Research Article - Journal of Physical Therapy and Sports Medicine (2022) Volume 6, Issue 6
Some aspects of rehabilitation of post-covid patients with ischemic stroke.
Gulnora Sattarovna Rakhimbaeva, Shokhida Rustamovna Gazieva, Dilnoza Turdikulovna Bobamuratova, Dilshoda Turdikulovna Akramova*, Ulugbek Doniyor Ugli ShodiyevDepartment of Neurology, Tashkent Medical Academy, Republic of Uzbekistan
- *Corresponding Author:
- Dilshoda Turdikulovna Akramova
Department of Neurology
Tashkent Medical Academy
Republic of Uzbekistan
Tel: +99894118589
E-mail: rustamovna89@mail.ru
Received: 25-Oct-2022, Manuscript No. AAJPTSM-22-78176; Editor assigned: 31-Oct-2022, PreQC No. AAJPTSM-22-78176;(PQ); Reviewed: 17-Nov-2022, QC No AAJPTSM-22-78176; Published: 24-Nov-2022, DOI:10.35841/aajptsm-6.6.126
Citation: Akramova D.T. Some aspects of rehabilitation of post-covid patients with ischemic stroke. J Phys Ther Sports Med. 2022;6(6):126
Abstract
The problem of studying the features of the dynamics of neurological deficit and cognitive functions in the early recovery period in post-COVID patients with IS and optimizing therapy is becoming of national importance and an urgent need. Purpose of the Study: To study the features of the dynamics of neurological deficit and higher brain functions in the early recovery period of ischemic stroke in post-COVID patients, with an assessment of the effectiveness of modified drug and non-drug programs of rehabilitation therapy. Materials and Research Methods: A total of 80 patients took part in the clinical study. The patients were divided into 2 groups. Group 1 - post-COVID patients with IS, Group 2 - nonCOVID patients with IS. Results: The inclusion of ethylmethylhydroxypyridine succinate and rivaroxaban in standard therapy met expectations and showed its positive role in reducing the recovery time of patients' functions, as determined using BDNF and cortisol biomarkers, as well as using data from the Rankin, Rivermead, MoCa and NIHHS scales. Conclusion: Based on the results of the obtained data, the effectiveness of the approved therapy in the rehabilitation of post-COVID patients with ischemic stroke was established.
Keywords
COVID-19, Ischemic stroke, BDNF, Cortisol, Rankin, Rivermead, MoCA, NIHSS, Ethylmethylhydroxypyridine succinate, Rivaroxaban.
Introduction
According to expert estimates of the World Health Organization (WHO), stroke is the second leading cause of death in the world. Thus, in 2016, the death rate from stroke was more than 6 million (adjusted for 2019-6.2 million) people, or 127 deaths for every 100 thousand people per year. These data are relative, since not all cases of morbidity are recorded. The incidence of stroke varies significantly in different regions - from 1 to 5-8 cases per 1000 population per year.
Relevance
The problem of studying the dynamics of neurological deficit and cognitive functions in the early recovery period in post- COVID patients with IS and optimizing therapy becomes of national importance and an urgent need, since according to observations, the disease increases the likelihood of ischemic stroke, increasing - Causes of disability and mortality of the population.
The pandemic of coronavirus infection that has swept the world's population has indirectly increased the incidence of strokes, encephalopathy and other cerebrovascular complications. Numerous observations show that patients with COVID-19 are most often exposed to hypoxia, which leads to a decrease in cerebral oxygenation, which significantly increases the development of stroke, and first of all, in patients with existing cerebrovascular diseases. COVID-19, or SARS-CoV-2, belongs to the subgenus Sarbecovirus and is the seventh known coronavirus that can infect humans. The Coronavirus Study Group of the International Committee on Taxonomy of Viruses proposed designating this virus as severe acute respiratory syndrome coronavirus 2 (MERS virus) (SARS-CoV-2) [1-14].
