- Biomedical Research (2015) Volume 26, Issue 3
Sociodemographic characteristics of patients with Demodex brevis and Demodex folliculorum infestation and its association with rosacea and Behçet?s disease
Suleyman Durmaz1*, Erkan YULA2, Ozlem AYCAN KAYA3, Aysegul AKSOY GOKMEN2, Cetin KILINC4, Metin ATAMBAY5, Ozlem EKIZ6, Harika GOZUKARA BAG7, Bayram PEKTAS21Konya Numune Hospital, Microbiology Laboratory, Konya, Turkey
2Department of Medical Microbiology, Faculty of Medicine, University of Katip Celebi Izmir, Turkey
3Department of Medical Parasitology, Faculty of Medicine, University of Mustafa Kemal, Hatay, Turkey
4Department of Medical Microbiology, Faculty of Medicine, University of Mustafa Kemal, Hatay, Turkey
5 Department of Parasitology, Faculty of Medicine, University of Inonu, Malatya, Turkey
6Department of Dermatology, Faculty of Medicine, University of Mustafa Kemal, Hatay, Turkey
7Department of Biostatistics, Faculty of Medicine, University of Inonu, Malatya, Turkey
- *Corresponding Author:
- Suleyman DURMAZ
Konya Numune Hospital Microbiology Laboratory
Konya, Turkey 42003, Konya, Turkey
Accepted date: March 03 2015
Abstract
Demodex mites are ectoparasites often found in the skin thought to be associated with the development of some skin diseases. Demodex positivity may be affected by several factors. In order to determine the relationship between Demodex infestation and rosacea disease (RD), Behçet’s disease (BD) and various individual parameters such as gender, personal hygiene and skin type. A total of 238 individuals (61 with RD, 46 with BD, and 131 healthy subjects) were investigated for the presence of Demodex folliculorum and D. brevis using the standardized skin surface biopsy technique and a questionnaire. The incidence of Demodex mites in RD patients was significantly higher when compared to the control group (p=0.010 and p=0.001, respectively). However, there was no difference between those with BD and the control group. There was a significant difference between ages of groups, skin types, use of moisturizer, and itching, without taking into account the presence of Demodex among the disease groups (p<0.05). On the other hand, there was no significant difference between disease groups in terms of data of gender, skin care, epilation, and face washing. Our study reveals that the positivity rates of Demodex mites in rosacea patients were significantly higher. Mean ages of groups, skin types, use of moisturizer, and the presence of itching of the ear and face may be associated with higher density of Demodex mites.
Keywords
Rosacea, Behçet’s Disease, D. folliculorum, D. brevis, Sociodemographic characteristics.
Introduction
Demodex folliculorum (D.f.) and Demodex brevis (D.b.) are ectoparasites often found in the follicles of facial skin. D.f. is usually found in the follicular infundibulum and D.b. in the sebaceous ducts and meibomian glands [1]. These mites are common commensals of the pilosebaceous units of the face, scalp and upper chest. Demodicosis (or “demodicidosis”) is the term applied to cutaneous diseases caused by Demodex mites. The parasite is found in large numbers on the face and in other areas of the body where sebum formation is abundant, but the pathogenic role of D.f. mites in human dermatopathology is still a matter of debate. Dominating dermatologic concepts define infestation as evidence of living D.f. mites at a density of five or more mites per square centimeter of skin surface (demodicidosis); these mites are usually considered to play a pathogenic role when they multiply, and rarely penetrate the dermis [2]. In infected humans who have no symptoms, Demodex mite density was shown to be <5 parasites/cm2 of skin [3]. The pathogenic mechanisms of transmission of these mites are still unknown; however, human-to-human transmission by close contact is assumed. Today, the medical importance of this phenomenon still draws discussion. Mite density in healthy skin is age dependent, increases with age, and reaches up to 100% in elderly people. In addition, it is claimed that Demodex has been associated with the development of rosacea, pityriasis folliculorum, perioral dermatitis, seborrheic dermatitis, pustular eruption, blepharitis, seborrheic alopecia, and other skin lesions such as rosacea and sebaceous adenoma [4-8].
The pathophysiology of rosacea disease (RD) remains unknown. A leading theory suggests a vascular basis; however, clinical observations and histopathologic studies suggest that inflammation of the pilosebaceous follicle may be central to the pathogenesis of rosacea [9]. According to evidence from biopsies of the skin surface; individuals with RD have a higher density of Demodex spp. Morever, Demodex spp. is considered to be an important factor in the etiology of the disease. Increased blood flow in papillary dermal vessels provides the possibility of invasion of the dermis, or that the vessels act as a favorable habitat for Demodex spp. In addition, it is considered that the parasites may contribute to the development of rosacea lesions by mechanically blocking the follicular gap, or by acting as vectors to microorganisms.
Behçet’s disease (BD) is a chronic, relapsing, multisystemic, idiopathic, and inflammatory disease, with classical symptoms consisting of oral aphthous ulcers, genital ulcers, and uveitis [10]. Vasculitis of arteries and veins is an important feature of BD. BD is likely mediated by a combination of genetics, infectious agents, immune dysregulation, and inflammatory mediators, such as shock proteins, oxidative stress, lipid peroxidation, and environmental factors. Although the exact cause of BD is unknown, researchers have focused on genetic predisposition, environmental factors, and infectious agents such as bacteria or viruses. There is limited knowledge about dermatological parasite infestation in patients with BD. A growing number of case reports and epidemiological studies show that Demodexhas an aversion for skin lesions of the face. Therefore, the infestation of Demodex has been recognized by many researchers as one of the important causes of skin diseases, and has increasingly become a public health concern [11,12].
The aim of this study was to determine the relationship between Demodex infestation and RD, BD and various individual parameters.
Material and Methods
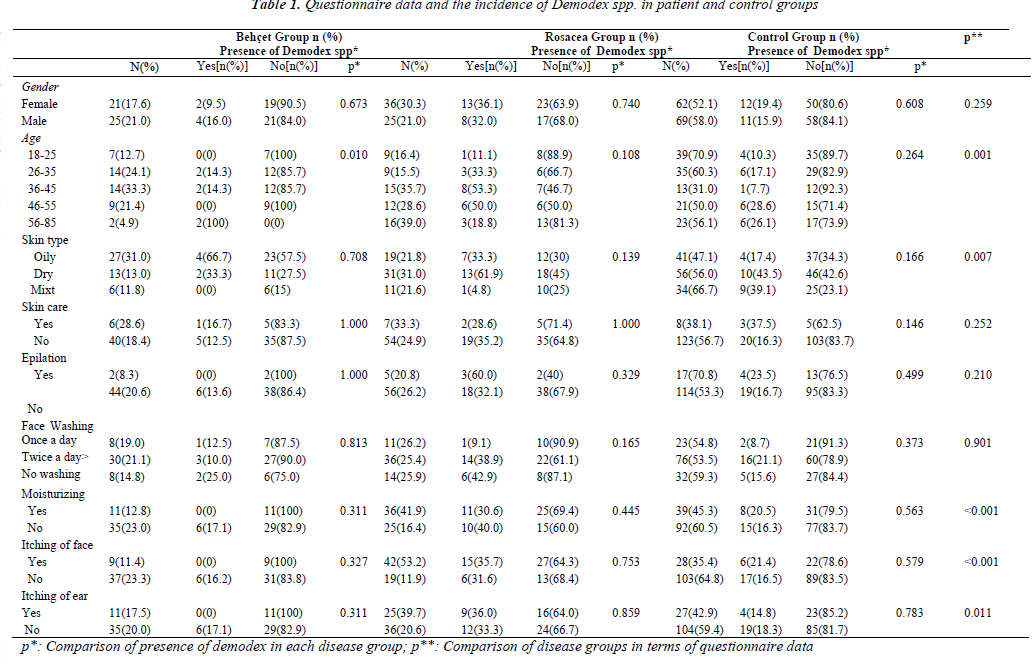
The ethics committee of Inonu University Faculty of Medicine approved the study, and written informed consent was obtained from all patients and controls. Patients diagnosed with RD and BD at the Clinics of Department of Dermatology, were recruited for this study between June 2012 and July 2013 RD was diagnosed clinically and International Behçet’s Study Groups criteria were used for diagnosis of BD. Control subjects were selected from healthy people who did not have any skin diseases. The exclusion criteria for the groups (RD, BD, and control groups) were as follows; age<18 years, another dermatological disease on the face (such as herpes infection, impetigo, perioral dermatitis, seborrheic dermatitis, lupus erythematosus), pregnancy or lactation, systemic diseases (such as diabetes mellitus, malignancy malignancy), receiving phototherapy, radiotherapy or chemotherapy, topical a caricidal usage, and use of oral or topical antibiotics in the previous month. Demographic data were collected by preparing a questionnaire for patients and controls. Information on age, gender, skin type (dry, oily, and mixed), skin care, epilation, frequency of face washing, itching of the face and ear data were collected (Table 1).
