- Biomedical Research (2010) Volume 21, Issue 4
Study of lipid profile and oxidative stress in chronic renal failure
Sumathi M.E.1*, Manjunath M Tembad2, Jayaprakash murthy D.S.3, Preethi B.P41Deptartment of Biochemistry, Sri Devraj Urs Medical College,Tamaka, Kolar, India
2Deptartment of Biochemistry, J.J.M medical college, Davangere, India
3Deptartment of Biochemistry, J.J.M medical college, Davangere, India
4Deptartment of Biochemistry, J.J.M medical college, Davangere, India
- *Corresponding Author:
- Sumathi M.E
Deptartment of Biochemistry
Sri Devraj Urs Medical College
Tamaka, KOLAR. Karnatak,India
E-mail: drsuma_bio@yahoo.co.in
Accepted May 27 2010
Abstract
Chronic renal failure is a debilitating disease which leads to many complications, most com-mon being cardiovascular. Hence this study was undertaken to know the risk of cardiovas-cular morbidity in CRF patients. The levels of serum TG, TC, LDL-C, VLDL-C, TC/HDL-C and LDL-C/HDL-C ratio were significantly increased and HDL-C was significantly de-creased in cases when compared to controls. Serum TG, TC, VLDL-C and HDL-C are sig-nificantly increased in conservatively managed patients than hemodialysis patients. Serum MDA was significantly increased and SOD was significantly decreased in cases when com-pared to controls. These changes were more pronounced in hemodialysis patients when compared to conservatively managed patients. We also did the correlation between lipid and oxidative stress parameters, in which serum MDA was positively correlated with all the lipid parameters except HDL-C and serum SOD was negatively correlated with all lipid parame-ters except for HDL-C. This study suggests that increased lipoproteins along with increased oxidative stress leads to accelerated atherosclerosis in CRF patients.
Keywords
Chronic renal failure; Dyslipidemia; Oxidative stress; Malondialdehyde; Superoxide dismutase.
Introduction
Chronic Renal Failure (CRF) is the state which results from a permanent and usually progressive reduction in renal function, in a sufficient degree to have adverse con-sequences on other systems. [1] In the developing coun-tries, the awareness and burden of CRF on society has been highlightened during last decade. In India, incidence of CRF is not well documented because of lack of na-tional registry and data regarding its incidence. It has been estimated that the prevalence of CRF in India may be up to 785 people per million populations. [2]
Chronic Renal Failure leads to many complications over a period of time. The most common include cardiovascular, cerebrovascular and peripheral vascular diseases. Deaths due to cardiovascular complications are 4-20 fold higher in CRF patients than any other cause in general popula-tion.[3] These complications are due to many metabolic and endocrinal disturbances among which dyslipidemia is one of the constant feature of CRF. Lipid abnormalities can be detected as early as renal function begins to de-cline (Glomerular Filtration Rate (GFR) < 50ml/min) but the type and severity vary among different patients. [3,4].
CRF patients are also subjected to enhanced oxidative stress due to reduced antioxidant systems and increased prooxidant activity.[5] During this process polyunsatu-rated fatty acids, present in cell membrane are oxidized in vivo to form aldehydes of variable chain length like malondialdehyde (MDA). This lipid peroxidation product can structurally alter DNA, RNA, body protein and other biomolecules.[6]
Lipid abnormalities and enhanced oxidative stress in CRF patients, accelerates the process of atherosclerosis result-ing in cardiovascular complications. Hence this study was undertaken to assess the alterations in the serum lipid pro-file and determination of oxidative stress to know the risk of development of cardiovascular complications in CRF patients.
Materials and Methods
A case control study of serum lipid profile and oxidative stress in chronic renal failure patients were carried out from February 2007 to February 2008. Both controls and cases of CRF attending OPD and dialysis units were se-lected from Bapuji hospital and Chigateri general hospi-tal. Both these hospitals are attached to teaching institute J.J.M medical college, Davangere. Each gave an informed consent and this study was approved by the ethical and research committee of J.J.M Medical college to use hu-man subjects in the research study.
A total number of 110 subjects were participated in the study, of which 60 clinically diagnosed cases of chronic renal failure > 20 years of age were included. Among 60 CRF cases, 30 were on maintenance hemodialysis for a period of 5 months to 3 years. These patients were un-dergoing hemodialysis for 3-4 hours three times a week. Remaining 30 patients were on conservative line of treatment.
Control group consists of 50 age and sex matched normal healthy adults without any major illness. Patients with diabetes mellitus, familial hyper lipoproteinemia and who are on hypolipidemic drugs were excluded from the study by asking family and past history.