It is important to note that among the numerous post-COVID conditions, stroke occupies a special position. The cumulative prevalence in the review of stroke was 2%; data were extracted from 29 studies; most studies report a prevalence of 1 to 3%. This is the first time that cumulative stroke prevalence has been reported in patients with COVID-19 and points to the alarming persistent neurological morbidity associated with the pandemic.
In addition, this cumulative prevalence is noted to be much higher than previously reported for patients with influenza. Comparing the risk of stroke with COVID-19 and influenza found that the prevalence of stroke is 0.2% with influenza compared to 1.2% with COVID-19 [11]. The aim of the research in connection with the above was to study the dynamics of neurological deficit and higher brain functions in the early recovery period of ischemic stroke in post-COVID patients, with an assessment of the effectiveness of modified drug and non-drug rehabilitation therapy programs.
Materials and Methods of Research
A total of 80 patients took part in the clinical study. The patients were divided into 2 groups. Group 1-post-COVID patients with IS, Group 2-non-COVID patients with IS. Age and gender gradation in groups is presented in Table 1. In these groups, both clinical neurological and anamnestic examinations were performed in accordance with the standards of neurological examination [4,5]. The diagnosis of IS was established according to the criteria of ICD 10, the classification of Levin O.S., after taking an anamnesis, a thorough clinical and neurological examination, a study of the functions of the cognitive sphere, Magnetic Resonance Imaging (MRI).
| Groups | Average | Men | Women | ||||
|---|---|---|---|---|---|---|---|
| abc | % | Average age |
abc | % | Average Age |
||
| Group 1 (covid 19 with ischemic stroke) (n=40) | 60,7÷0,92 | 26 | 65,0 | 60,5÷1,42 | 14 | 35,0 | 60,1÷1,95 |
| Group 2 (Ischemic stroke) (n=40) | 60,3÷1,4 | 23 | 57.5 | 60,2÷1,83 | 17 | 42.5 | 60.4÷2,08 |
Table 1: Distribution of examined patients depending on by age and gender.
Non-parametric methods were used to process the results of laboratory analyzes and obtain clinical statistics. The degree of axiomaticity P was equal to 0.05. A clinical and neuropsychological assessment of patients was carried out using special scales of Rankin, Rivermead, MoCa (The Montreal Cognitive Assessment), NIHHS (National Institutes of Health Stroke Scale). Conducted neuroimaging research methods (MRI). For patients of both groups, special exercises are included (exercise therapy-therapeutic physical culture-a medical discipline that uses physical culture (mainly physical exercises) for the treatment and rehabilitation of patients)-a set of developed rehabilitation exercises to restore lost functions in the postischemic period of patients. It is known that the therapeutic effect of physical education is based on the use of one of the most important functions of any living organism-movement. It is no coincidence that Avicenna's words are still repeated-"Movement can replace many drugs, but not a single medicine can replace movement." Movement acts as a biological stimulus, stimulating the activity of organs and systems and, ultimately, normalizing their work due to the capabilities of the organism itself. Exercise is of great importance-physical exercises should be applied systematically and dosed; repetition and gradual increase in load allows you to restore impaired functions in the most optimal way, develop motor skills, and strengthen the body.
In the group of patients who had previously recovered from Covid-19 and had IS, in addition to standard therapy, Ethylmethylhydroxypyridine Succinate (EMHPS) and rivaroxaban were also used as additional drugs in the complex of rehabilitation procedures. EMHPS affects various links of free radical processes in biomembranes and inside the cell. It inhibits the processes of Lipid Peroxidation (LPO), actively reacts with primary and hydroxyl radicals of peptides, reduces the elevated level of Nitric Oxide (NO) in the brain during pathology, and on the other hand, increases the activity of antioxidant enzymes, in particular superoxide dismutase and glutathione peroxidase, responsible for neutralization of reactive oxygen species [1-3,6,12].The drugs were administered orally, after meals. Therapy with the antioxidant drug EMHPS always begins with injectable forms (saturation phase of the therapeutic effect)-2 weeks. 5 ml in physiological saline IV. Drip or jet or / m in the morning and evening. Then they switched to tablets (the phase of maximizing the therapeutic effect) 125 mg 3 times a day, and rivaroxaban tablets 20 mg 1 time a day. Exercise therapy is used more intensively-3 times a day. A group of patients with IS without a history of COVID-19 received standard therapy. The effect of the developed measures for drug and non-drug therapy was studied during the first 3 months of treatment.
