Case Report - Journal of Gastroenterology and Digestive Diseases (2016) Volume 1, Issue 1
Splenic Artery Pseudoaneurysm in the Setting of Acute Pancreatitis and Valproate in a 12 Year Old Male
Grant Morris*Department of Pediatrics, Geisinger Medical Center, Academy Avenue, Danville, USA
- *Corresponding Author:
- Morris G
Department of Pediatrics, Geisinger Medical Center, 100 N. Academy Avenue, Danville, PA 17822, USA,
Tel: 570-271-5606
Fax: 570-214-0133
E-mail: gamorris@geisinger.edu
Received date: April 24, 2016; Accepted date: June 20, 2016; Published date: June 23, 2016
Abstract
Splenic artery pseudoaneurysm, a rare complication of pancreatitis, carries a potentially high mortality rate and must be considered in recurrent pancreatitis. Advances in diagnostic and therapeutic techniques, especially endovascular embolization, have decreased morbidity and mortality. We present a pediatric patient with splenic artery pseudoaneurysm following recurrent pancreatitis managed with endovascular embolization.
Keywords
Abdominal pain; Pancreatitis; Coil embolization; Endovascular; angiography; Valproate.
Introduction
This case would be useful in a class to discuss the importance of recurrent pancreatitis in pediatrics and outlines the need for further work up for this condition. Additionally, this case illustrates the use of endovascular techniques to repair vascular complications of pancreatitis.
Case Description
The primary subject matter of this case concerns pediatric gastroenterology. Secondary issues examined include vascular complications of pancreatitis and recurrent pancreatitis. The case has a difficulty level appropriate for second year graduate students. The case is designed to be taught in one to two class hours and is expected to require one to two hours of outside preparation by students.
Case Synopsis
The incidence of pancreatitis in children has been increasing over the past two decades [1]. The diagnosis of acute pancreatitis requires two of the following three criteria: abdominal pain that suggests, or is compatible with acute pancreatitis, serum lipase or amylase that is at least three times greater than the upper limit of normal, and imaging findings characteristic of, or compatible with acute pancreatitis [2]. Acute pancreatitis in children is typically caused by trauma, systemic illness, biliary disease, or medications, such as valproate or azathioprine. Medications, in general, have been estimated to account for 0.3 to less than 2 percent of all cases of acute pancreatitis with higher incidences in pediatric patients, although this etiology is believed to be underreported [3]. Fortunately, most cases are self-limiting and have a benign course. Additionally, in recurrent pancreatitis it is important to consider anatomic, environmental, metabolic, autoimmune, and genetic factors [4]. Splenic artery pseudoaneurysm (SAP) is a rare complication of pancreatitis, and is more often reported in children following blunt abdominal trauma [5]. To our knowledge, there have been six reports of pediatric SAP unrelated to trauma [6-11], one of which was related to medication9. We present a case of a pediatric patient with SAP following acute pancreatitis in a patient taking valproate.
Case Report
A 12-year-old African American male with a complex past medical history, including seizure disorder, presented with two days of abdominal pain and irritability following a week of cough, rhinorrhea, and fatigue. He had decreased appetite. No emesis, diarrhea, fever, trauma, rash, or recent seizure. He had a history of constipation treated successfully with polyethylene glycol. Labs revealed a lipase of 206 U/L (reference range 3-32 U/L), amylase 217 U/L (reference range 30-100 U/L), elevated valproate level, and platelet count of 45,000 (reference range 140-400 K/uL). Additional labs included normal liver and kidney panels, white blood cell count, and hemoglobin. Parvovirus B19, Epstein-Barr virus, and cytomegalovirus titers were negative. Hereditary pancreatitis panel (CFTR, PRSS1, SPINK1) was negative.
Two months prior he had symptomatic acute pancreatitis presenting with intermittent abdominal pain which was worse after eating. Amylase was 219 U/L and lipase was 257 U/L. At that time, abdominal ultrasound was normal with a poorly visualized pancreas. Outpatient management included low fat diet. Lipase normalized within 10 days.
Past medical history included: hyperthermia-induced cerebral infarct and hemorrhage at age 8 months, global developmental delay, cerebral palsy, complex partial seizures, and constipation. Medications were valproate, rufinamide, clonazepam, clonidine, omeprazole, folic acid, and polyethylene glycol. Family history unknown, as patient was adopted.
