have a shorter period of survival and easily develop SRE, which seriously affect the life quality of them. The incidence rates of bone, brain and adrenal metastasis of the patients with mutant EGFR are relatively higher. Thus, for patients with mutant EGFR, special attention shall be paid to prevention and treatment of bone metastasis during control of primary disease.
Acknowledgement
The authors would like to give their thanks to Natural Science Foundation of Xinjiang Uyghur autonomous region (2016D01C368) for their financial support.
References
- Tsuya A, Kurata T, Tamura K, Fukuoka M. Skeletal metastases in non-small cell lung cancer: a retrospective study. Lung Cancer 2007; 57: 229-232.
- Nobuyuki K. Prospective study on the incidence of Bone Metastasis (BM) and Skeletal-Related Events (SREs) in patients (Pts) with stage IIIB and IV lung cancer-Csp-HOR 13. J Thorac Oncol 2014; 9: 231-238.
- Kohno T, Tsuta K, Tsuchihara K. RET fusion gene: translation to personalized lung cancer therapy. Cancer Sci 2013; 104: 1396-1400.
- Shi Y, Au JS, Thongprasert S. A prospective, molecular epidemiology study of EGFR mutations in Asian patients with advanced non-small-cell lung cancer of adenocar-cinoma histology (PIONEER). J Thorac Oncol 2014; 9: 154-162.
- Uramoto H, So T, Nagata Y. Correlation between HLA alleles and EGFR mutation in Japanese patients with ade-nocarcinoma of the lung. J Thorac Oncol 2010; 5: 1136-1142.
- Wanqing C, Rongshou Z, Peter D. China statistics in China. Cancer J Clin 2016; 66: 115-132.
- Einger DS, Akerley W, Bepler G. Non-small cell lung cancer. J Natl Compr Canc Netw 2010; 8: 740-801.
- Pikor LA, Ramnarine VR, Lam S. Genetic alterations defining NSCLC subtypes and their therapeutic implications. Lung Cancer 2013; 82: 179-189.
- Herbst RS. Review of epidermal growth factor receptor biology. Int J Radiat Oncol Biol Phys 2004; 59: 21-26.
- Goto K, Nishio M, Yamamoto N. A prospective, phase II, open-label study (JO22903) of first line erlotinib in Japanese patients with epidermal growth factor receptor (EGFR) mutation positive advanced non-small-cell lung cancer(NSCLC). Lung Cancer 2013; 82: 109-114.
- Yang CH, Fukuoka M, Mok TS. Final overall survival results from a phase III randomized, open-label, first-line study of gefitinib vs. carboplatin/paclitaxel in clinically selected patients with advanced non-small-cell lung cancer in Asia (IPASS). Ann Oncol 2010; 21.
- Tetsuya M, Satoshi M, Yasushi Y. Updated overall survival results of WJTOG 3405, a randomized phase III trial comparing gefitinib (G) with cisplatin plus docetaxel (CD) as the first-line treatment for patients with non-small cell lung cancer harbouring mutations of the epidermal growth factor receptor (EGFR). ASCO Meeting Abstracts 2012; 30: 7521.
- Liu Y, Liu J, Chen Y. Mutation of epidermal growth factor receptor and clinicopathologic features of patients with lung cancer. Gungdong Med 2016; 37: 1365-1368.
- Yang C, Xu W, Feng Q. Analysis on EGFR mutation detection of non-small cell lung cancer in different areas in Yunnan province. Med J Nat Defending Forces Southwest Chin 2016; 26: 4-7.
- Lichtenberger BM, Tan PK, Niederleithner H. Autocrine VEGF signaling synergizes with EGFR in tumor cells to promote epithelial cancer development. Cell 2010; 140: 268-279.
- Barr S, Thomson S, Buck E. Bypassing cellular EGF receptor dependence through epithelial-to-mesenchymal-like transitions. Clin Exp Metastasis 2008; 25: 685-693.