Research Results
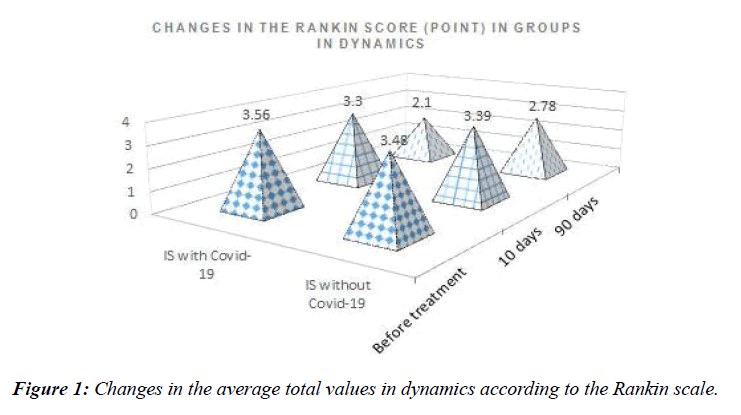
According to the Rankin scale, in the group of post-COVID patients with IS (Post-COVID with Ischemic Stroke) at the beginning of treatment, when detailed, 52.5% of patients had a moderate disability (3 points), 47.5% had a severe disability (4 points). After rehabilitation measures, a pronounced impairment of life (4 points) was noted in no one, moderate impairment of life (3 points) in 37.5%, mild impairment in 30%, normal values were noted in 32.5% of patients. In the group of patients with Ischemic Stroke without a history of COVID-19, at the beginning of treatment, 43.9% of patients had moderate disability (3 points), 56.1% had severe disability (4 points).
After rehabilitation measures, a pronounced impairment of life activity (4 points) was not noted in anyone, moderate impairment of life activity (3 points) was detected in 78%, mild impairment of life activity (2 points) in 22%, no significant impairment of life activity was noted.
Changes in the average total values in dynamics according to the Rankin scale are shown in Figure 1.
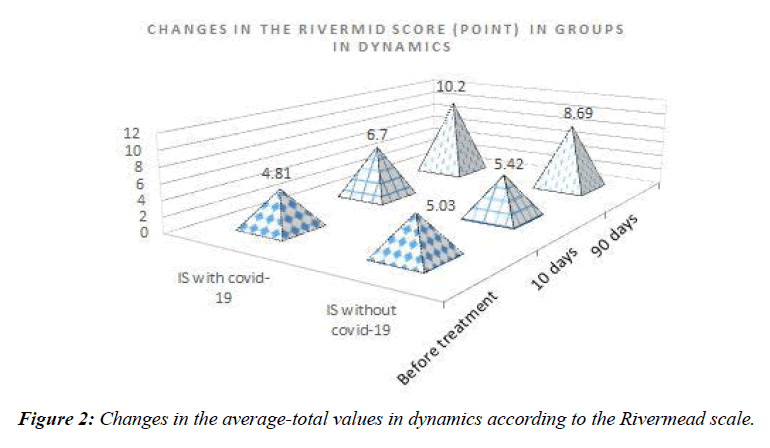
According to the Rivermead scale, 2.5% of patients scored 10–11 points in the IS with covid-19 group at the beginning of treatment, 15% of patients scored 8–9 points, 32.5% of patients scored 5–7 points, and 50% of patients scored 2–4 points. After rehabilitation measures, points were scored by 10% of patients, 11-13 points by 35% of patients, 8-10 points by 47.5% and 6-7 points by 7.5% of patients [14].
