Case Report - Ophthalmology Case Reports (2023) Volume 7, Issue 1
Spontaneous closure of traumatic macular hole: The fastest yet.
Oscar Eaton*, Francesc March de Ribot
Department of Ophthalmology, Dunedin Hospital, Dunedin, New Zealand
- Corresponding Author:
-
Dr. Oscar Eaton
Department of Ophthalmology,
Dunedin Hospital,
Dunedin,
New Zealand,
E-mail: o.eaton@me.com
Received: 05-August-2022, Manuscript No. OER-22-71303; Editor assigned: 10-August-2022, PreQC No. OER-22-71303 (PQ); Reviewed: 24-August-2022, QC No. OER-22-71303; Revised: 31-January-2023, Manuscript No. OER-22-71303 (R); Published: 28-February-2023, DOI: 10.35841/oer-7.1.154
Citation: Eaton O, de Ribot FM. Spontaneous closure of traumatic macular hole: The fastest yet. Ophthalmol Case Rep. 2023;7(1):154
Abstract
Spontaneous closure of traumatic macula holes has widely been reported between 2-54 weeks. However, closure in under 2 weeks is rare. A man in his 20’s presented to our eye department following blunt trauma to the right eye from a paint ball gun. Examination revealed a full thickness macula hole with overlying operculum. Spontaneous closure was found 4 days after the injury.
Keywords
Macular hole, Spontaneous closure, Traumatic, Operculum.
Introduction
The vitreoretinal interface of the human eye is a complex anatomical structure where the vitreous gel attaches to the inner limiting membrane of the retina via collagen fibrils and adhesive molecules consist of fibronectin and laminin [1]. Over time, the vitreous gel undergoes liquefaction accompanied by progressive weakening of the adhesion at the vitreoretinal interface. These processes lead to a detachment of the vitreous from the retina, known as Posterior Vitreous Detachment (PVD), the early signs of which are evident from 40 years of age onward [2].
Persistent Vitreo Macular Adhesion (VMA) develops when only a partial PVD take place and part of the posterior hyaloid remains attached to the macular area. This interminable adhesion can lead to traction at the vitreoretinal interface, often referred to as Vitreomacular Traction (VMT), which in turn can lead to symptoms including metamorphopsia, decreased Visual Acuity (VA), and central visual field defects. Based on the literature, there is a familiar association between VMT (and symptomatic VMA) and diabetic retinopathy and similarly with exudative age related macular degeneration [3-6].
Vision in patients with untreated VMT may decline over time, while spontaneous vitreomacular separation occurs infrequently. In a study of patients with VMT who underwent vitrectomy, significant improvement in VA was observed in eyes with shorter duration of symptoms. These data suggest that earlier treatment of VMT may help to perform a better visual outcome [7].
Progression of VMT can lead to Full Thickness Macular Hole (FTMH) formation, which if left untreated can accompany to central legal blindness. Based on data from observational and randomized trials, conducted previous surgery became the standard of care for treatment of FTMHs; the spontaneous closure of FTMHs is a rare occurrence. Rather, the majority (>70%) of small Macular Holes (MHs) tend to expand in diameter, and VA decreases. Furthermore, with longer duration of FTMHs, there is a greater likelihood of irreversible retinal damage and associated lack of functional improvement following surgery [8].
Until recently, the only treatment for VMT, MH, and other diseases related to abnormalities of the vitreoretinal interface was vitrectomy. Vitrectomy has costs and risks associated with it, and the risks can limit safety and efficacy. As a result, most eyes with VMT have been observed, rather than treated, until significant loss of vision has already occurred. A minimally invasive release of vitreous traction could potentially be paradigm shifting in the management of these patients.
Ocriplasmin (generic name for microplasmin) is a truncated form of the serine protease plasmin that has retained its enzymatic properties. Recently approved for use in the United States and Europe, ocriplasmin is a vigorous collagenase activator with proteolytic activity against a range of components of the vitreoretinal interface, including fibronectin and laminin. In vitro, ocriplasmin has the greater activity against fibrinogen, followed by fibronectin, gelatin, collagen type IV, and laminin. The proteolytic activity of ocriplasmin may lead to disruption of the vitreoretinal interface while preserving the morphology of the retina and the ultrastructure of the inner limiting membrane. Previous preclinical and clinical studies have highlighted the beneficial effects of ocriplasmin in facilitating PVD. Experiments carried out in vivo and ex vivo demonstrated that intravitreal injection of ocriplasmin shows pharmacologic vitreolysis with detachment of the vitreous from the retinal surface. Phase 2 studies demonstrated that ocriplasmin was well tolerated and produced nonsurgical resolution of VMA and closure of FTMHs [9,10].
Results of two phase 3 clinical trials showed a statistically significant difference in favor of a single intravitreal injection of ocriplasmin 125 μg versus placebo injection for achieving the primary efficacy end point, VMA resolution at day 28, as well as the key secondary efficacy end point, total PVD at day 28.24 compared with placebo injection, eyes treated with ocriplasmin were more likely to have nonsurgical closure of FTMHs at day 28 (P<0.001), nonsurgical three line or greater improvement in Best Corrected Visual Acuity (BCVA) at 6 months (P=0.02), and a reduced need for vitrectomy at 6 months after ocriplasmin treatment (P=0.02) (secondary end points) [11].
