Research Article - Journal of Public Health Policy and Planning (2023) Volume 7, Issue 4
Strategy for the fight against HIV within community-based distribution sites for the use of male and female condoms for post-COVID 19 resilience of key populations in a post-conflict country.
Benjamin Muma Makiala*, Dr. Arlant Kalombo, Dr. Diego Mbiti, Brunette Nsundi, Eva Bushabu, Nlandu Bakebo Chris, Tshilomba Kanda Rolonde
Department of Environmental and Sustainable Development, Institute Superior of Rural Development of Mbeo, Kinshasa, Democratic Republic of the Congo
- Corresponding Author:
- Benjamin Muma Makiala
Department of Environmental and Sustainable Development
Institute Superior of Rural Development of Mbeo
Kinshasa, Democratic Republic of the Congo.
E-mail: benjamin2012muma@gmail.com, nnk873@student.bham.ac.uk
Received: 27-Jun-2023, Manuscript No. AAPHPP-23-104032; Editor assigned: 01-Jul-2023, PreQC No. AAPHPP-23-104032 (PQ); Reviewed: 12-Jul-2023, QC No. AAPHPP-23-104032; Revised: 24-Jul-2023, Manuscript No. AAPHPP-23-104032 (R); Published: 29-Jul-2023, DOI: 10.35841/aaphpp- 7.4.190
Citation: Makiala M B. Strategy for the fight against HIV within community-based distribution sites for the use of male and female condoms for post-COVID 19 resilience of key populations in a post-conflict country. J Public Health Policy Plan. 2023;7(4):190
Introduction
Coronavirus disease 2019 (COVID-19) has spread rapidly around the world since first reports from Wuhan, China in December 2019, and the outbreak was declared a pandemic by WHO on March 12, 2020. About 37 .9 million people living with HIV are at risk of infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes COVID-19. Although some international institutions, in collaboration with governments and community partners, are working to maintain the provision of HIV-related services to people living with HIV, the COVID-19 pandemic presents several obstacles and challenges for the continuum of HIV care:
• First, the implementation of quarantine, social distancing and community confinement measures has reduced access to routine HIV testing, which calls into question the achievement of the first UNAIDS 90-90-90 target in the world, that 90% of all people living with HIV will know their HIV status. HIV testing is the essential first step towards entering the continuum of HIV care. Even with the availability of HIV self-test kits in some areas, testing remains a big challenge in settings where access to these kits is limited. Therefore, increased efforts are needed to increase access and facilitate testing.
• Second, timely linkage to HIV care could be hampered during the COVID-19 pandemic. People living with HIV who should have started antiretroviral therapy (ART) in hospital may be deterred or delayed because hospitals are busy treating patients with COVID-19. Additionally, as many public health authorities around the world are focused on controlling COVID-19, resource allocation for HIV care may be reduced and circumstances surrounding the continuum of HIV care may deteriorate. 'aggravate.
• Third, the COVID-19 pandemic could also hamper the continuation of ART. Hospital visits could be restricted due to the implementation of city lockdowns or traffic controls. UNAIDS and the BaiHuaLin Alliance of People Living with HIV, with support from the Chinese National Center for AIDS/STD Control and Prevention, conducted a survey of people living with HIV in China in February 2020. 5, 6 of this population, 32.6% were at risk of stopping ART and about 48.6% did not know where to obtain antiviral drugs in the near future. People living with HIV facing discontinuation of ART could not only experience deterioration in their physical health, but also experience severe psychological pressure [1].
As UN-AIDS urges all actors around the world to ensure that the response to HIV is integrated into recovery efforts from the COVID-19 pandemic as well as other emergencies and crises in humanitarian contexts to benefit young people [2].
We are interested in facing these various obstacles and this recommendation by the attraction expressed by the actors of the fight against HIV AIDS at the beginning of the year 2023 which expresses a concern for the scientific event of mark which brings together the scientists of the world at this 32nd Canadian Congress on HIV/AIDS Research (CAHR 2023) within which is being held today in Quebec from April 27 to 30, 2023 whose Scientific Program Committee has chosen as the central theme of the congress: “Boomerang effect: From HIV to SARS-CoV2 and back” [3].
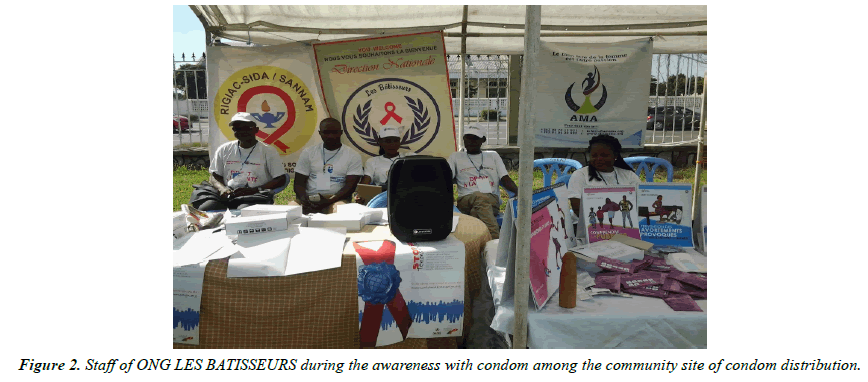
As a response to this vibrant internationally renowned scientific appeal, the NGO LES BATISSEURS, a non-governmental organization which was created on March 22, 1994 following surveys carried out among women in the health zone of the FUNA at the time (Kingabwa) whose mission is to promote public health actions through sustainable development actions in favor of children and women as well as the community, whose vision is to have a community in a world where everyone has the right to health and sustainable development [4]; proposes to make its modest contribution around the boomerang effects in the context of socio-behavioral contributions around a discussion entitled: “Strategy for the fight against HIV within community-based distribution sites for the use of male and female condoms for post-COVID 19 resilience of key populations in a post-conflict country” [5].
Title describes the boomerang effects taking into account the themes of this congress, namely: people of African, West Indian and black origins, children and adolescents, living with HIV, etc.
Indeed such as is notified the cries of alarm of the Actors of the ground of fight against the HIV which describes at the present time how many figures which are not good and they make fear the worst with the associations of fight against the AIDS. The Covid-19 pandemic has caused a significant drop in human immunodeficiency virus (HIV) testing. With 5.2 million HIV serologies carried out in laboratories, screening activity, which had increased between 2013 and 2019, fell by 14% between 2019 and 2020, reveals Public Health France (SPF) in a press release, Tuesday, November 29. In addition, between March 2020 and April 2021, the number of blood tests fell by 16% compared to what was expected, the National Agency for Research on AIDS and Viral Hepatitis (ANRS) was already alarmed in a report. Published in September. This deficit was not offset by sales of self-tests, which fell by 22% over the same period. Result: the number of new HIV-positive people put on treatment fell by 20% in one year.
This situation alarms Florence Thune, Managing Director of the Sidaction association, but also all those involved in the fight against AIDS in general, because we fear that we are once again witnessing an epidemic rebound in the short and medium terms by his statement: “We are extremely concerned, because screening is an essential tool in controlling the epidemic: a correctly treated HIV-positive person obtains a so-called undetectable viral load, as it is so low in the blood. In concrete terms, it no longer transmits HIV. First and foremost, this means knowing your serological status [6].
Indeed, making all these cries of alarm ours, it is appropriate to specify that our contribution is a fruit of the social actions emanating from the prevention of HIV and the psychosocial care of key populations in the Democratic Republic of Congo (DRC), a country that experienced its first cases of HIV in 1983 and, like many developing countries, has faced a massive security challenge in the face of Rwandan-style genocidal aggression for more than 25 years.
Country with a generalized epidemic with a prevalence of HIV infection estimated at 1.2% in the general population in 2017, it is higher in women (1.6%) than in men (0.6%) with disparities in urban areas (1.6%) than in rural areas (0.9%)
The DRC is also one of 13 countries facing the challenges of tuberculosis and HIV/TB co-infection at the same time. In 2015, the WHO estimated the incidence at 325 cases/100,000 inhabitants. The prevalence at 532 cases/100,000 inhab, while the HIV-TB incidence was 324 cases per 100,000 inhab in 2014. (PNDS 2016-2020) [7].
According to Spectrum v5.755 2019 estimates, the number of new HIV infections increased from 24,089 cases in 2014 to 18,573 cases in 2018 in the general population and from 3,032 to 2,353 cases in children aged 10 – 19 years.
The evolution of the incidence of HIV among adults aged 15 to 49 in the DRC evolves in sawtooth from 2010 to 2019 with a slight increase until 2021 (Graph 1).
Notes that new HIV infections are reduced between 2010 and 2018, going from 30,621 to 18,573, i.e. a 39% reduction. Projections show us that new infections can be reduced by 60% between 2010 and 2023 with the development of an acceleration plan which requires mobilization of additional resources, political commitment at the national level by implementing the Fast - UNAIDS track [8].
Also starting from the new incidences of other studies as revealed to us by the Canadian Agency which estimates that out of 1,520 new infections (varying between 870 and 2,260) were contracted in Canada in 2020, which represents a slight decrease compared to the 2018 estimate (1,760; range of 1,360 and 2,190).
The estimated incidence rate for the total Canadian population for 2020 was 4.0 per 100,000 population (from 2.3 to 6.0 per 100,000 population), which represents a slight decrease from the 2018 estimate (4.7 per 100,000 population; 3.7 to 5.9 per 100,000 population)
The observed decrease in new HIV infections in 2020 may have been influenced by reduced access to HIV testing services due to HIV:
The external condom: is called male condom, a sheath of polyurethane, latex or polyisoprene covering the penis during sexual intercourse. There are many varieties and brands of external condoms [9].
The internal condom: is called condom penetrating the female vagina, is a cylindrical bag of polyurethane or nitrile. It was designed for vaginal sex, but can also be used for anal sex.
The cylindrical pocket is open on one side and closed on the other, and includes a flexible ring at each end. The ring at the closed end is used to insert the condom into the vagina or anus and hold it in place. The ring at the open end of the cylindrical pouch remains outside the vagina or anus [10].
Taking into account the different conceptual approaches, starting from our continual descent into the field, our understanding of the community distribution sites of female and male condoms in acronym SDCP evolve in the health zones composed of individuals who evolve into common interest groups with problems. common, living or sharing a common land where either the common health facilities (FOSA) who find themselves faced by a common challenge or challenges which they are forced to reverse the trend of the situation, of calamity, of the pandemic experienced at the start . Compared to what Gabriel Gérard defines, on the objective or subjective level of the term, these dynamics of objectification and subjectification shape social spaces affected by Covid-19, from a health and political point of view. In the history of the fight against AIDS, the polysemous term “community” has historically been used to define the social groups affected, objectively and subjectively, by the virus. In activist circles, we often speak of the "AIDS community", a vague but powerful notion that synthesizes the collective experience represented by the mobilization of patients and their relatives, but also of caregivers or researchers against this epidemic.