In the 1- group, according to the Rivermead scale at the beginning of treatment, 10-11 points were scored by 24.4% of patients, 8-9 points were scored by 4.9% of patients, 5-7 points by 19.5% and 0-3 points by 51.2% of patients. After rehabilitation measures, points were scored by 9.8% of patients, 10-13 points by 22% of patients, 8-9 points by 14.6% and 5-7 points by 53.6% of patients.
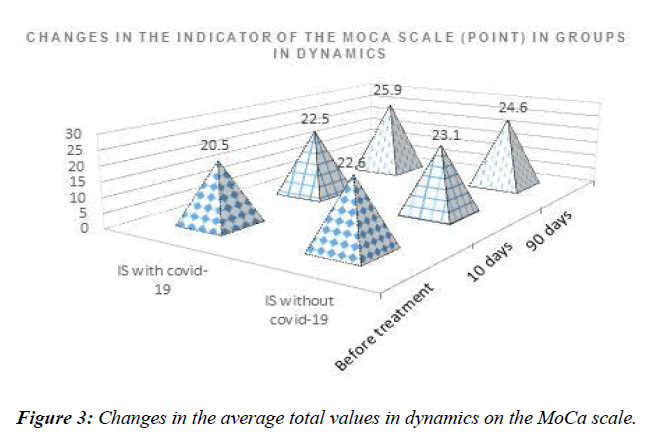
Changes in the average-total values in dynamics according to the Rivermead scale are shown in Figure 2. According to the MoCa scale in the 1 group, at the beginning of treatment, 2.5% of patients had 24 points, which corresponds to mild cognitive impairment, 32.5% - 21-23 points-moderate cognitive impairment, and 65% of patients had 19-20 points, which corresponds to severe cognitive impairment. After rehabilitation measures, recovery to normal levels was noted in 70% (26-28 points), in 17.5% of patients it remained at the level of 24-25 points and in 12.5% of patients at the level of 21 points.
In the second group of patients, before treatment, 12.5% (5) of patients had mild cognitive impairments, 87.5% (35) had moderate cognitive impairments, and no patients with severe cognitive impairments were found. After rehabilitation measures, recovery to normal levels was noted in 12.2% (26-27 points), in 43.9% of patients it remained at the level of 24-25 points, in 26.9% of patients at the level of 22-23 points and 17,1 at level 21 points. Changes in the average total values in dynamics on the MoCa scale are shown in Figure 3.
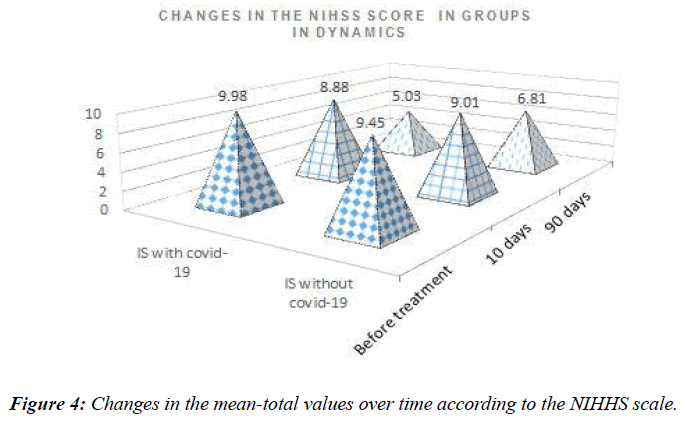
According to the NIHHS scale used to determine the level of neurological deficit in the covid group with stroke at the beginning of treatment, 12.5% of patients had severe neurological disorders (13 points), 62.5% had moderate neurological disorders (9-12 points) and in 25% of mild degree (7 points). After rehabilitation measures, 2.5% of patients had moderate neurological disorders (9 points), 85% had mild neurological disorders (3-8 points), and 12.5% (2 points) were assessed as satisfactory according to the NIHHS scale.
In the second group, according to the NIHHS scale, before treatment, 17.1% of patients had severe neurological disorders (13 points), 58.6% had moderate neurological disorders (9-12 points) and 24% had mild neurological disorders (7 points). After rehabilitation measures, 39.1% of patients had moderate neurological disorders (9-11 points), and 60.9% of patients had mild neurological disorders (4-8 points). Changes in the mean-total values over time according to the NIHHS scale are shown in Figure 4.
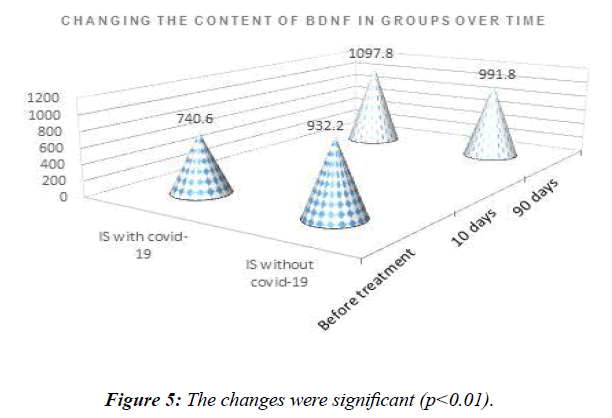
In the study of the quantitative content of cerebral neurotrophic factor (BDNF) in blood serum before treatment in patients of the first group in the recovery period after suffering an Ischemic stroke, the content of BDNF was 740.6 ± 34.5 pg/ ml, by the end of the study it rose to 1097.8 ± 42.1 pg/ml. The changes were significant (р˂0.01, Figure 5).
In patients of the comparison group before treatment, the content of BDNF was 932.2 ± 42.6 pg/ml, by the end of the study it rose to 991.8 ± 42.8 pg/ml. The changes were not significant (p>0.05, Figure 5).
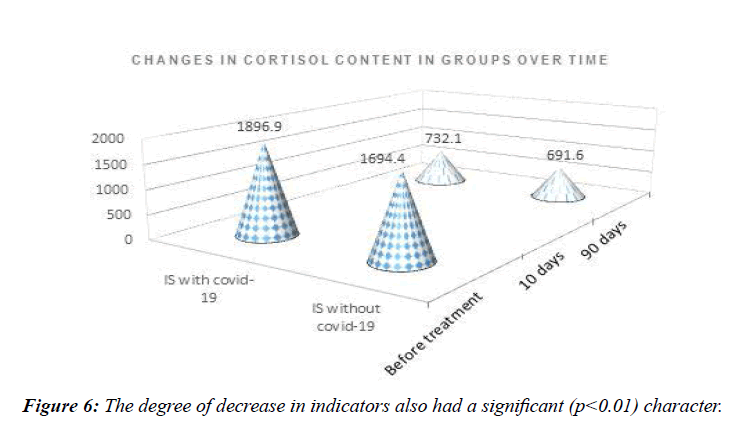
By determining the level of cortisol in the covid group with stroke, its values at the beginning of the recovery period were set at the level of 1896.9 ± 24 ng/ml, which decreased to 732.1 ± 23.6 ng/ml by the end of the study. The degree of decrease in indicators also had a significant (р˂0.01) character (Figure 6).
Cortisol levels in the non-covid group with stroke were set at the beginning of the recovery period at the level of 1694.4 ± 54.3 ng/ml, by the end of the study it decreased to 691.6 ± 32.1 ng/ml. The degree of decrease in indicators also had a significant (р˂0.01) character (Figure 6).
Discussion
The pandemic of coronavirus infection that has swept the world's population has indirectly increased the incidence of strokes, encephalopathy and other cerebrovascular complications. Numerous observations show that patients with COVID-19 are most often exposed to hypoxia, which leads to a decrease in cerebral oxygenation, which significantly increases the development of stroke, and first of all, in patients with existing cerebrovascular diseases [13]. COVID-19, or SARS-CoV-2, belongs to the subgenus Sarbecovirus and is the seventh known coronavirus that can infect humans [10]. The Coronavirus Study Group of the International Committee on Taxonomy of Viruses proposed designating this virus as severe acute respiratory syndrome coronavirus 2 (MERS virus) (SARS-CoV-2) [7,8,14].
Analysis of data for 3 months showed that in all indicators of the scales there are positive relationships with their values before and after treatment. The more pronounced the indicators on the values of the scales before treatment, the more pronounced the indicators on the values of the scales after treatment.
For this, an analysis of the relationship between the scales used was carried out using a correlation analysis in both groups. The Pearson correlation coefficient was used. In the course of the analysis, interrelationships between changes in the scale indicators, expressed to varying degrees, were identified.
Conclusion
Post-covid patients admitted with ischemic stroke showed worse rates of recovery of cognitive and neurological deficits compared with patients without a history of COVID-19. The initial level of BDNF in post-COVID patients was significantly lower (740.6 pg/ml, p<0.01) than in patients without a history of COVID-19 (932.2 pg/ml). An average negative correlation was established between the amount of BDNF and cortisol (r = -0.476, p<0.01), which shows that the higher the level of cortisol, the lower the content of BDNF, which has a strong correlation with the worst results of the neuropsychological test MoCA (r=0.71, p<0.01). Against the background of drug and non-drug correction in post-covid 19 patients with ischemic stroke, the rehabilitation period is accelerated, which is confirmed by a significant (p<0.01) improvement in the scores of Rankin, Rivermead, MoCa and NIHSS, neurotrophic factor BDNF.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Financial Support
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgements
All authors participated in the research process and data collection
References
- Voronina TA. New directions in the search for nootropic drugs (problem article). Bulletin of RAMN. 1998;(1):16-21.
- Voronina TA. Mexidol: spectrum of pharmacological effects. SS Korsakov J Neurol and Psychiatr. 2012;112(12): 86-90.
- Kuznetsov YuV., Matyushin IA., Smirnov LD., et al. Study of the antioxidant activity of new analogs of ethylmethylhydroxypyridine succinate and hydroxypyrididobenzimidazole derivatives. Bulletin of New Med Technol. 2006;13(3):9-10
- Mikhailenko AA. Clinical practice in neurology. Publisher: SPb: Foliant. 2001:480.
- Skoromets AN. Topical diagnosis of diseases of the nervous system: A guide for doctors. 2012:623.
- Bashkatova V, Narkevich V, Vitskova G, et al. The influence of anticonvulsant and antioxidant drugs on nitric oxide level and lipid peroxidation in the rat brain during penthylenetetrazole-induced epileptiform model seizures. Progress in Neuro-Psychopharmacol and Biol Psychiatr. 2003;27(3):487-92.
- Gorbalenya AE, Baker SC, Baric RS, et al. Severe acute respiratory syndrome-related coronavirus: The species and its viruses–a statement of the Coronavirus Study Group. BioRxiv. 2020.
- Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. The Lancet. 2020;395(10224):565-74.
- Mao L, Wang M, Chen S, et al. Neurological manifestations of hospitalized patients with COVID-19 in Wuhan, China: a retrospective case series study. MedRxiv. 2020.
- Nicholas J. Beeching, Tom E. Fletcher. Robert Fowler.COVID-19. BMJ Best Practices. BMJ.2020.
- Misra S, Kolappa K, Prasad M, et al. Frequency of neurological manifestations in COVID-19: a systematic review and meta-analysis of 350 studies. MedRxiv. 2021.
- Voronina TA. Present-day problems in experimental psychopharmacology of nootropic drugs. Neuropharmacology. Harwood Academic Publ GmbH UK. 1992;2:51-108.
- Wu Y, Xu X, Chen Z, et al. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain, Behavior, and Immunity. 2020;87:18-22.
- Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China, 2019. New Eng J Med. 2020.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref