- Biomedical Research (2012) Volume 23, Issue 2
Serum vitamin D and metabolic syndrome among postmenopausal women in Gorgan
Abdoljalal Marjani1 and Sedigheh Moghasemi21Department of Biochemistry and Biophysics, Biochemistry and Metabolic Disorder Research Center, Gorgan Faculty of Medicine, Golestan University of Medical Sciences, Gorgan, Golestan Province, Iran
2Department of Midwifery, Golestan University of Medical Sciences, Gorgan, Golestan Province, Iran
Accepted date: February 25, 2012
Abstract
In this study, we aimed to assess levels of serum 25-hydroxyvitamin D in relation to metabolic syndrome among postmenopausal women in Gorgan. The study group included 100 postmenopausal women who were referred to the different Health Centers in Gorgan. Body mass index, waist circumference, Hip, waist to hip ratio, diastolic blood pressure, triglyceride, fasting blood glucose and 25-hydroxyvitamin D levels were significantly higher in postmenopausal women with metabolic syndrome, but HDL-cholesterol was lower. Prevalence of the metabolic syndrome was 31%. There were significant differences in 25-hydroxy vitamin D of postmenopausal women with and without vitamin D deficiency. Prevalence of the vitamin D deficiency in postmenopausal women was 30%. There were significant differences in 25-hydroxy vitamin D of postmenopausal women with and without vitamin D deficiency who had metabolic syndrome. Our results show that postmenopausal status might be a predictor of metabolic syndrome in this area. Our findings suggested that vitamin D levels have no association with metabolic syndrome. There were no significant differences in vitamin D levels in postmenopausal women with and without metabolic syndrome. Vitamin D deficiency is not associated with the metabolic syndrome.
Keywords
Gorgan, Metabolic syndrome, Vitamin D, postmenopausal women
Introduction
Vitamin D deficiency and insufficiency is the most health problem among postmenopausal women worldwide. Some finding suggests that low levels of serum 25 - hydroxyvitamin D (25(OH) D) could be associated with elevated risk of cardio metabolic disorders comprising cardiovascular disease [1-3] type 2 diabetes [4]. Some studies show that there is a relation of serum 25(OH) D to fasting glucose [5,6]. Low serum 25(OH) D concentrations could be associated with dyslipidemia [7–9]. There are few studies of the relation of serum 25(OH) D levels to metabolic and lipid markers. Vitamin D deficiency could be a risk factor for the metabolic syndrome [10,11]. There is little evidence about the relationship between vitamin D status and metabolic syndrome. A possible role of vitamin D deficiency in the pathogenesis of the metabolic syndrome has been mentioned [9,12,13]. Cardiovascular disease is one of the main reasons of death among women in the world [14]. Studies show that women aged older than 55 years old show a higher incidence of cardiovascular disease than younger women [15-17]. Other studies showed that there is a high prevalence of metabolic syndrome in postmenopausal women, which was changed from 32.6% to 41.5 % [18-20]. Study of Rossi et al [21] showed that postmenopausal women with metabolic syndrome had less preferable cardiovascular risk factors. The mechanism which explains the effect of menopause on the cardiovascular system remains unknown [22]. Some studies show that there is no difference in cardiovascular risk factors when compared premenopausal with postmenopausal women [22-25]. In several studies, the incidences of metabolic syndrome in postmenopausal women were increased in whole world [26,27]. Some epidemiological studies [9,28-30] showed that 25 (OH) D statuses is conversely collaborated with metabolic syndrome in western populations [31,32]. There is limited evidence from the Asian population. Some studies showed that there are ethnic differences in vitamin D metabolism and its nutritional status [10,33]. In Asian countries, metabolic syndrome has become one of the most health problems [34]. There is little information about the relationship of vitamin D deficiency and prevalence of metabolic syndrome among Asian populations. In this study, we aimed to assess levels of serum 25(OH) D in relation to metabolic syndrome among postmenopausal women in Gorgan (South East of Caspian Sea), Iran.