In public health, “communities” refer to social groups that share characteristics (behaviour’s, identities, discrimination, violence, etc.) that make them potentially vulnerable to HIV. The fight against AIDS has also seen the development of unprecedented epistemic communities, bringing together researchers and patients. And we could speak, in symmetry, of communities of “indifference” to describe the disinterest or hostility of some of the decision-makers [11].
We note that among these various analyses as well as the challenges that the communities are confronted with by the serious problems and unfortunate consequences caused by HIV in conjunction with covid-19, which should be noted, falls in the efforts undertaken in the psychological, social comfort and economy of several communities.
Reason why boomerang effects understood as the effect that designates a psychological, political or economic mechanism, where an action leads to the opposite consequence of that sought [12] hence the impact of HIV associated with that of COVID19 causes regressive back effects to the progress of economies, politics and the psychology of humans within the communities of the countries of the world.
Despite this conceptual analysis, we note that thanks to the boomerang effects of SARS-COV2 unintended consequences, a global shortage of condoms is looming due to the many factories and distribution circuits paralyzed, warned the sector's leading manufacturer: according to the UN, nearly half of the inhabitants of the planet are now confined to their homes and businesses deemed “non-essential” are closed in many countries Lucie Oriel tells us [13].
Method
Our methodological approach makes use of a few studies or surveys carried out in the field, such as recently in the USA the survey was conducted online from April to May 2020. The GBMSM were recruited through advertisements broadcast on social network platforms, recruiting a sample of 518 GBMSM. The analysis considers three changes in self-reported measures of sexual behaviour: number of sex partners, number of anal sex partners, and number of anal sex partners not protected by pre-exposure prophylaxis (PrEP) or condoms. About two-thirds of the sample said they believed it was possible to contract COVID-19 through sex, with anal sex reported as the least risky sexual act. Men generally did not feel it was important to reduce their number of sexual partners during COVID-19, but reported moderate willingness to have safer sex during COVID-19 [14].
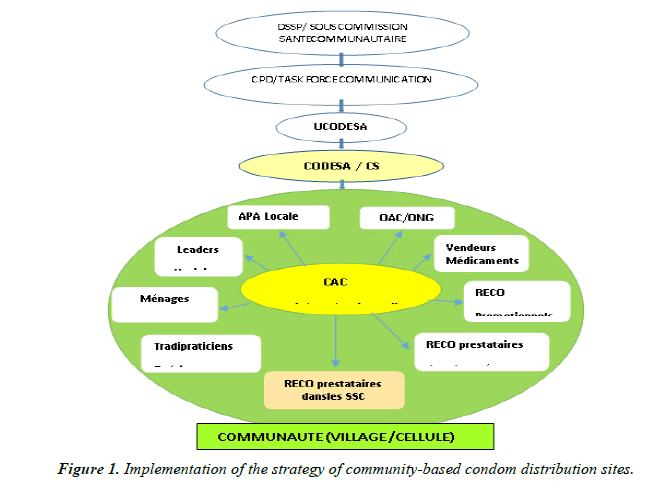
Based on our technique and method of intervention in the field, we are stakeholders in the structures and actors of the community system described below in this pendulum of community health in the DRC contributing to the response to the health pyramid starting from the direction of care of primary health care, the provincial health division, the health zone and the health area [15] Figure 1.
Thus the figure above demonstrates our approach to the
implementation of the strategy of community-based condom distribution sites targeted to key populations contributes to the response or response to the directives of community dynamics, lessons learned , adapt the interventions of the activities by health zone within the community animation cells (CAC) taking into account the national multi-sectoral strategic plan to fight against HIV AIDS, the national plan on community health and the support of UNFPA ,ASF/USAID in favour of our various targets below [16] Figure 2.
Young people and teenagers in the 15-25 age group
Making so much of this age trance, many publications and studies show that with regard to campaigns in favour of protected sexuality, it emerges from an assessment that has been drawn up "that there is at this there is no compelling example of a generalized epidemic being reversed as a result of preventive actions centred on condoms” (Green, 2003). Studies indicate that in the sub-Saharan region, younger generations continue to have sex around age 14, usually without a condom. About half of new infections in sub- Saharan Africa affect young people aged 15 to 24 (Global HIV Prevention Working Group, 2003) [17].
Our strategy within the community-based distribution sites of female and male condoms is ensured by health zone and community animation cell (CAC) in collaboration with youth associations such as RACOJ, Jeunesses Espoir and many other associations. community excise which received more than 284,585 condoms for the fight against sexually transmitted infections, HIV-AIDS for a group of at least 2095 young people and teenagers in the age group of 15 to 25 sensitized every 3 months during the he year with a view to contributing enormously to the protection of reproductive health and the AIDS virus because nowadays the consultation between the general practitioner and the teenager is a singular interview. The teenager, especially the boy is not often seen in consultation and this is increased by the current COVID-19 pandemic. Sexuality, contraception and STIs are discussed in consultation on the basis of different reasons. The approach to these subjects can come from the adolescent who has an explicit request or presents an acute problem or from the doctor during a prevention consultation. However, these themes are still addressed too rarely and unevenly. Many factors positively or negatively influence the general practitioner to address sexuality, contraception, and STIs [18].
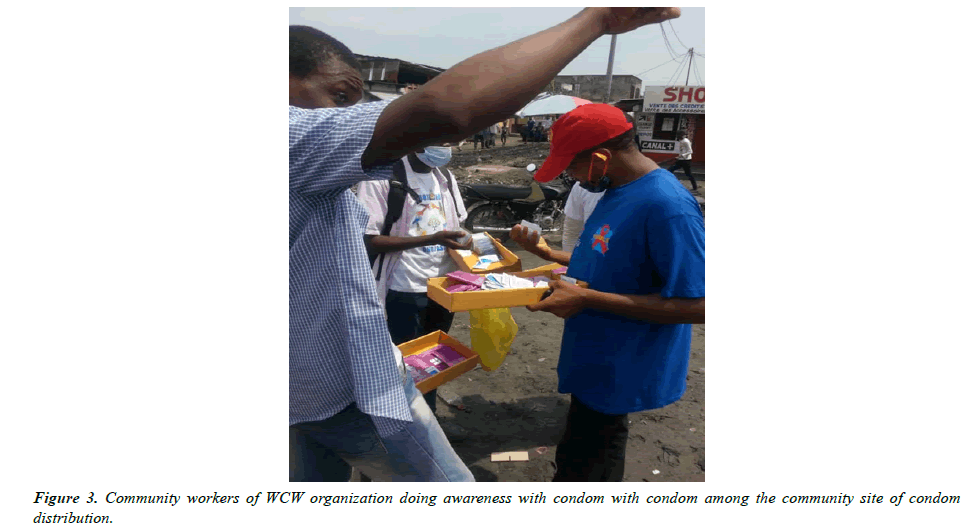
Starting from the advent of COVID19, several efforts in this direction have experienced a brake and sudden breaks; let's say boomerang effects on the psychological and social level with regressive repercussions on the medical, educational and economic levels as well as demographics. SARS-COV2 has contributed to the regressive return effects of actions already initiated in the fight against HIVSDA in this age group, stress, contempt, denial, sabotage, refusal to join programs associated with covid 19 Figure 3.
Adults in the 25-70 age groups among sex workers (SW)
Using projects like the EU-funded “HIV infection in female prostitutes” project has also linked reduced HIV infection with condom use. In addition, the project has shown that responsible correct use prevents the transmission of HIV [19], which is why we encourage our interventions in communitybased distribution sites of female and male condoms carried out in collaboration with local associations. such as CEDHUC-ONG, Forum sida and many other community excise associations within health zones and Community Animation Cells has contributed enormously to the reduction of sexually transmitted infections and HIVSDA in 450 PS sensitized as well as their sexual partners through 51,935 condoms . In addition, referring to the World Bank report published in 1997, we distinguish two categories of countries: those which were affected by an incipient epidemic, where cases of infection by the HIV virus remained rare, and those where concentrated or generalized epidemics prevailed. In the case of our country where these various community condom distribution sites operate, this report argued that for maximum cost-effectiveness, prevention programs should aim to prevent the greatest possible number of secondary infections per dollar spent, within three target audiences: adolescents, who still have life ahead of them, sex workers, likely to infect a large number of people like flight crew, drivers, road hauliers, who have frequent sexual relations and are vectors of infectious diseases. In countries with concentrated or generalized epidemics (e.g. in sub-Saharan Africa), the report again found it necessary to target audiences most likely to contract and spread the virus, but further called for going beyond these categorical approaches to take action with the general population. At that time, most countries in sub-Saharan Africa were slowly opening their eyes to the undeniable reality of the epidemic. National AIDS control programs have therefore begun to promote programs called ABC (Abstinence, Be Faithful or use Condoms), in other words advocating sexual abstinence, faithfulness or the use of condoms, to reduce the risk of transmission by sexual path, the Catholic Church opposing in most countries resistance to section "C" [20].
In these days these enormous contributions are experiencing disruptions, obstacles and mistrust, breakup of customers following the psychosis emitted by the consequences of the transmission of SARS-COV2, the boomerang effects of which have impacted certain customers and a return to square one at the start of the level. socio-economic, the total hassle in the social and psychological life of Sex Professionals (PS) because the quick hand-to-hand blows have known a mistrust for fear of being contaminated and becoming a case enumerate contact in the face of the screening strategy for the SARSCOV2 and the trusted customer has become a suspicious customer, hence the regression of savings and the purchasing power of PSs because the COVID-19 pandemic, like any other health crisis, brings to light existing inequalities and affects disproportionately already criminalized, marginalized and precarious populations who often do not benefit from social protection mechanisms as highlighted by the Global Network of Sex Work Projects (NSWP) and UNAIDS who wish to attract attention of all of us to the difficulties and concerns specific to sex workers according to [21] Charlotte Pezeril, Delphine Metten COVID -19 continues to spread around the world, many places face the risk of SARS infection -CoV-2 and barriers and challenges to maintaining the continuum of HIV care. The situation could be worse in places where health systems are weak. . Many authors of scientific publications and community actors in the fight against AIDS in Africa believe that the chronology of care for people living with HIV in Africa requires patient access to ARVs, but in the face of super infection, the need is to use male and female condoms [22] this is why our strategy of community-based distribution sites for female and male condoms carried by local associations such as WCW, COSAHO-ONG, Forum sida and support groups from Health facilities (FOSA) contribute enormously to play an important role in maintaining HIV-related services to ensure the reduction of cases of STI/HIV super infections, limitation of unwanted births and others in favour of more than 2,480 PLHIV/VVS/MSM sensitized through 242,285 condoms made available to them for correct and responsible use because studies show that A large French HIV PrEP cohort bringing together more than 3,000 MSM (men who have sex with men) from Paris and its region has confirmed the very large effectiveness of continuous or on-demand PrEP with TDF/FTC (Truvada), already demonstrated in the authorization studies: the two formulas showed in participants a 99 percent reduction in the risk of infection with HIV. Note that MSM taking PrEP continuously had significantly fewer side effects than those taking PrEP on demand. Some 75 percent of MSM were affected by sexually transmitted infections (STIs), including many cases of acute hepatitis C. In summary, the results of this cohort confirm the high efficacy and safety of TDF/FTC PrEP and highlight the importance of regular screening for STIs, including hepatitis C, as part of a PrEP. More information on HIV PrEP in Switzerland [23].