Physical exam at admission revealed a developmentally delayed non-verbal male in no distress. Vital signs and general physical exam were normal. Abdomen was soft, non-tender, nondistended with no organomegaly. Normal bowel sounds.
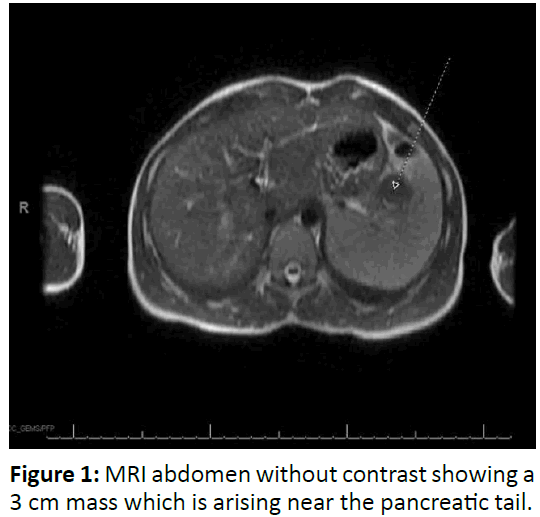
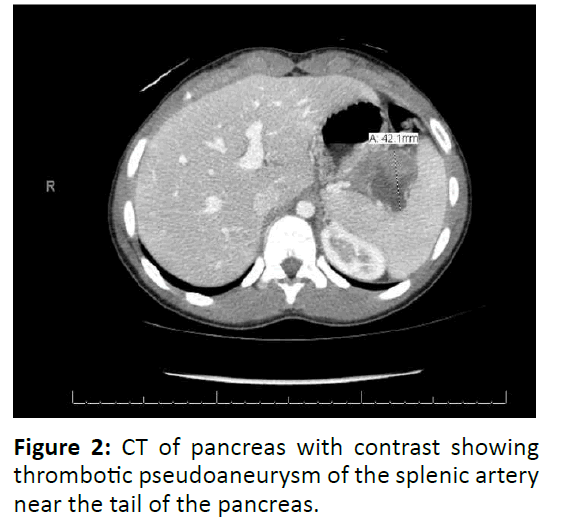
On admission, a clear liquid diet, IV fluids and pantoprazole were started. Pain was controlled with ketorolac. Valproate was discontinued. Due to his second episode of pancreatitis, non-contrast abdominal magnetic resonance imaging (MRI) and magnetic resonance cholangiopancreatography (MRCP) were obtained, revealing 3.1 centimeter heterogeneous mass with evidence of blood products arising from pancreatic tail (Figure 1). Subsequent pancreatic computed axial tomography (CT) scan with IV contrast showed nearly completely thrombosed pseudoaneurysm of the splenic artery at splenic hilum with 4.2 centimeter maximum axial dimension as well as edematous pancreatic tail (Figure 2). He underwent successful coil and Gel- Foam embolization of actively bleeding branch of the splenic artery. There were no prior signs of bleeding. Lipase normalized two days after coil embolization. Three weeks later, follow up abdominal CT angiogram showed resolution of splenic hilar artery hematoma and pseudoaneurysm without complicating infarct. He has not had any further episodes of pancreatitis.
Case Overview
The incidence of acute pancreatitis is a rising entity among children [12]. The Food and Drug Administration reports pancreatitis as a black box warning for valproate. Most cases of valproate associated pancreatitis present within the first year of therapy; however it can develop at any time [13]. This patient was diagnosed with two episodes of acute pancreatitis based on the clinical definition from the INSPPIRE group2 after two years of valproate therapy. Additionally, he met the criteria for acute recurrent pancreatitis given that he had a documented normal lipase with complete resolution of abdominal pain before the subsequent episode of acute pancreatitis [2]. He also had a SAP, which is very rare in the pediatric population. SAPs can be complications of pancreatitis and are believed to form when the splenic artery wall integrity is compromised following exposure to pancreatic enzymes leading to vascular erosion. This leads to a weak vessel wall and formation of a pseudoaneurysm (PA) as blood leaks out and is contained by surrounding fibrotic tissues. Additionally, PA’s are commonly associated with pseudocysts [6,7,14].
This patient was on valproate which can be considered high risk therapy given the FDA black box warning. However, valproate was deemed the best medication to control his seizures, which is why it was continued after the first episode of acute pancreatitis. For this patient, valproate was a set up for his pancreatitis which ultimately led to his SAP. The patient’s imaging studies did not reveal any congenital or structural abnormalities making this etiology unlikely. Additionally, he had an unremarkable infectious and hereditary work up which further supports valproate as a cause of the pancreatitis leading to the SAP
PA’s most commonly involve the splenic artery due to it’s course along the pancreas [6,8,11]. However, any vasculature along the pancreas can be affected, as illustrated by cases involving the gastroduodenal artery [7] and the superior mesenteric artery6. PA’s take time to develop, usually don’t occur immediately after an episode of pancreatitis, and can develop between weeks to years after an episode of pancreatitis [7,13].
The clinical presentation of a PA from most to least common includes abdominal pain, hematochezia/melena, hemosuccus pancreaticus, and hematemesis [13]. This child presented with abdominal pain two months after an acute episode of pancreatitis. A similar presentation of diffuse abdominal pain was reported in a 6-year-old with chemotherapy (L-asparaginase) induced acute pancreatitis complicated by a SAP [9].
Accurate and timely diagnosis of SAP is vital because of the potentially lethal hemorrhage that could occur if the PA spontaneously ruptures [6,8,13]. Catheter angiography is considered the gold standard of diagnosis and allows visualization of smaller pseudoaneurysms that can be missed with CT and given the significant morbidity of even small pseudoaneurysms, direct angiography might still need to be considered if suspicion is high as it allows the added benefit of embolization at time of diagnosis [7,8]. However, advancements in technology allow multidetector computed tomography (MDCT) to be a sensitive modality that allows less invasive but comparable assessment6. Additionally, MDCT with angiography can be useful for pre-surgical planning [6]. Ultrasonography is a less reliable diagnostic modality as it is operator dependent and may be limited due to bowel gas or obesity8. If these lesions are large, duplex Doppler ultrasound may be able to identify turbulent arterial flow within an anechoic mass [11,15].
Treatment should be initiated immediately given this potential for spontaneous rupture and high mortality [8,13]. With improved technology and endovascular techniques, surgery is no longer firstline therapy. Transcatheter embolization has become the more common therapeutic procedure, offering reduced morbidity and mortality as compared to direct surgical intervention8. Most commonly, only the feeding vessel is embolized to achieve thrombosis of the PA [13,14]. Potential complications from this technique include splenic infarction, migration of coil, intestinal necrosis and vascular dissection [13,14]. Close follow up is necessary to monitor for re-bleeding in which splenectomy would be the definitive therapy [14].
It is important that patients with a second episode of pancreatitis be considered for additional work up for underlying pathology, including additional laboratory studies and imaging. This case further supports transcatheter embolization as a minimally invasive and safe treatment in hemodynamically stable children with SAP. It also demonstrates the importance of maintaining suspicion for a PA in children that present with abdominal pain with a history of pancreatitis and the utility of imaging these children.
Discussion Questions
–– What are the clinical criteria necessary to diagnose acute pancreatitis? What are the criteria for acute recurrent pancreatitis? Answer: The diagnosis of acute pancreatitis requires two of the following three criteria: abdominal pain that suggests, or is compatible with acute pancreatitis, serum lipase or amylase that is at least three times greater than the upper limit of normal, and imaging findings characteristic of, or compatible with acute pancreatitis. Acute recurrent pancreatitis requires at least two distinct episodes of acute pancreatitis along with one of the following: complete resolution of pain (at least a one month pain-free interval between the diagnoses of acute pancreatitis) or complete normalization of serum amylase or lipase before the subsequent episode of acute pancreatitis is diagnosed, along with complete resolution of pain, irrespective of the time interval between episodes of acute pancreatitis.
–– What are broad categories for potential causes of recurrent pancreatitis in the pediatric population? Answer: Anatomic, environmental, metabolic, autoimmune, and genetic causes (i.e. CFTR, PRSS1, SPINK1).
–– What is the most common artery involved in pseudoaneurysms associated with pancreatitis usually involved and why? Answer: splenic artery due to its adjacent position and course to the pancreas.
–– What are the most common presenting symptoms of a patient with a splenic artery pseudoaneurysm? Answer: abdominal pain, hematochezia/melena, hemosuccus pancreaticus, and hematemesis.
–– What is the gold standard for diagnosis of SAP and why? Catheter angiography is considered the gold standard of diagnosis which allows visualization of smaller pseudoaneurysms that can be missed with CT and given the significant morbidity of even small pseudoaneurysms. This also has the benefit of being therapeutic.
–– Are there any potential strategies to prevent pseudoaneurysms in the setting of pancreatitis? Answer: There are not any known documented ways to prevent an arterial pseudoaneurysm in the setting of pancreatitis. The best approach would be to effectively manage the pancreatitis and/or prevent further episodes of pancreatitis. This would best be done by doing an appropriate work up to determine the etiology of pancreatitis. For this patient specifically, perhaps his SAP could have been prevented by discontinuing the valproate after the first episode of pancreatitis. However, valproate was determined to be the best medication to control his seizures.
References
- Bai HX, Lowe ME, Husain SZ (2011) What have we learned about acute pancreatitis in children? J Pediatr Gastroenterol Nutr.52:262-70.
- Morinville VD, Husain SZ, Bai H, Barth B, Alhosh R, et al. (2012) Definitions of pediatric pancreatitis and survey of present clinical practices. J Pediatr Gastroenterol Nutr. 55:261-265.
- Husain SZ, Morinville V, Pohl J, Abu-El-Haija M, Bellin MD,et al. (2016) Toxic-Metabolic risk factors in pediatric pancreatitis: recommendations for diagnosis, management and future research. J Pediatr Gastroenterol Nutr. 62:609-17.
- Werlin S, Konikoff FM, Halpern Z, Barkay O, Yerushalmi B, et al. (2015) Genetic and elctrophysiological characteristics of recurrent acute pancreatitis. J Pediatr Gastroenterol Nutr. 60:675-679.
- Oguz B, Cil B, Ekinci S, Karnak I, Akata C, et al. (2005) Posttraumatic splenic pseudoaneurysm and arteriovenous fistula: diagnosis by computed tomography angiography and treatment by transcatheter embolization. J Pediatr Surg. 40:e43-46.
- Ahmed HK, Hagspiel KD, McGahren III ED, Angle JF, Leung DA,et al. (2004) Pancreatic pseudoaneurysm in a child with hereditary pancreatitis: diagnosis with multidetector CT angiograpy. Pediatr Radiol. 34:656-659.
- Allen CJ, Curbelo M, Samuels SL, Perez EA, Chacon A,et al. (2015) Endovascular coil embolization of a pancreatic pseudoaneurysm in a child with pancreatitis. Pediatr Surg Int. 31:1195-1198.
- Fuchs Y, Candela N, Sung C, Weinstein T, Levine J (2010) Splenic pseudoaneurysm in a child with hereditary pancreatitis. J Pediatr Gastroenterol Nutr. 50:686-687.
- Larsen CC, Laursen CB, Dalby K, Graumann O (2014) Splenic artery pseudoaneurysm due to acute pancreatitis in a 6-year-old boy with acute lymphoblastic leukaemia treated with L-aspariginase. BMJ Case Rep. doi:10.1136/bcr-2013-202298.
- Puri A, Acharya H, Tyagi S, Curian S, Chadha R,et al. (2012) Pseudoaneurysm of the radial branch of the splenic artery with pancreatic pseudocyst in a child with recurrent acute pancreatitis: treatment with endovascular stent graft and cystogastrostomy. J Pediatr Surg. 47: 1012-1015.
- Srinivas M, Kataria R, Bhatnagar V, Tandon T, Iyer KV, et al. (1998) Intra-pancreatic splenic artery pseudoaneurysm. A rare complication of chronic calcific pancreatitis. Pediatr Surg Int. 13:171-174.
- Nydegger A, Heine RG, Ranuh R, Gegati-Levy R, Crameri J, et al. (2007)Changingincidence of acutepancreatitis: 10-year experience at the Royal Children's Hospital, Melbourne. J Gastroenterol Hepatol. 22:1313-1316.
- Verde F, Fishman EK, Johnson PT (2015) Arterial pseudoaneurysms complicating pancreatitis: literature review. J Comput Assist Tomogr. 39:7-12.
- Tessier DJ, Stone WM,Fowl RJ,Abbas MA,Andrews JC, et al. (2003)Clinicalfeatures and management of splenic artery pseudoaneurysm: Case series and cumulative review of literature. JVasc Surg. 38:969-974.
- Kirby JM, Vora P, Midia M, Rawlinson J (2008) Vascular complications of pancreatitis: imaging and intervention. Cardiovasc Intervent Radiol. 31:957-970.