The presence of Demodex mites was determined by standardized skin surface biopsy (SSSB) technique in patients and control groups.In this method, clinical samples were taken with cyanoacrylate containing glue. Before taking samples, the selected skin regions (nose, chin, left cheek, right cheek, and forehead) were cleaned and dried to remove cream and lotions from the skin where samples were taken. Sample sites were cleaned with alcohol. A 1-cm2- circle was drawn on one side of a slide with a glass pen, and 1 ml of adhesive containing cyanoacrylate was applied to other side. After one minute, the adhesive side of slide was pressed onto the skin of the individuals. After preparing the slide by adding 1 ml Hoyer solution to the sample, the density of Demodex spp. was evaluated with light microscopy technique using x40 and x100 zooming. The determination of five and more parasites/cm2 area was diagnosed as infestation.
Statistical analysis
The minimum, maximum and median values were used for identification of quantitative data. Categorical data were defined as the percentage of number and line. Chi-square and Fisher’s exact chi-square tests were used in comparison of categorical variables. The Mann- Whitney U test was used for comparison of between control groups and disease groups. A p-value less than 0.05 was considered as significant.
Results
There were 107 patients in total [61 with RD, 36 female (59.0%), 25 male (41.0%), mean age 44.66 ± 15.69 years, range 18–83; and 46 with BD, 21 female (45.7%), 25 male (54.3%) mean age 38.02 ± 12.02 years, range 21–80]. The control group consisted of 131 participants [62 (47.3%) female, 69 male (52.7%); mean age 38.46 ± 16.84 years, range 18-84]
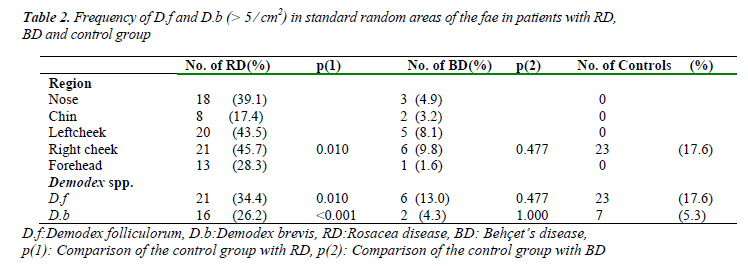
Demodicidosis was found in 21 patients with RD (34.4%); in six patients with BD (13.0%); and in 23 controls (17.6%). D.f. was found to accompany D.b. in all detectedonly in the right cheek area in the control group. The incidence of D.f. and D.b. in RD patients was significantly higher than the control group (p=0.010 and p=0.001, respectively); there was no difference in the BD group in terms of D.f. and D.b incidence (p=0.477 and p=1.00, respectively) (Table 2).
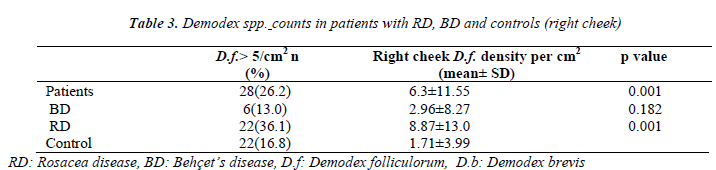
As shown in Table 3, parasite density was mostly detected in the right cheeks of RD patients. Mean D.f. density (in the right cheek) was 6.3 ±11.55⁄cm2 (range 0–40) in the patient group, and 1.71 ±3.99⁄cm2 (range 0–15) in the control group (Table 3).