About 5ml of venous blood was drawn under aseptic pre
Results
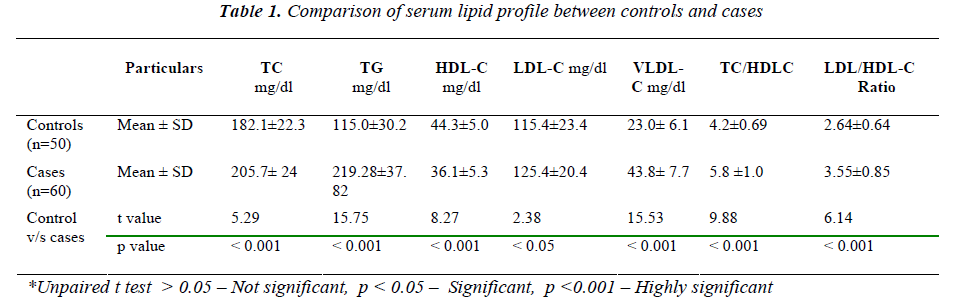
Table 1 shows comparative analysis of serum lipid profile between controls and cases. The mean values of TC, TG, LDL-C, VLDL-C, TC/HDL-C and LDL/HDL ratio are increased in cases when compared to controls except HDL-C.
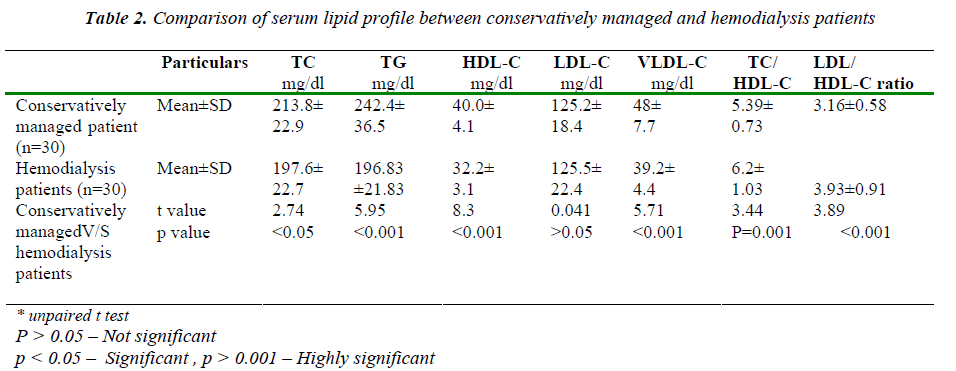
Table 2 shows the comparative analysis of serum lipopro-tein between conservative management and hemodialysis patients. When compared to hemodialysis patients, the mean values of TC, TG, HDL-C, LDL-C and VLDL-C are increased in conservatively managed patients and this difference is statistical significance (p < 0.001) except LDL –C which was not significant (p < 0.05).The mean values of TC/HDL-C and LDL-C/ HDL-C ratios are in-creased in hemodialysis patients when compared to cons- cautions in a sterile bulb from selected subjects after a period of overnight fasting of 12 hrs, serum was separated by centrifugation and used for analysis. Serum lipid pro-file which includes triglycerides (TG), total cholesterol (TC), high density cholesterol (HDL-C) were estimated by enzymatic method and serum low density cholesterol (LDL-C) and very low density cholesterol(VLDL-C) were calculated by using Friedwald fomula.[7] Serum MDA (malondialdehyde) by thiobarbituric acid (TBA) method [8] and Superoxide dismutase by Marklund and marklund method. [9]
Lipid profile was analyzed by using ERBA kits in micro- lab semi-autoanaylzer of MERCK Company. All the re agents used in the estimation were of analytical grade.
Statistical Analysis
Independent T test was done to compare means and pear sons correlation was done to correlate lipid profile and oxidative stress parameters. All the statistical analysis was done by using SPSS software.
ervatively managed patients and it is statistically signifi-cant
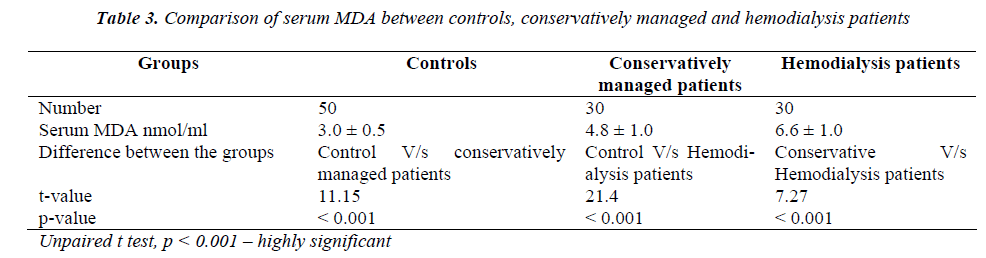
Table 3 shows the comparative analysis of serum MDA between controls and cases. When compared to controls, both conservatively managed and hemodialysis patients showed significant increased levels of MDA (p < 0.001) and the levels of MDA are significantly increased in hemodialysis patients when compared to conservatively managed patients (p < 0.001).