Material and Methods
This cross sectional study was performed in the Biochemistry and Metabolic Disorders Research Center of Gorgan, Golestan province (South East of Caspian Sea, North East of Iran) in 2011. The study group included 100 subjects with postmenopausal women who were referred to the different Health Centers in Gorgan. Postmenopausal women who had at least 1 year, history of cessation of menses were included. All the included subjects provided an informed consent. At the point of study entry, all study participants were subjected to clinical and biochemical investigations. Data were collected by trained interviewers. First of all, a questionnaire was completed at each Health Center by trained interviewers. Demographic information is achieved by a questionnaire. The exclusion criterion was the coexistence of any other serious illness.
Exclusion criteria included having hormone replacement therapy, taking drugs such as anti-diabetes and antihypertensive anti-lipidemic agents and smokers. A venous blood sample was collected from all the subjects who came after 8-12-hours in the morning after an overnight fast. The samples were centrifuged for 10 minutes at 3000 rpm. The serum was used for estimating fasting blood glucose, triglycerides, total cholesterol, LDL-cholesterol and HDL-cholesterol concentrations, by biochemical kit using spectrophotometer techniques (Model JENWAY 6105 UV / VIS) in the Biochemistry and Metabolic Disorders Research Center (Faculty of Medicine). 25- hydroxyvitamin D determined using enzyme immunoassay (EIA) kit with ELISA technique. 25-hydroxyvitamin D with <25nmol/L, 25-74nmol/L and >250nmol/L were classified as deficient, insufficient and sufficient, respectively. Postmenopausal women considered to have metabolic syndrome if they had any three or more of the following, according to the ATP III Criteria: [35]
A. Abdominal obesity: Waist Circumference >88 cm
B. Hypertriglyceridaemia: serum triglycerides level > 150 mg/dl
C. Low HDL-cholesterol: < 50 mg/dl
D. High blood pressure: SBP > 130 mmHg and/or DBP > 85 mmHg or on treatment for hypertension.
E. High fasting glucose: serum glucose level > 110 mg/dl or on treatment for diabetes.
Weight was then measured, while subjects were minimally clothed without shoes, using digital scales. Height was measured in standing position without shoes using tape meter while the shoulder was in a normal position. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Those with a BMI of 25.0-29.9 Kg/m2 were classified as overweight, whilst those with a BMI ≥30 Kg/m2 were defined as obese. Subjects with BMI greater than 45 Kg/m2 were considered very obese [36]. Waist circumference was measured at the point halfway between the lower border of ribs and the iliac crest in a horizontal plane [9], and hip circumference was measured at the widest level over the greater trochanters. Waist to hip ratio was calculated as waist circumference divided by Hip Circumference. Systolic and diastolic blood pressure was measured twice after 10-15 minutes resting in sitting position from the right hand. Two measurements were done from all postmenopausal women at five minutes intervals and we used the average of 2 measurements. The results were reported as percentages and mean ± SD. The statistical analysis was done with SPSS- 16 version software. The results were evaluated by using student\'t\' and Chi square test. Statistical significance was considered at P < 0.05.
Results
Table 1 shows that the mean body mass index, waist circumference, Hip, waist to hip ratio, diastolic blood pressure, triglyceride and fasting blood glucose levels were significantly higher in postmenopausal women with metabolic syndrome, but the mean HDL-cholesterol was lower (p< 0.05).There were no significant differences in the age, Years since post menopause, total cholesterol, systolic blood pressure, LDL-cholesterol and 25-hydroxy vitamin D of postmenopausal women with and without metabolic syndrome. Prevalence of the metabolic syndrome in postmenopausal women was 31%.