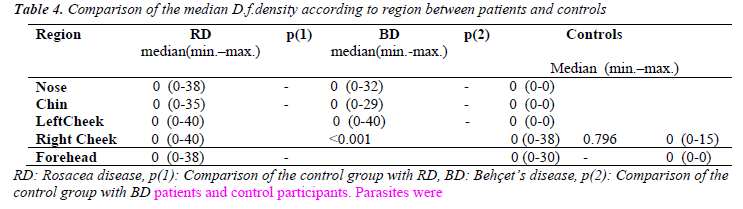
The p-value of just the right cheek was calculated to compare BD and RD patients and those in the control group (Table 4). There was no significant difference when comparing the presence of D.f. occurrence in the right cheeks of the control group and BD patients, but there was a significant difference in comparing the control group with RD patients (p<0.001). While there was a significant difference between age groups in terms of the presence of Demodex in BD patients (p=0.001), there was no significant difference in other parameters. There was a significant difference between the ages of groups, skin types, use of moisturizer, and itching without taking into account the presence of Demodex, according to the disease groups (p<0.05). However, there was no significant difference between disease groups in terms of gender, skin care, epilation, and face washing (Table 1).
There was no significant difference between gender, skin type, skin care, epilation, face washing, use of moisturizer, and itching of the face and ear in terms of the presence of parasites between the BD and control groups. However, there was a significant difference between mean age of groups in terms of the presence of Demodex spp. in BD patients (p=0.010). There was no significant difference between gender, age, skin type, skin care, epilation, face washing, moisturizing, and itching of the face and ear in terms of the presence of Demodex spp. in RD patients (Table 1).
There was a statistically significant difference between age, skin type, use of moisturizer, and itching of face and ear when comparing patient groups with questionnairedata, without taking into account the presence of Demodex (p=0.001, 0.007, <0.001, <0.001, 0.011, respectively). There was no significant difference in terms of gender, skin care, epilation, and face washing (Table 1).
Discussion
Demodex folliculorum is a universal ectoparasite which is believed to play a major etiopathogenic role in a variety of skin diseases. Their role in human diseases is under investigation, and a growing number of studies indicate that they contribute to chronic inflammatory conditions of the skin, such as rosacea, blepharitis, otitis externa, alopecia and folliculitis [13,14]. Demodex infestation has been investigated previously, particularly in rosacea. However, there have been no study reported investigating the sociodemographic characteristics of BD and RD in terms of Demodex infestation.
Various techniques, including skin scraping, skin pressurization, cellophane tape method, SSSB, skin biopsy, hair epilation, and comedo extraction, have been used to detect Demodex mites. It has been suggested that the SSSB technique defined by Marks and Dawber facilitates the diagnosis by detection of the liquid amount in cm2 due to the complete gathering of the follicle content with the surface of the skin’s corneal layer where the D.f.’s are located. Therefore, this has been our preferred research technique [15].
Our results revealed that gender was not statistically correlated with Demodex infestation. This finding is in accordance with the conclusions of previous reports [16-19]. In addition, we found that gender was not statistically correlated with Demodexinfestation in patients with RD and BD.
Studies have shown that Demodex infestation rates elevated with age [20-22]. Only newborns are completely free of the mites, and acquire them almost as soon as they are picked up by their mothers and other family members. In accordance with the other studies, we found statistically significant differences between age groups (18-25 and 56-85 years) and BD patients. We believe Demodex spp. prevalence in the study population may have reached the upper limit by aging, due to the fact that the skin of elderly peoples is mature, and a great deal of follicular and sebaceous gland cells can provide Demodex with abundant nutrition. Demodex infestation could cause hyperkeratosis and follicular orifices can be easily blocked. Therefore, large amounts of Demodex mites would parasitize and reproduce in hair follicles.
According to the literature, the rate of Demodex infestation increases in patients with oily and mixed skin types [16,17,22]. Similar results were obtained in our study.
The possible underlying mechanism is that the sebaceous glands in oily or mixed skin are more numerous and more sophisticated, which could provide a suitable environment for the growth of Demodex mites.
It was considered that bad hygieneand skin care may provide a suitable medium for parasite infestation. In our study, it was found high percentage of positivity that doesn’t make skin care in all patient groups. However, there were no significant differences between them due to the small sample size. Another explanation; washing the face cleans the skin surface, but may not effectively eliminate the Demodex mites in hair follicles and sebaceous glands.
Marufi et al. [23] found D.f. in the external ear skins of the two patients who reported external ear itching. Ding et al. [24] investigated the incidence of D.f. and D.b. in secretions of the external ear canal, and found a positive result in 11.58% of the slides. In another study, D.f. was reported in the external ear skin of two patients who had itching of the external ear canal, but the itching was attributed to other causes [25]. Our study found a statistically significant difference between itching of the ear and the presence of Demodex infection.
In the present study, we found no statistically significant difference in both disease groups in terms of epilation and incidence of Demodex infestation. We expected a lower incidence of Demodex in patients who undergo epilation due to the removal of the follicle content that feeds the Demodex; however, there was no significant difference. We expected that a better hygiene regimen with increased face washingto lessen the fat content on the face would result in decreased Demodex infection. Our results showed that the incidence rate of Demodex spp.decreased as face washing increased; however, this cannot be confirmed due to the small sample size, and to the numeric difference between subjects who washed their faces one or more times. We did not find any other studies where such habits have been examined in the literature.
Rosacea is a chronic inflammatory relapsing disorder of the facial skin characterized by transient or persistent erythema and telangiectasia, and, frequently, papules and pustules. This disease has been observed most frequently in patients with pale skin and light eyes [26,27]. Various factors have been proposed for the pathogenesis of rosacea, although the precise etiology is still unknown. A wide variety of theories about the pathomechanism have been proposed. The possible etiologic factors are grouped into the following categories: vasculature, climatic changes, matrix degeneration, chemicals and ingested agents, inflammation of the pilosebaceous unit, and microbial organisms [28]. Recently, other studies have pointed out that Demodex parasites are associated with the pathogenesis of RD. Histopathological examination of skin biopsies of RD patients often show a follicular-oriented inflammatory response, and Demodex mites are frequently observed using the skin surface biopsy technique which extracts mites from follicular canals [29,30]. In addition, movement of the mites inside the pores of the skin irritates the skin, and the skin responds to irritation by producing more oil. In some people who have RD, the combination of oil and Demodex infestation could trigger a vicious cycle that keeps the skin sensitive to the environmental triggers that cause RD.
Roihu et al.[31] found that the mite prevalence in their study’sRD group (51%) was significantly higher than in the rest of the study population (eczema 28% and lupus discoides 31%). It has been reported that the prevalence of Demodex mitesin patients with acne rosacea (38.6%) was significantly higher than in patients with discoid lupus erythematosus (21.3%) and actinic lichen planus patients (10.6%) (p< 0.001)(38). Topical immunosuppression with steroid may be another cause of demodicosis. It has been suggested that topical steroids can cause rosacea-like lesions on previously healthy skin, or may exaggerate symptoms of demodicosis [32,33]. Abd-El-Al et al.[34] revealed the pathogenesis of D.f. in rosacea, and found 28.6/cm2 to be the highest density of mites detected in a single patient’s cheek which was measured by using the SSSB technique in 16 patient diagnosed with papulopustular rosacea. Forton et al.[30] performed a standardized skin-surface biopsy (1 cm2) of the cheeks of 49 rosacea patients. They found the density of Demodex was significantly higher in patients with RD than in controls (mean = 10.8/cm2; p < 0.001). In accordance with this study, we found that the incidence of D.f. and D.b. in RD30 patients was significantly higher when compared with the control group. In our study, demodicidosis was found in 21 patients with RD (34.4%), and also that the parasite density was mostly detected in the right cheeks of RD patients (Mean density = 6.3 ± 11.55⁄cm2). Demodex mites do not like to live in normal skin, and usually prefer dry, or, more likely, oily skin. Moisturizing dry skin and reducing the oiliness of oily skin may reduce the risk of infestation and rosacea.
BD is a systemic inflammatory disease which presents with recurrent oral aphtha, cutaneous manifestations, uveitis, and genital ulcer. The etiology of BD remains unknown. However, environmental factors may trigger the disease, as well as infectious agents, bacteria or viruses, and genetic predisposition [34]. There are limited studies investigating the relationship between BD and Demodex parasites in the literature. Emre S et al.[35] investigated D.folliculorum prevalence among 40 patients with BD in cheek and eyelashes samples taken using the SSSB technique. They found 7.5% positivity for BD in cheek skin samples, and 10% for control group patients (p<0.05). However, they reported that D.f. prevalence was significantly different between eyelash samples (65%) for BD patients who took several combinations of medications and the control group (10%).Immunosuppression may stimulate the pathomechanism in the clinical manifestation of demodicosis, particularly following corticosteroid use or chemotherapy, or due to diseases of an immunocompromised nature, such as AIDS or malignancy. On the other hand we found no significant difference when comparing the presence of D.f. in the right cheeks of the control group and BD patients.
Conclusion
Our study demonstrates that the positivity rates of Demodex mites in rosacea patients were significantly higher compared to the control group. However there was no difference between BD and control groups. Age group, skin type, use of moisturizer, and presence of itching of the ear and face may be associated with a higher density of Demodex mites. This parasite should be kept in mind under similar clinical conditions to manage the specific symptoms which manifest.
Conflict of interest
The authors have not declared any conflicts of interest.
Ethical standards
The experiments comply with the current laws of the Republic of Turkey.
A part of this study was presented as poster presentation at First Turkish Congress of One Healt in Konya/Turkey at 9-10 April 2015
References
- Desch C, Nutting WB. D. folliculorum(Simon) and D.brevisAkbulatova of man:redescripton and reevaluation. J Parasitol 1972; 58(1): 169-177.
- Forton, F, Seys B, Marchal J, Song M. D. folliculorumand topical treatment: a caricidal action evaluated bystandardized skin surface biopsy. Br J Dermatol 1998;138(3): 461-466.
- Forton F. Standardized skin surface biopsy: method to estimate the Demodexfolliculorumdensity, not to study the Demodexfolliculorumprevalence. J EurAcadDermatolVenereol 2007; 21(9): 1301-1302.
- Erbagcı Z, Ozgoztaşı O. The significance of D. folliculorumdensity in rosacea.Int J Dermatol 1998; 39(1):743-745.
- Karincaoglu Y, TepeB, Kalayci B, Atambay M, SeyhanM. Is Demodexfolliculorum an aetiological factor inseborrhoeic dermatitis? ClinExpDermatol 2009; 34(8): 516-520.
- Yula E, Aycan-Kaya O, Atambay M, Doganay S, DaldalN, Tuzcu AE. What is the importance of Demodexfolliculorumand D. brevisin etiology of blepharitis.TurkiyeKlinikleri J Med Sci 2013; 33(2): 420-424.
- Gokce C, Aycan-Kaya O, Yula E, Ustun I, Yengil E, Sefil F, Rizaoglu H, Gultepe B, Bayram F. The effect of blood glucose regulation on the presence of opportunistic Demodexfolliculorummites in patients with type 2 diabetes mellitus. Journal of International Medical Research 2013; 41(5): 1752-1758
- Cevik C, Aycan-Kaya O, Akbay E, Yula E, Yengil E, Gulmez M.I, Akoglu E. Investigation of demodexspecies frequency in patients with a persistent itchy ear canal treated with a local steroid. J Laryngol Otol. 2014; 128(8): 698-701.
- Erbagci Z, Ozgoztasi O. The significance of Demodexfolliculorumdensity in rosacea.Int J Dermatol 1998;37(6): 421-425.
- Cekmen M, Evereklioglu C, Er H, Inaloz HS, DoganayS, Turkoz Y, Ozerol IH. Vascular endothelial growth factor levels are increased and associated with disease activity in patients with Behçet's syndrome. Int J Dermatol 2003; 42(11): 870-875.
- Baima B, Sticherling M. Demodicidosis revisited. ActaDermVenereol 2002; 82(1): 3-6.
- Karincaoglu Y, Bayram N, Aycan O, Esrefoglu M. The clinical importance of Demodexfolliculorum presenting with nonspecific facial signs and symptoms. J Dermatol 2004; 31(8): 618-626.
- Elston DM. Demodex mites as a cause of human disease. Cutis 2005; 76(5): 294-296.
- Burns DA. Follicle mites and their role in disease.ClinExpDermatol 1992; 17(3): 152-155.
- Marks, R., Dawber, RPR. Skin surface biopsy: an improved technique for the examination of the horny layer. Br J Dermatol 1971; 84(1):117-123.
- He X, Chen YZ, Wu SY, Zhang CF, Wang QH, Pan LL. Investigation and analysis of Demodex mites infection of students in Fujian Medical University. Strait J Prev Med 2009; 15(1): 39-40.
- Cao YS, You QX, Wang L, Lan HB, Xu J, Zhang XH, Yang H, Xiong YJ, Tian XF. Facial Demodex infection among college students in Tangshan. Chin J ParasitolParasitic Dis 2009: 27(3): 271-273.
- Wang AH, Wang T. Analysis of the relation between the facial skin diseases and the infection of demodicid mites in teenagers. Mod Prev Med 2008; 35(17): 3396- 3399.
- Bonnar E, Eustace P, Powell FC. Demodex mite innormal skin. Lancet 1991; 337(8750): 1168.
- Bonnar E, Eustace P, Powell FC. The Demodex mite population in rosacea. J Am AcadDermatol 1993; 28(3): 443-448.
- Gao JL, Tao YF, Hu LH, Chen Q, Zhao JM, Yan LY. Study on Demodex infection in facial disease patients and relative risk factors. Zhejiang J Lab Med 2008; 6(2): 26-27.
- Yang XM, Luo Y. Survey of infectious status of facial vermiform mite in some primary school pupils and middle school students in Haikou City. China Trop Med 2006; 6(8): 1532-1533.
- Marufi M, Ozturkcan S, Ozcelik S, Saygı G. D. folliculorumin the skin of external ear canal in patientssuffering from ear ıtching (report of two cases) TurkiyeParazitolDerg 1996; 20(3): 357-359.
- Czepita D, Kuzna-Grygiel W, Czepita M, Grobelny A. Demodexfolliculorum and Demodexbrevis as a cause of chronic marginal blepharitis. Ann Acad Med Stetin.2007;53(1):63-67.
- Ding Y, Huang X. Investigation of external auditory meatus secretion Demodexfolliculorum and Demodex breuis infection in college students. Lin Chuang Er Bi Yan HouKeZaZhi, 2005; 19(4): 176-177.
- Jansen T. Clinical presentations and classification of rosacea. Ann DermatolVenereol 2011;138(3):192-200.
- Scheinfeld NS. Rosacea.Skinmed 2006; 5(4): 191-194.
- Crawford GH, Pelle MT, James WD. Rosacea: I. Etiology, pathogenesis, and subtype classification. J Am AcadDermatol 2004; 51(3): 327-341.
- Powell FC. Rosacea and the pilosebaceous follicle.Cutis 2004; 74(3): 9-12.
- Forton F, Seys B. Density of Demodexfolliculorumin rosacea: a case control study using standardized skin surface biopsy. Br J Dermatol 1993; 128(6): 650–659.
- Roihu T, Kariniemi AL. Demodex Mites in Acne Rosacea. J CutanPathol 1998; 25(10): 550-552.
- Moravvej H, Dehghan- Mangabadi M, Abbasian MR, Meshkat- Razavi G. Association of rosacea with demodicosis. Arch Iran Med 2007; 10(2): 199-203.
- Egan CA, Rallis TM, Meadows KP, Krueger GG. Rosacea induced by beclomethasonedipropionate nasal spray. Int J Dermatol 1999; 38(2): 133-134.
- Abd-El-Al AM, Bayoumy AM, Abou Salem EA. A study on Demodexfolliculorum in rosacea. J Egypt SocParasitol 1997; 27(1): 183-195.
- Emre S, Aycan OM, Atambay M, Bilak S, Daldal N, Karincaoglu Y. What Is The Importance of Demodex folliculorum in Behçet’s disease? TurkiyeParazitol Derg 2009; 33(2): 158-161.