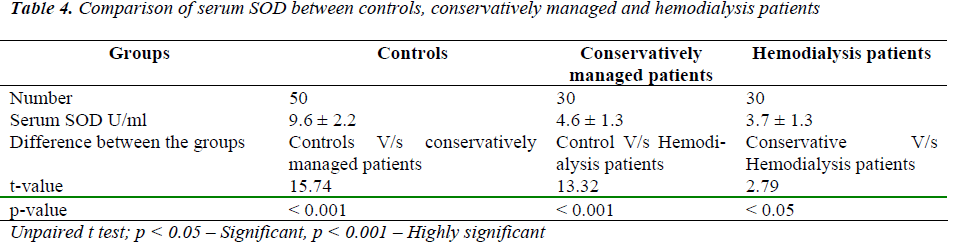
Table 4 shows comparative analysis of serum SOD levels between controls and cases. Mean values of SOD are de-creased in both conservatively managed patients and hemodialysis patients when compared to controls. SOD level is decreased markedly in hemodialysis patients when compared to conservatively managed patients (p < 0.001).
hemodialysis patients when compared to controls. SOD level is decreased markedly in hemodialysis patients when compared to conservatively managed patients (p < 0.001).
Discussion
Disorders of lipoprotein metabolism, imbalance between generation of free radicals and antioxidant defense system during uremia and dialysis are important mechanisms of atherogenesis in CRF.
The mean value of triglycerides is significantly increased in cases when compared to controls. This result is accor-dance with studies done by S M Alam et al [10], Bharat Shah et al [11], P Lee et al [12] and Ziad A Massy [13] . Hypertriglyceridemia is a common feature of CRF. Pres-ence of insulin resistance in renal failure activates hor-mone sensitive lipase causing increased FFA which stimulates the production of apoB-100 containing lipopro-teins like VLDL leading to hypertriglyceridemia. Several authors also suggested that hypertriglyceridemia in CRF may be due to defective metabolism of TG rich lipopro-teins by lipoproprotein lipase(LPL) and hepatic lipase [14,15,16]
The mean value of TC is significantly increased in cases when compared to controls. This is in accordance with the study of M.M. Avram et al [17], P.O Attman et al [18] and Mayumi Tsumura et al [19]. Many studies have re-ported variable results. A study done by B.S Das et al.,[20] observed decreased levels of TC in CRF patients. The reason for this decrease may be due to reduced food intake. CRF is associated with hypercholesterolemia which is due to associated proteinuria and renal insuffi-ciency per se. Proteinuria leads to alteration in gene ex-pression for HMG-CoA reductase resulting in increased activity of HMG-CoA reductase leading to hypercholes-terolemia. [14].
In our study mean value of HDL-C is significantly de-creased in CRF patients when compared to controls. Many studies conducted by Ziad A Massy et al [13], BS. Das et al [20] and Tetsuo Shoji et al [21] have also ob-served the same results. The reason for decreased concen-tration of HDL-C in CRF is not fully understood. It may be due to decreased activities of LPL, hepatic triglyceride lipase (HTGL), lecithin cholesterol acyl transferase (LCAT) and increased concentration of cholesterol ester transfer protein (CETP) and decreased apolipoprotein concentrations.[14]
This study included 30 conservatively managed patients and 30 hemodialysis patients. The mean values of TC, TG, LDL-C, VLDL-C, TC/HDL-C and LDL/HDL-C in conservatively managed patients are significantly in-creased when compared to hemodialysis patients except for LDL-C. This is in accordance with the study of SM Alam et al [10], Bharat Shah et al [11] and Mayumi Tsu-mura et al [19]. The cause for the decrease in lipoprotein concentrations could be due to removal of lipoproteins by repeated dialysis and decreased peripheral resistance to insulin after initiation of dialysis [11].
MDA is a lipid peroxidation product which is formed dur-ing oxidation process of PUFA by reactive oxygen spe-cies. MDA is the sensitive marker of lipid peroxidation. MDA level is significantly elevated in hemodialysis pa-tients when compared to conservatively managed patients. This is in accordance with study of C.M Loughrey et al [22], A. Marjani [23] and Talia Weinstein et al [24]. Al-though hemodialysis leads to improvement of several bio-chemical parameters like creatinine, urea levels and plasma lipid patterns, but it can cause harmful atherogenic effects. The increase in lipid peroxidation resulting from hemodialysis could be provoked by bio incompatibility of dialysis membrane. When cells come in contact with the dialyzer membrane leads to sensitization of cell mem-brane components leading to compliment activation which cause formation of other reactive oxygen species which will initiate peroxidation of PUFA. [23,24]
SOD functions as a scavenger of superoxide radical in the body. Mean value of SOD is significantly decreased in hemodialysis (p value < 0.05) patients when compared to conservatively managed patients. This is in accordance with the study of A. Marjani [23], M Sasikala et al [25] and M. Nouri et al [26]. Mechanisms involved in de-creased serum SOD activity in CRF patients may be due to increased production of ROS such as H2O2 which is known to suppress SOD activity. Decreased SOD activity among hemodialyzed patients could be due to decreased levels of Cu2+ and Zn2+ as they are cofactors of cytoplas-mic SOD. Increased lipid peroxidation causes consump-tion of antioxidant enzymes, particularly in hemodialysis patients, may be also one of the reasons for decreased SOD levels. [27]
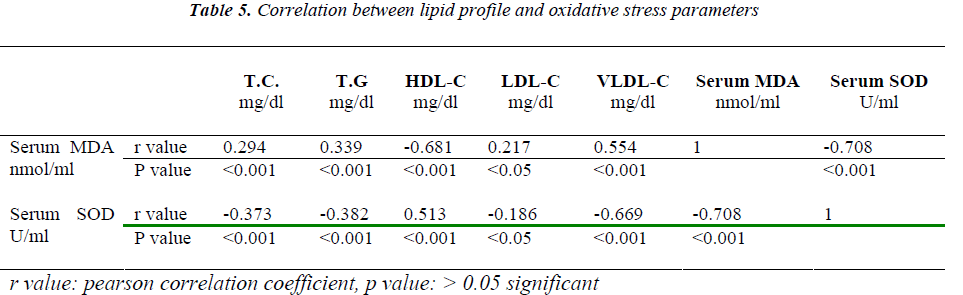
We also compared the serum lipids with oxidative stress parameters by using pearson correlation. We observed that serum MDA positively correlates with TC, TG, LDL, VLDL and negatively correlates with HDL and SOD. With respect to SOD it is vice versa. Thus dyslipidemia and oxidative stress may act in synergy leading eventually to accelerated atherosclerosis.
Conclusion
This study suggests that there is increased risk of cardio-vascular complications in CRF patients particularly in patients who are on hemodialysis. The altered concentra-tion of serum lipoproteins, MDA and SOD leads to accel-erated atherosclerosis in CRF patients. Hence by advising proper diet or drugs lipid abnormalities will be brought to normal levels.
Acknowledgement
It is a great honor to express my gratitude to my beloved teacher Dr. D.S JAYAPRAKASH MURTHY,B.Sc.,MD., Professor and Head, Department of Biochemistry, for his suggestion and constant source of inspiration throughout my post graduation course. It is with this sense of heart-felt gratitude and appreciation to my guide and teacher, Professor . Manjunath M. Tembad., Department of Bio-chemistry, J.J.M. Medical College, Davangere for the preparation of this work.
References
- Winearls CG. Chronic Renal failure In : Warrell DA, Cox TM, Firth JD, Benz EJ, Eds. Oxford text book of Medicine 4th edn, Vol 3. New York, Oxford University press; 2003: 263-278.
- Abraham G, Moorthy AV, Aggarwal V. Chronic kid- ney disease : A silent epidemic in Indian subcontinent – strategies for management. J Indian Med Assoc 2006; 104 (12): 689-91.
- Oda H, Keane WF. Lipid abnormalities in end stage renal disease. Nephrol Dial Transplant 1998; 13 (Suppl 1): 45-49.
- Wanner C. Importance of hyperlipidaemia and therapy in renal patients. Nephrol Dial Transplant 2000; 15 (Suppl 5): 92-96.
- Locatelli F, Canaud B, Eckardt KU, Stenvinkel P, Wanner C, Zoccali C. Oxidative stress in end-stage re- nal disease: an emerging threat to patient outcome. Nephrol Dial Transplant 2003; 18: 1272-1280.
- Daschner M, Lenhartz H, Botticher D, Schaefer F, Wollschlager M, Mehls O et al. Influence of dialysis on plasma lipid peroxidation products and antioxidant lev- els. Kidney Int 1996; 50: 1268-1272.