With the advent of SARS-COV2, several groups experienced a regression based on the boomerang effects of covid 19, quarantine, social distances, the psychological and economic effects of which are very remarkable by the drop in socioeconomic activities, frustrations, psychological shocks, emotional etc.,
There are reports that gender-based violence is on the rise during the COVID-19 pandemic. Are we likely to see an increase in HIV infections because of this? Absolutely! Sexual violence is a key driver of HIV infection, especially among adolescent girls and young women. Unfortunately, in Africa, 5,400 young women are infected with HIV every week! The infection rate for girls is four times higher than for boys of the same age. Women and girls are much more vulnerable to infection and it is all due to the tolerance of sexual violence, the culture of acceptance of harmful masculinity, the lack of comprehensive sex education in schools. This environment that makes a girl unsafe has been made worse by COVID-19 [24].
In several countries, the exceptional measures taken to fight the COVID-19 pandemic have had an enormous impact on the management of the other health needs of the populations. In the field of the fight against HIV, hepatitis and other STIs, services have been reduced and difficulties of access have multiplied. The program stresses the urgency of now ensuring the full resumption of screening and prevention activities and learning lessons from the fight against HIV [25].
OVC/ERF (HIV orphans and other vulnerable children in family breakdown)
In collaboration with so many other likembe centre association, association of children in family breakdowns and our strategy of community-based sites for the distribution of female and male condoms to contribute to the protection of more than 205 OVC and children in family breakdowns against crimes of sexual violence, abusive sexuality and clandestine abortions are sensitized through 23,735 condoms.
Particular attention is to encourage any Community Health Worker in SDCPs to make female condoms accessible to young girls for correct and responsible use, providing foresight given their vulnerability to sexual violence, STIs, unwanted pregnancies such as emphasizes Community Health Worker and HIV Peer Educator, Neema knows full well that teenage pregnancies and HIV infections are shattering the dreams of countless girls and young women in her community, country and across the continent. In Eastern and Southern Africa, HIV disproportionately affects adolescent girls and young women. About 4,900 adolescent girls and young women aged 15 to 24 are infected with the virus every week in sub-Saharan Africa. Most of these infections occurred in East Africa and Southern Africa without omitting Central Africa.
Wishing to help her peers overcome these obstacles, the health worker is a source of inspiration for young women in her community. It instils in them the will to educate themselves, the passion and the ability to act that they need to take charge of their destiny [26].
But with the boomerang effects of SARS-COV2, we have noted a regression in the level of monitoring and protection of this vulnerable group which has experienced denials, refusals to accept the situation of the effects of covid19 in the economies of associations of support as well as cases of ruptures of financing from where the galley.
People in uniforms
Numbers among which our interventions of communitybased distribution sites of female and male condoms to fight against sexually transmitted infections and HIV AIDS in favour of at least 795 People in uniform sensitized through 94,235 condoms, working in a displacement environment or progressive mobility away from their regular households in a sometimes aggressive professional command environment with effects on sexual habits and behaviour. The arrival of covid19 is a source of regular shortages in the supply of condoms in sites and causes psychosis and other psychological shocks in the management of infections and secondary infections of STIs/AIDS Figure 4.
INPSS learners
Among our associative collaborators for the implementation of the strategy of community-based sites for female and male condoms are a number of learners from the National Professional Institute of Health Science (INPSS) who, in collaboration with Tulene University, including a number of more than 50 young learners also have the duty to contribute to the fight against clandestine abortions, sexual health by the distribution of 8,225 condoms among young people and teenagers within the community because this program also aims to inform about the transmission of the virus HIV and AIDS, to develop the social promotion of condoms and to teach young people to practice negotiation, especially since in the face of poverty, misery and other social factors, girls have become very demanding of sexual intercourse. Within their circle, they have multiple partners and risky sexuality such as kamuké sukali transformed into Udjana, etc.
The realities within the socio-cultural diversity of communities there are exchange practices that play an important role in the negotiation of sexual relationships. Money and gifts are exchanged for a person's sexual favors and serve to strengthen ties. At school, the theme of condoms has sown continues to sow trouble, coming up against the uneasiness of the teachers responsible for tackling the question and the resistance of the parents. There are students who have even been withdrawn from school for this reason. Many programs focused on safer sex tend to underestimate the complexity of sexuality, its multiple meanings and the social relationships that underpin it. They postulate that individuals are autonomous and will respond rationally to information provided about the risks of HIV transmission. The reasons that push people to have sex are therefore multiple: to exercise power, to show love, to commit to someone or even to be "cool"... Why do we have sex, with whom, when and where? Etc.