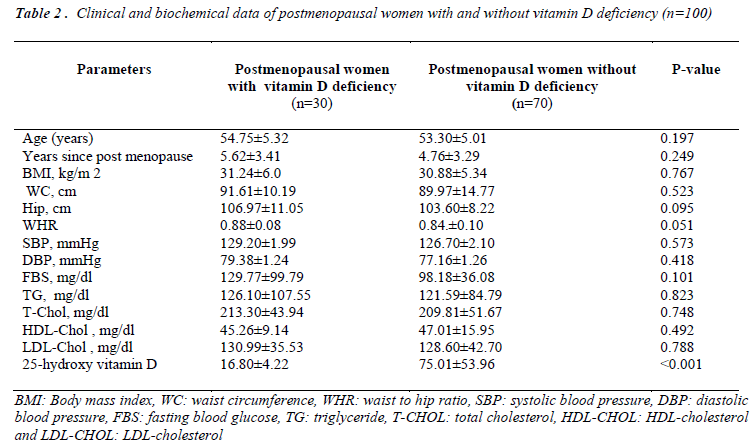
Table 2 shows the clinical and biochemical data of postmenopausal women with and without vitamin D deficiency. There were no significant differences between all parameters. There were significant differences in 25- hydroxy vitamin D of postmenopausal women with and without vitamin D deficiency. Prevalence of the vitamin D deficiency in postmenopausal women was 30%.
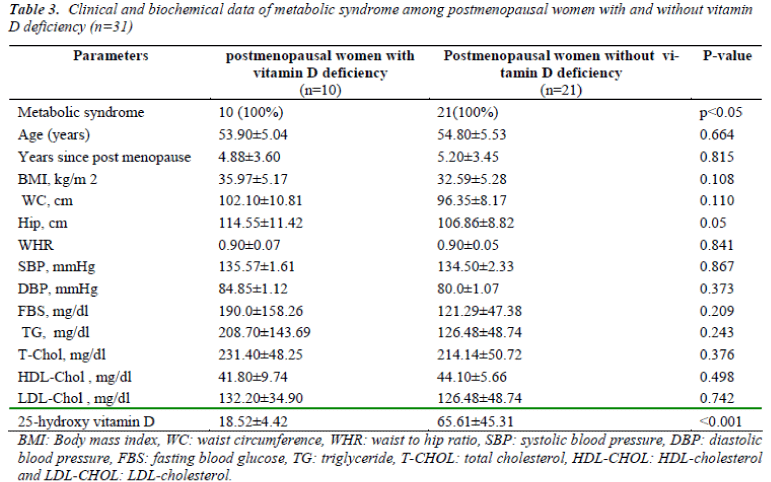
Table 3 shows the clinical and biochemical data of postmenopausal women with and without vitamin D deficiency who had metabolic syndrome. There were no significant differences between all parameters. There were significant differences in 25-hydroxy vitamin D of postmenopausal women with and without vitamin D deficiency who had metabolic syndrome. Prevalence of the vitamin D deficiency in postmenopausal women with metabolic syndrome was 32.26%.
Discussion
The prevalence of metabolic syndrome in postmenopausal women is 31%. Study on postmenopausal women in Austria showed that the prevalence of metabolic syndrome was 32.6% [20] which was similar to that in our finding. In an another study on postmenopausal women in Chengdu, China, showed that the prevalence of metabolic syndrome was 37.34%, which was higher than our finding [19] In our study, we showed the prevalence of the components of metabolic syndrome in postmenopausal women. Low HDL-cholesterol and high waist circumference were the most usual factors of metabolic abnormality in postmenopausal women. Prevalence of cardiovascular diseases might be increased. This may happen with high prevalence of metabolic syndrome in postmenopausal women. Study of Deibert et al [37] showed that prevalence of metabolic syndrome among post-menopausal women was 36.1% and also some other studies showed that menopausal women in Canada [38], Ecuador [27] and South Korea [39] had prevalence of metabolic syndrome 31%, 41.5% and 54.6% respectively. Our study shows that postmenopausal women were overweight and obese. Study of Lobo showed that weight increase and obesity greatly drive the elevated prevalence of metabolic syndrome in postmenopausal women. Changes in central obesity can cause metabolism abnormality and influence health [40]. Estrogen secretion decrease in postmenopausal women dependents on metabolic alterations and resulting agglomeration of abdominal fat. It is important to reduce the risk of cardiovascular disease in postmenopausal women. It suggests that postmenopausal women control blood glucose, blood pressure, lipid profile and change their life style to decrease extra weight increase by diet and sport [41]. Our findings show that there are no significant differences of vitamin D among postmenopausal women with and without metabolic syndrome. Some studies have shown that there is an association between vitamin D deficiency and the metabolic syndrome in the general population [9] and in women [30]. Our findings do not confirm these results in postmenopausal women. Some other studies show that there is no association between vitamin D deficiency and the metabolic syndrome in postmenopausal women [33,37,42].These findings are in agreement with our results. Despite vitamin D deficiency has been shown to influence nearly 40% of the general population [43]. In this study, we have shown a prevalence of vitamin D deficiency of 30% among postmenopausal women which is lower than the prevalence in the general population. The occurrence of vitamin D deficiency in postmenopausal women with metabolic syndrome was 32.26%. Our findings suggested that vitamin D deficiency was not common in postmenopausal women. The low prevalence of vitamin D deficiency in our study groups could be interpreted by environmental and genetic factors. It is possible that weather conditions changes could be responsible for the differences in the prevalence of vitamin D deficiency among different populations because of differences in sunlight exposure. Some studies have showed that vitamin D status is related to genetic variants of vitamin D metabolizing genes [44]. One explanation for low vitamin D deficiency among postmenopausal women perhaps associated with high sunlight exposure in this area. Another explanation for low vitamin D deficiency may be related to blood samples were drawn during the spring and summer. We also measured 25 (OH) vitamin D concentrations by ELISA which is different with other available methods. However, the links between metabolic syndrome and vitamin D are not exactly clear.
Conclusions
In summary, our results show that postmenopausal status might be a predictor of metabolic syndrome in this area.
Our findings also suggested that vitamin D levels have no association with metabolic syndrome. There were no significant differences in vitamin D levels in postmenopausal women with and without metabolic syndrome. Vitamin D deficiency is not associated with the metabolic syndrome.
Acknowledgement
The author would like to thank the personnel at the Biochemistry and Metabolic Research Center and different health centers of Golestan University of Medical Sciences for providing for their cooperation and assistance in the handling of experiments.
Competing interest
The authors have no conflicts of interest.
Funding
The study was funded by research deputy of Golestan University of Medical Sciences.
References
- Dobnig H, Pilz S, Scharnagl H, Renner W, Seelhorst U, Wellnitz B, et al. Independent association of low serum 25-hydroxyvitamin d and 1,25-dihydroxyvitamin d levels with all-cause and cardiovascular mortality. Arch Intern Med 2008; 168:1340–1349.
- Giovannucci E, Liu Y, Hollis BW, Rimm EB. 25-hydroxyvitamin D and risk of myocardial infarction in men: a prospective study. Arch Intern Med 2008; 168:1174–1180.
- Wang TJ, Pencina MJ, Booth SL,Wang TJPencina MJBooth SLJacques PF, Ingelsson E, Lanier K, et al. Vitamin D deficiency and risk of cardiovascular disease. Circulation 2008; 117:503–511.
- Knekt P, Laaksonen M, Mattila C, Härkänen T, Marniemi J, Heliövaara M, Rissanen H, et al. Serum vitamin D and subsequent occurrence of type 2 diabetes. Epidemiology 2008; 19:666–671.
- Cheng S, Massaro JM, Fox CS, Larson MG, Keyes MJ, McCabe, et al. Adiposity, cardiometabolic risk, and vitamin D status: the Framingham Heart Study. Diabetes 2010; 59: 242–248.
- Scragg R, Sowers M, Bell C. Serum 25-hydroxyvitamin D, diabetes, and ethnicity in the Third National Health and Nutrition Examination Survey. Diabetes Care 2004; 27:2813–2818.
- Karhapaa P, Pihlajamaki J, Porsti I, Kastarinen M, Mustonen J, Niemelä O. et al. Diverse associations of 25-hydroxyvitamin D and 1,25-dihydroxy-vitamin D with dyslipidaemias. J Intern Med 2010; 268:604–610.
- Martins D, Wolf M, Pan D, Zadshir A, Tareen N, Thadhani R, et al. Prevalence of cardiovascular risk factors and the serum levels of 25-hydroxyvitamin D in the United States: data from the Third National Health and Nutrition Examination Survey. Arch Intern Med 2007; 167:1159–1165.
- Ford ES, Ajani UA, McGuire LC, Liu S. Concentrations of serum vitamin D and the metabolic syndrome among U.S. adults. Diabetes Care 2005; 28:1228–1230
- Chiu KC, Chu A, Go VL, Saad MF: Hypovitaminosis D is associated with insulin resistance and beta cell dysfunction. Am J Clin Nutr 2004; 79:820–825.
- Boucher BJ: Inadequate vitamin D status: does it contribute to the disorders comprising syndrome ‘X’? Br J Nutr 1998; 79:315– 327.
- Pereira MA, Jacobs Jr DR, Van Horn L, Slattery ML, Kartashov AI, Ludwig DS. Dairy consumption, obesity, and the insulin resistance syndrome in young adults: the CARDIA Study. JAMA 2002; 287:2081–2089.
- Liu S, Song Y, Ford ES, Manson JE, Buring JE, Ridker PM. Dietary calcium, vitamin D, and the prevalence of metabolic syndrome in middle-aged and older US women. Diabetes Care 2005; 28: 2926–2932.
- Lloyd-Jones D, Adams R, Carnethon M, De SG, Ferguson TB, Flegal K, et al: Heart disease and stroke statistics-2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation 2009; vol.119, no.3, pp.480-486.
- Lerner DJ and Kannel WB. Patterns of coronary heart disease morbidity and mortality in the sexes: a 26-year follow-up of the Framingham population. Am Heart Journal 1986; 111: 383–390.
- Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the Third National Health and Nutrition Examination Survey. JAMA 2002; 3: 356-359.
- Rosamond W, Flegal K, Friday G, Furie K, Go A, Greenlund K, et al; American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics—2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee Circulation 2007; .5: e69-e171.
- Chedraui P, HidalgoL, Chavez D, Morocho N, Alavado M, Hu A. Quality of life among postmenopausal Ecuadorian women participating in a metabolic syndrome screening program. Maturitas 2007; 56: 45-53.
- Ding QF, Hayashi T, Zhang XJ, et al. Risks of CHD identified by different criteria of metabolic syndrome and related changes of adipocytokines in elderly postmenopausal women. J Diabetes Complications 2007; 21: 315-319.
- Ponholzer A, Temml C, Rauchenwald M, Marszalek M, Madersbacher S . Is the metabolic syndrome a risk factor for female sexual dysfunction in sexually active women? Int J Impot Research 2008; 20: 100-104.
- Rossi R, Nuzzo A, Oriqliani G, Modena MG.. Metabolic syndrome affects cardiovascular risk profile and response to treatment in hypertensive postmenopausal women. Hypertension 2008; 52: 865-872.
- Peters HW, Westendorp IC, Hak AE, Grobbee DE, Stehouwer CDA, Hofman A, et al. Menopausal status and risk factors for cardiovascular disease. J Intern Med 1999; 246: 521–528.
- Kannel WB, Hjortland MC, McNamara PM, Gordon T. Menopause and risk of cardiovascular disease: the Framingham study. Ann Intern Med 1976; 85: 447–452.
- Razay G, Heaton KW, Bolton CH. Coronary heart disease risk factors in relation to the menopause. Q J Med 1992; 85: 889– 896.
- Hjortland MC, McNamara PM, Kannel WB. Some atherogenic concomitants of menopause: the Framingham Study. Am J Epidemiol 1976; 103: 304–311.
- Royer M, Castelo-Branco C, Blumel JE, Chedraui PA, Danckers L, Bencosme A, et al: The US National Cholesterol Education Programme Adult Treatment Panel III (NCEP ATP III): prevalence of the metabolic syndrome in postmenopausal Latin American women. Climacteric 2007; 2: 164-170.
- Hidalgo LA, Chedraui PA, Morocho N, Alvarado M, Chavez D, Huc A. The metabolic syndrome among postmenopausal women in Ecuador. Gynecol Endocrinol 2006; 8: 447-454.
- Forouhi NG, Luan J, Cooper A, Boucher BJ, Wareham NJ. Baseline serum 25-hydroxy vitamin D is predictive of future glycemic status and insulin resistance: the Medical Research Council Ely Prospective Study 1990–2000. Diabetes 2008; 57: 2619–2625
- Hypponen E, Boucher BJ, Berry DJ, Power C. 25-hydroxyvitamin D, IGF-1, and metabolic syndrome at 45 years of age: a cross-sectional study in the 1958 British Birth Cohort. Diabetes 2008; 57:298–305.
- Reis JP, von Muhlen D, Miller ER 3rd: Relation of 25-hydroxyvitamin D and parathyroid hormone levels with metabolic syndrome among US adults. Eur J Endocrinol 2008;159: 41–48
- Botella-Carretero JI, Alvarez-Blasco F, Villafruela JJ, Balsa JA, Vazquez C, Escobar- Morreale HF. Vitamin D deficiency is associated with the metabolic syndrome in morbid obesity. Clin Nutr 2007; 26:573–580
- Hjelmesaeth J, Hofso D, Aasheim ET, Jenssen T, Moan J, Hager H, Roislien J, Bollerslev J. Parathyroid hormone, but not vitamin D, is associated with the metabolic syndrome in morbidly obese women and men: a cross-sectional study. Cardiovasc Diabetol 2009; 8:1-7.
- Awumey EM, Mitra DA, Hollis BW, Kumar R, Bell NH. Vitamin D metabolism is altered in Asian Indians in the southern United States: a clinical research center study. J Clin Endocrinol Metab 1998; 83: 169–173.
- Cornier MA, Dabelea D, Hernandez TL, Lindstrom RC, Steig AJ, Stob NR, Van Pelt RE, Wang H, Eckel RH. The metabolic syndrome. Endocr Rev 2008; 29:777–822
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults Adult Treatment Panel III). JAMA 2001; 285: 2486-2497.
- World Health Organization. Prevention and Management of the Global Epidemic of Obesity. Report of the WHO Consultation on Obesity. WHO: Geneva, 1998 (Technical Report Series, No. 894).
- Dalton M, Cameron AJ, Zimmet PZ, Shaw JE, Jolley D, DW Dunstan, TA Welborn; AusDiab Steering Committee. Waist circumference, waist-hip ratio and body mass index and their correlation with cardiovascular disease risk factors in Australian adults. J Intern Med 2003; 254: 555-563.
- Piché ME, Weisnagel SJ, Corneau L, Nadeau A, Bergeron J, Lemieux S. The WHO and NCEP/ATPIII definitions of the metabolic syndrome in postmenopausal women: are they so different? Metab Syndr Relat Disorder 2006; 1: 17-27.
- Kim HM, Park J, Ryu SY, Kim J. The effect of menopause on the metabolic syndrome among Korean women: the Korean National Health and Nutrition Examination Survey, 2001. Diabetes Care 2007; 3: 701-706.
- Lobo RA. Metabolic syndrome after menopause and the role of hormones. Maturitas 2008; 60: 10-18.
- Heidari R, Sadeghi M, Talaei M, Rabiei K, Mohammadifard N, Sarrafzadegan N. Metabolic syndrome in menopausal transition: Isfahan Healthy Heart Program, a population based study. Diabetology & Metabolic Syndrome 2010; 2: 59-64.
- Rueda S, Fernandez-Fernandez C, Romero F, Martinez de Osaba J, Vidal J, Vitamin D. PTH, and the metabolic syndrome in severely obese subjects. Obes Surg 2008;18:151–154.
- Malabanan A, Veronikis IE, Holick MF. Redefining vitamin D insufficiency. Lancet 1998; 351:805–806.
- Engelman CD, Fingerlin TE, Langefeld CD, Hicks PJ, Rich SS, Wagenknecht LE,et al. Genetic and environmental determinants of 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D levels in Hispanic and African Americans. J Clin Endocrinol Metab 2008; 93:3381–3388.