- Nader R, Warnick GR. Lipids, lipoproteins, apolipo- proteins and other cardiovascular risk factors. In : Bur-tis CA, Ashwood ER and Bruns DA, eds. Tietz textbook of clinical chemistry and molecular diagnostics, 4th edn. New Delhi Elsevier Co 2006; 916-952.
- Dillard, Kunert KJ, Tappel. Effects of vitamin E,ascorbic acid and mannitol on Alloxan-induced lipid peroxidation in rats. Arch Biochem Biophysics 1982; 216 (1): 204-212.
- Nandi A, Challergee JB. Assay of superoxide dismu- tase activity in animal tissues. J Biosci 1988; 13 (3): 305-315.
- Alam SM, Bhatt AK. Abnormal lipoprotein in uraemic patients treated conservatively and by maintenance hemodialysis. JAPI 1991; 39 (2): 170-171.
- Shah B, Nair S, Sirsat RA, Ashavaid TF, Nair KG.Dyslipidemia in patients with chronic renal failure and in renal transplant patients. J Prostgrad Med 1994; 40 (2): 57-60.
- Lee P, O’Neal D, Murphy B, Best J. The role of ab- dominal adiposity and insulin resistance in Dyslipide- mia of chronic renal failure. Am J Kidney Dis 1997; 29 (1): 54-65.
- Massy ZA, Khoa TN, Lacour B, Descamps-Latscha, Man NK, Jungers P. Dyslipidemia and the progression of renal disease in chronic renal failure patients. Nephrol Dial Transplant 1999; 14: 2392-2397.
- Vaziri ND. Dyslipidemia of chronic renal failure: The nature, mechanisms and potential consequences. Am JPhysiol Renal Physiol 2006; 290: 262-272.
- Ma KW, Greene EL, Raij L. Cardiovascular risk fac- tors in chronic renal failure and hemodialysis popula- tions. Am J Kidney Dis 1992; 19 (6): 505-513.
- Prinsen BHCMT, Velden MGMDS, de Koning EJP, Koomans HA, Berger R, Rabelink TJ. Hypertriglyc- eridemia in patients with chronic renal failure : possible mechanisms. Kidney Int 2003; 63(84): S121-S124.
- Avram MM, Goldwasser P, Burrell DE, Antignani A, Fein PA, Mittman N. The uremic dyslipidemia : a cross-sectional and longitudinal study. Am J Kidney Dis 1992; 20 (4): 324-335.
- Attman PO, Alaupovic P, Tavella M, Gibson CK. Ab- normal lipid and apolipoprotein composition of major lipoprotein density classes in patients with chronic re-nal failure. Nephrol Dial Transplant 1996; 11: 65-69.
- Tsumura M, Kinouchi T, Ono S, Nakajima T, KomodaT. Serum lipid metabolism abnormalities and change in lipoprotein contents in patients with advanced-stage re- nal disease. CCA 2001; 314: 27-37.
- Das BS, Misraf SK, Rao VM, Satpathy SR, Bose TK. Serum lipid in chronic renal failure. JAPI 1984; 32 (12): 1019-1021.
- Shoji T, Nishizawa Y, Nishitani H, Yamakawa M,Mori H. Impaired metabolism of high density lipopro- tein in uremic patients. Kidney Int 1992; 41: 1653-1660.
- Laughrey CM, Young IS, Lightbody JH, McMaster D, McNamee PT, Trimble ER. Oxidative stress in hemo- dialysis Q J Med 1994; 87: 679-683.
- Marjani A. Clinical effect of hemodialysis on plasma lipid peroxidation and erythrocyte antioxidant enzyme activities in Gorgan (South East of Caspian Sea). Ind J Nephrol 2005; 15: 214-217.
- Weinstein T, Chagnac A, Korzets A, Boaz M, Ori Y, Herman M et al. Hemolysis in hemodialysis patients : evidence for impaired defense mechanisms against oxi-dative stress. Nephrol Dial Transplant 2000;15: 883- 887
- Sasikala M, Subramanyam C, Sadasivudu B. Early oxidative change in low density lipoproteins during progressive chronic renal failure. IJCB 1999; 14 (2):176-183.
- Nauri N, Nobar MR, Argani H, Rokhforooz. Superox- ide dismutase and glutathione peroxidase in hemodia- lyzed patients and transplant recipient and their rela-tionship to osmotic fragility. Med J Islam Acad Sci1999; 12 (2): 33-38.
- Toborek M, Wasik T, Drozdz M, Klin M, Magne K, Grzebieniak EK. Effect of hemodialysis on lipid per- oxidation and antioxidant system in patient with chronic renal failure. Metabolism 1992; 41 (11): 1229-1232.