Case Presentation
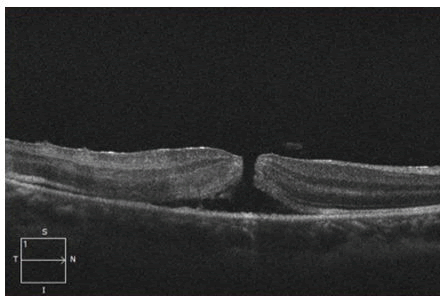
A man in his 20’s presented to our eye department following blunt trauma to the right eye from a paint ball gun earlier that day. The Visual Acuity (VA) of the affected eye was 1/60, Intraocular Pressure (IOP) was 14 mmHg, and the anterior segment was normal. Posterior segment examination revealed a full thickness elliptical macular hole with perimacula oedema and scattered intraretinal haemorrhage and oedema throughout the periphery (Figure 1). On Ocular Coherence Tomography (OCT) the narrowest internal diameter of the defect measured 148 μm (Figure 2) [12].
Results and Discussion
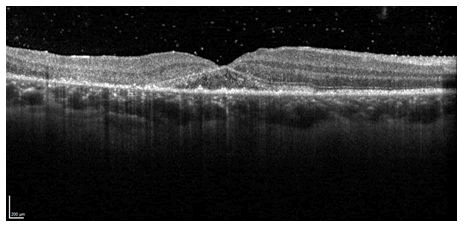
There was presence of vitreomacular adhesion with overlying operculum, localised detachment of the neurosensory retina and an absence of cystic oedema at the hole margin. On review 4 days after injury spontaneous closure was observed (Figure 3). The examination revealed complete posterior vitreous detachment with apposition of the macula hole, increased retinal thickness and atrophic changes. The patient was reviewed again at 3 months with a VA of 1/60. There was restoration of the foveal pit and progression of the inferiortemporal macula atrophy.
Conclusion
Spontaneous closure of traumatic macular holes has been reported many times before, with a varied time course of between 2 and 54 weeks. Closure under 2 weeks is rare, with one of the earliest reports being 10 days. Classification of traumatic macula hole based on OCT findings can aid in the prediction of hole closure. In this case, the absence of posterior vitreous detachment at the time of injury and the absence of cystic oedema at the hole margin was associated with hole closure. Spontaneous closure is usually associated with improvement in visual acuity, although the severity of initial trauma and extent of neurosensory retinal detachment can limit the visual outcome, as in this case.
Patient Consent
Oral consent has been obtained to allow publication of the case and inclusion of imaging.
Acknowledgment
None.
References
- Yamada H, Sakai A, Yamada E, et al. Spontaneous closure of traumatic macular hole. Amer J Ophthalmol. 2002;134(3):340-7.
[Crossref] [Google Scholar] [PubMed]
- Miller JB, Yonekawa Y, Eliott D, et al. Long term follow up and outcomes in traumatic macular holes. Amer J Ophthalmol. 2015;160(6):1255-8.
[Crossref] [Google Scholar] [PubMed]
- Misra DK, Barman M, Deori N, et al. Hyperacute spontaneous closure of a traumatic macular hole in a colobomatous eye. Amer J Ophthalmol Case Rep. 2019;15:100504.
[Crossref] [Google Scholar] [PubMed]
- Huang J, Liu X, Wu Z, et al. Classification of full thickness traumatic macular holes by optical coherence tomography. Retina. 2009;29(3):340.
[Crossref] [Google Scholar] [PubMed]
- Zhou Q, Feng H, Lv H, et al. Vitrectomy vs. spontaneous closure for traumatic macular hole: A systematic review and meta analysis. Fron Med. 2021;8:2622.
[Crossref] [Google Scholar] [PubMed]
- Petropoulos IK, Matter MA, Desmangles PM. Spontaneous closure of macular hole: One year follow up with spectral domain optical coherence tomography. Klinische Monatsblatter Fur Augenheilkunde. 2009;226(4):363-4.
[Crossref] [Google Scholar] [PubMed]
- Aalok L, Azad R, Sharma YR, et al. Microperimetry and optical coherence tomography in a case of traumatic macular hole and associated macular detachment with spontaneous resolution. Indian J Ophthalmol. 2012;60(1):66.
[Crossref] [Google Scholar] [PubMed]
- Newman DK, Flanagan DW. Spontaneous closure of a macular hole secondary to an accidental laser injury. British J Ophthalmol. 2000;84(9):1075.
- Gao L, Dong F, Chan WM. Traumatic macular hole secondary to Nd: YAG laser. Eye. 2007;21:571-3.
[Crossref] [Google Scholar] [PubMed]
- Fernández MG, Navarro JC. Spontaneous closure and quick reopening of a full thickness idiopathic macular hole. Vision Pan America. 2012;11:60.
- Gupta MP, Ferrone PJ. Pediatric macular hole. A Quick Guide to Pediatric Retina. 2021:277-281.
- Goel N, Prakash A, Gupta AK. Repeat fluid gas exchange for failed primary macular hole surgery. Indian J Ophthalmol. 2014;62(11):1104-5.
[Crossref] [Google Scholar] [PubMed]