But with SARS-COV2 and its boomerang effects contribute to the breakdown of actions in the face of denials, and other negative psychological attitudes that the stress of covid 19 provides within the community.
To do this, in order to ensure the feasibility of our interventions, we proceed to the technique of advocacy in favor of the right to sexual and reproductive health with technical and financial partners as well as with political-admiring authorities and leaders Figure 5, Table 1.
| No. | TARGET | Number | Qty dispensed | % | Observation |
|---|---|---|---|---|---|
| 1 | Youth 15-25 | 2.480 | 284.585 | 40.8 | Fight against STI/HIV clandestine abortion |
| 2 | PLHIV/VVS/MSM | 2.095 | 242.285 | 34.4 | Fight against STI/HIV superinfections, PMTCT-community, Sexual Violence |
| 3 | People in Uniform | 795 | 94.235 | 13 | Fight against STIs/HIV, unwanted pregnancies |
| 4 | Adults PS 25-70 | 450 | 51.935 | 7.4 | Fight against STIs/HIV |
| 5 | OVC/ERF | 205 | 23.735 | 3.3 | Fight against SV, STI/HIV |
| 6 | INPS learners | 50 | 8.225 | 0.8 | Fight against clandestine abortions, STI/HIV, unwanted pregnancies |
| Total | 6.075 | 705,000 | 100% |
Table 1. Quarterly distribution of condoms
Results
• 2,480 young people and teenagers in the age group of 15 to 25 benefited during the distribution carried out by site 284,585 condoms during the sensitization of their peers every 3 months during the year in order to contribute enormously to the protection of their health of reproduction and STI/AIDS, 40.8% need for condoms, sexually active population. An adoption of the correct and responsible use of male condoms at least per condom sexual intercourse every 3 months during the year.
• 450 PS are sensitized as well as their sexual partners for 51,935 condoms to contribute to the reduction of infections and super infections of sexually transmitted diseases and HIVSDA, that is to say 7.4% of expressed need for condoms.
• 2,095 PLHIV/VVS/MSM sensitized through 242,285 condoms to contribute to the reduction of cases of STI/ HIV super infections, limitation of births and births of unwanted children and preventive PMTCT, i.e. 34.4% condom need.
• More than 205 OVC and children in family breakdown against crimes of sexual violence, abusive sexuality and clandestine abortions are sensitized through 23,735 condoms for correct and non-abusive use, i.e. 3.3% expressed need for condoms.
• At least 795 People in uniform working in an environment of progressive displacement or mobility away from their households having aggressive effects on their sexual habits and behavior are sensitized on the correct and responsible use of at least 94,235 condoms at least one condom each sexual intercourse per trimester and per year, or 13% need for condoms.
• More than 50 young learners have the duty to contribute to fight against clandestine abortions by the distribution of 8.225 condoms among young people and teenager within the community is 0.8% of need in condoms.
• 5 target groups reached every 3 months
• Adoption of adaptive behavior in the face of the challenges of HIV for the survival of key populations in a post-conflict country. Implementation of resilience mechanisms.
Lessons learned
• The provision of male and female condoms has become one of the practical strategies for combating clandestine abortions, STIs/HIV, unwanted pregnancies, given the actions carried out within community distribution sites. , to do so, it is very important to create an environment conducive to supporting behavior change. This also depends on support from rapid and decisive political leadership. School closures and quarantine measures are powerful tools.
• But the lesson from HIV is that supporting safer behaviors means addressing the structures that limit or enable people's choices.
• Just as gender-based violence has hindered safer sexual behavior choices for women, so scarcity of clean water will limit hand washing. In the short term, pragmatic responses such as the massive and rapid distribution of soap, disinfectant and personal protective equipment against SARS-CoV-2 will be necessary (just as the distribution of female condoms was for the fight against HIV).
• The correct and responsible use of male and female condoms ensures the protection of key populations against super infections, sexual violence, STIs/HIV within community distribution sites and also serves as support for partners in the response to HIV. As Anita Hardon points out: “If we finance therapeutic initiatives in developing countries, we must limit ourselves to countries that have mobilized and demonstrated their political will to implement preventive actions. If they don't use condoms, why should we care for them? (Representative of a multilateral organization) [27].
• HIV actions associated with SARS-COV2 create psychological, economic and policy back-and-forth effects. Modern approaches to HIV prevention are however guided by a socio-ecological framework. Meaningful community involvement can shape social norms. Building social capital, trust and community cohesion catalyzes the impact of health messages and can be fostered by supporting local leaders. These dynamics will accelerate HIV control among gay men, sex workers, and other communities. The design of the COVID-19 response will need to include older people, those with comorbidities, and those already living at the margins. [28].
• However, despite our actions in the field within the community-based distribution sites for male and female condoms (SDCP), we take the liberty of pointing out a parallelism on the one hand by paraphrasing the organizing committee which thinks that the condom serves as a metaphor for the fight against HIV, just as the mask serves as a metaphor for SARS-COV2, some scientists like Gabriel Gérard think that obviously, the comparison of the two pathologies has its limits, already mentioned since their appearances, and temporality is a marker differentiation key. On the one hand, an epidemic that has been going on for nearly 40 years, highly deadly, on the other, a virus that has been circulating for barely 36 months. For HIV, we are talking about a disease with which we can live in the long term and that treatments can control it, when Covid-19 is curable, but unfortunately quickly fatal in the most serious cases. Still, paying attention to how certain groups are affected by Covid-19 is a prism that allows us to consider its long-term social and political repercussions [29].
• We must anticipate health inequalities. Pandemic transmission of HIV has accelerated among wellconnected mobile networks, but the burden has shifted to poorer people and countries, young women and marginalized groups. The global burden of COVID-19 is likely to be hit hardest by older people and vulnerable LMIC groups.
• We need to track the socio-economic status and gender of those affected and expand this effort to track economic impacts. UN member states have pledged that “no one will be left behind”. The global response to COVID-19 must honor this commitment. Social conditions make it difficult for vulnerable people to change their behavior.
• The encouragement to “abstain, be faithful and use condoms” could not prevent HIV where gender inequality and stigma were the norm. Likewise, following instructions for washing hands and ensuring physical distancing will be more difficult for people living in poverty. Public health initiatives must overcome barriers to reach the poor, even if they seem to be less affected by the virus now [30].
Recommendations
• In collusion with UN-AIDS we suggest the egalitarian observance of the 90 90 90 targets in the face of the challenges of HIV and SARS-COV2 [31].
• We recommend that governments, community organizations and international partners work together to maintain the continuum of HIV care during the COVID-19 pandemic, with a particular focus on ensuring timely access to routine HIV services. and to avoid their interruption of access to services, especially since two analyzes show that on the one hand an analysis published in the magazine Nature in 1998 shows the presence of HIV in a blood sample taken in 1959 from a man who died in the Republic of the Congo (Belgian Congo at the time). This is the first documented case of a human carried away by HIV / AIDS and on the other hand studies show that the virus would have been established in America by the intermediary of a single man, a Haitian, who would have travelled in the Congo [32].
• We must also ensure that gains in testing, treatment and care are preserved in the current COVID-19 context and expand services, especially for adolescents, young people, women and girls, key populations and other priority populations,
• Roll out vertical transmission prevention and pediatric ART coverage in a stigma-free environment, building on innovative service delivery models [33].
• Conduct a priori basic socio-cultural surveys or studies among African populations with a view to preventing attitudes and other socio-behavioural phenomena that are not acceptable to the introduction of single-dose HIV and SARS-COV2 vaccines because the Covid-19 has been marked by debates to convince those who have been called the " vaccino-hesitant ". Certain factors can influence the acceptance of vaccines. A younger age, female gender, ethnic origin (black and African-American), religious beliefs, certain political ideologies, low level of education or even a more modest socio-economic level are negatively associated with hesitation vaccination in some studies. [25, 26] A French study of PLHIV showed that almost 30% of participants were hesitant to receive the vaccine despite a perception of a higher risk of severe disease in the event of exposure to SARS-CoV-2 compared to the general population. General doubts about the vaccine, fear of potential serious side effects, and feeling already immune/protected against Covid-19 were factors associated with vaccine hesitancy [34].
• The NGO LESBATISSEURS through the communitybased distribution site strategy for male and female condoms (SDCP) together with UNAIDS therefore recommend; once again, we call on governments to provide services. Communities need to be on the lookout. Community leaders must speak out. Where there is a threat, we must have shelter. We need to increase sexual and reproductive health services, which have been cut as governments juggle their resources. We say GBV responders, counsellors, sexual and reproductive health workers must be considered essential workers in the COVID-19 response, and their services must be maintained (Winnie Byanyima: Africa new).
Conclusion
In closing, together with Kimberly Marsh of UNAIDS, we ask ourselves the question: what about HIV prevention? does ensuring the availability of condoms have an impact in the post RSAS-COV2 period? The answer is yes because it is worth noting that when looking more closely at prevention services, our models reveal that the availability of condoms influences outcomes. It is important to say that treatment is paramount, but aspects such as access to condoms play a paramount role. We found a relative increase in HIV incidence of 20-30% over one year if condoms are missing for six months. They must therefore really be among our priorities.
The models focused on different possible disruptions to HIV services in sub-Saharan Africa due to the COVID-19 pandemic. These disruptions can impact HIV incidence (the number of new HIV infections) and the number of additional AIDS-related deaths than we would have seen if the COVID-19 pandemic had not happened. Not declared [35].
On the social level, this strategy of community distribution sites for male and female condoms (SDCP) is a response to adopting a positive way of life, a social behaviour of survival in the face of the challenge of HIV among African and Caribbean communities. and black people, children and adolescents, men who have sex with men (MSM), HIV care and treatment, prevention interventions and programmes, living with HIV and women; as the COVID-19 pandemic continues to impact global health priorities and HIV service delivery [36].
Several groups have experienced regressive pressures: quarantine, social distances, contact cases with the long list whose psychological and economic effects are very remarkable by the fall in socio-economic and political activities, frustrations, psychological and emotional shocks, work strategy by Zoom characterizing the lack of socialization in several work groups and areas of life, thus causing disarticulation and dysfunction and a drop in production Thus in several communities we note the designation of “irresponsible” individuals or behaviour is a classic
in the collective construction of prevention discourse. This mechanism makes it possible to draw a boundary between "good" and "bad" practices in the face of the risk of infection either with HIV or with SARS-COV2. In doing so, beyond the health issue, it asserts ways of doing things in society in a context of uncertainty. Faced with the risk of HIV transmission, discourse on the prevention and promotion of condoms has largely relied on this process. With a major pitfall, regularly pointed out by the social sciences: the focus on individual practices obscures the social conditions of prevention. However, experience shows that practices considered "unsuitable" from the point of view of public health are often perfectly explicable if the context in which they occur is taken into account. Moreover, given their unprecedented scale, their seriousness and the shock that they have both caused, AIDS and Covid-19 confront us with unprecedented health, social, economic and political challenges.
Not only do AIDS and Covid-19 respond to the three characteristics of Global Health issues according to Jeffrey Koplan (transcending national borders, calling for collective action and imposing a transversal approach), but they are, as we have seen, totally emblematic of these issues [36-39].
References
- Jiang H, Zhou Y, Tang W. Maintaining HIV care during the COVID-19 pandemic. The lancet HIV. 2020;7(5):e308-9.
- Joint United Nations Programme on HIV/AIDS. Global AIDS strategy 2021− 2026.
- Theme of the conference, scientific program committee.
- Internal document, NGO LS Batisseurs, presentation of the organization, 2023.
- JMS 2021 activity report, NGO LES Batisseurs/UNFPA, 2022.
- Mary Slavicek. HIV screening and prevention: Covid-19 has ruined the progress made in recent years. 2021
- Strategic plan of the Advocacy HIV / TUB DRC consortium 2020-2022.
- National strategic plan for the AIDS response 2020-2023 (PNMLS).
- 9Public Health Agency of Canada: “Estimates-hiv-incidence-prevalence-canada-meeting-90-90-90-targets-2020”, 2022.
- CATIE Canada's source for HIV and hepatitis C information: "Condoms and other physical barriers", 2021.
- “Covid-19: some lessons from the fight against HIV/AIDS”, 2020.
- "Self-confidence: how to overcome the boomerang effect", 2019.
- "Because of the coronavirus, a "disastrous" shortage of condoms is looming", the huffpost newsletters, 2020.
- Stephenson R, Chavanduka TM, Rosso MT, et al. Sex in the time of COVID-19: results of an online survey of gay, bisexual and other men who have sex with men’s experience of sex and HIV prevention during the US COVID-19 epidemic. AIDS Behav. 2021;25:40-8.
- National Community Health Strategic Plan 2019-2022.
- National Multisectoral Strategic Plan for the Fight against HIV-AIDS. 2019-2022.
- Hardon A. Combating the HIV/AIDS Epidemic in Sub-Saharan Africa: Putting Policies to the Test of Practice.
- How are issues relating to sexuality, STIs and contraception addressed in male adolescents in general practice consultations? 2022.
- The European Commission, CORDIS, the result of EU scientific research: "Commission provides 'strong scientific evidence' of link between condom use and HIV prevention", 2003.
- Hardon A. Confronting the HIV/AIDS epidemic in sub?Saharan Africa: policy versus practice. Int J Soc Sci. 2005;57(186):601-8.
- Charlotte Pezeril, Delphine Metten. Observatory of AIDS and sexualities: “Covid19 and HIV”, 2020
- Eboko F. Treating Aids in Africa. Biomedical Research and Humanitarian Work. Ethnol Fr. 2011;41(3):497-507.
- Hargreaves J, Davey C, Auerbach J, et al. Three lessons for the COVID-19 response from pandemic HIV. Lancet HIV. 2020;7(5):e309-11.
- Byanyima W, Musau Z. Addressing HIV in the time of COVID-19, 2020.
- Charlotte Pezeril, Delphine Metten. Observatory of AIDS and sexualities: “Covid19 and HIV”, 2020.
- Vulugu N. “HIV peer educator inspiring girls in her community”, 2022.
- Hardon A. The fight against the HIV /AIDS epidemic in sub-Saharan Africa: Policies put to the test of practice, Érès. Int J Soc Sci. 2005: 661-669.
- Hogg RS. Understanding the HIV care continuum. Lancet HIV. 2018;5(6):e269-70.
- One world, one health, one species Pandemic and cosmopolitics.
- Joint United Nations Program on HIV/AIDS (UNAIDS) Fact sheet: World AIDS Day 2019-global HIV statistics. 2019. ‘
- Labelle A. HIV/AIDS through time: our chronology, 2022.
- Tchiombiano S. Aids and Covid-19, two emblematic diseases of global health. Med Trop Sante Int. 2021;1(2):mtsimagazine-n1.
- Canada's source for HIV and hepatitis C information a history of HIV and AIDS.
- Tshikung ON., Calmy A. “HIV/AIDS. HIV and Covid-19: two interacting viral pandemics”, 2022;18:764-65.
- Braun DL. HIV is a risk factor for a severe form of COVID-19, UN-AIDS, Global AIDS Strategy, 2021-2026, 2021.
- Marsh K. Modeling extreme situations: COVID-19 and AIDS-related mortality, 2020.
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497-506.
- Tang W, Wu D. Opportunities and challenges for HIV self-testing in China. The lancet HIV. 2018;5(11):e611-2.
- Eboko F. Treating Aids in Africa. Biomedical Research and Humanitarian Work. Ethnol Fr. 2011;41(3):497-507.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref