- Biomedical Research (2015) Volume 26, Issue 2
Serum levels of brain-derived neurotrophic factor and clinical efficacy of mirtazapine in geriatric patients with major depression.
Yuqi Zhang1, Changsong Zhang2†, Zaohuo Cheng1, Wenwei Xu1, Xiaowei Liu1, Qing Xu1, Ying Wang1, Guilin Li1, Yang Ling2, Jing Zhu2
1Wuxi Psychiatric Hospital, Nanjing Medical University, Wuxi, China
2Clinical Oncology Laboratory, Changzhou Cancer Hospital of Soochow University, Changzhou, China
- Corresponding Author:
- Changsong Zhang
Clinical Oncology Laboratory
Changzhou Cancer Hospital of Soochow University
No. 1 North Huaide Rd. Changzhou
213002 China
Accepted date: January 30 2015
Abstract
We investigated the clinical efficacy of mirtazapine in Chinese patients with major depressive disorder (MDD) and also examined mirtazapine's effects on the serum brain-derived neurotrophic factor (BDNF) levels in these patients. Fifty-eight geriatric patients with major depression were assigned to an 8-week treatment with either 15 to 45 mg/day of mirtazapine. The efficacy measurements were performed by the Clinical Global Impression rating scales (CGI). Serum BDNF levels were measured using enzyme-linked immunosorbent assay (ELISA). In the study, mean serum BDNF level of untreated depressed patients at baseline was 23.08 ± 11.25 ng/ml and the mean Hamilton Rating Scale for Depression (HRSD) score was 27.8 ± 5.4. After remission was achieved, the mean serum BDNF level was 37.15±20.48 ng/ml whereas the mean HRSD score was 9.6±4.1. After 8 weeks of treatment there was a statistically significant difference in the serum BDNF levels. Meanwhile, HRSD scores and CGI scores were decreased significantly after mirtazapine treatment. Whatever male or female patients, mirtazapine significantly improved serum BDNF levels and decreased the CGI and HRSD scores from baseline. The results showed serum BDNF levels may be considered as a marker of response to mirtazapine antidepressant treatment for Chinese geriatric patients with major depression. And mirtazapine has been an important option for the treatment of major depression in geriatric patients.
Keywords
Major depressive disorder; Mirtazapine; geriatric patients; brain-derived neurotrophic factor
Introduction
Depression is the third leading contributor to the global disease burden [1] . Clinical depression in the elderly is common and is also frequently confused with the effects of multiple illnesses and the medicines used to treat them. Depression within the geriatric patient is an important issue as it is associated with increased mortality. Such depression may have a different aetiology to that in younger patients and be associated with comorbid chronic physical health problems or cognitive impairment [2].
Mirtazapine is an atypical antidepressant, which is a noradrenergic and specific serotonergic antidepressant, and is thought to result from a combination of noradrenergic and serotonergic effects, with the latter specifically involving enhancement of serotonin 5-HT1 receptor-mediated effects [3]. Mirtazapine has predominantly been evaluated in the treatment of major depression and is approved in many counties for use in the treatment of major depression, which is effective and well tolerated for the treatment of patients with moderate to severe major depression [4]. Monotherapy with mirtazapine 15-45 mg/day leads to rapid and sustained improvements in depressive symptoms in patients with major depression, including the elderly. It is as effective as other antidepressants and may have a more rapid onset of action than selective serotonin reuptake inhibitors [3]. Limited evidence suggests that for certain elderly patients, mirtazapine may be preferable to sertraline for treatment of depression. It may also be more cost-effective in patients who have dementia. The choice is highly dependent upon individual comorbidities and subsequent polypharmacy [5].
A growing body of evidence shows that brain-derived neurotrophic factor (BDNF) plays a role in depressive disorder. BDNF is important for maintaining synaptic function and neural plasticity [6]. Study shows that treatment of depression improves serum BDNF level which may be considered as a nonspecific peripheral marker of depression [7]. These results support the hypothesis that BDNF might play a critical role in the pathophysiology of major depressive disorder and successful antidepressant treatment increases the attenuated BDNF levels in depressed patients [8, 9].
Few studies have reported BDNF serum levels in elderly depressed subjects and their relationship with antidepressant therapy. The aim of the study was to evaluate BDNF serum levels in elderly depressed patients before and after antidepressant treatment and to determine the relationship between the serum BDNF level and the response to mirtazapine in Chinese patients with major depressive disorder (MDD).
Methods
Subjects
The present study was conducted from 2010 to 2013. Fifty eight in- and outpatients with MDD were recruited from the Department of Geriatric Psychiatry, the Wuxi Psychiatric Hospital, Nanjing medical University in China. The patients (21 males, 37 females) were diagnosed according to the Diagnostic and Statistical Manual of Mental Disorders (fourth edition) criteria for MDD with the consensus of at least two experienced psychiatrists on the basis of an unstructured interview and a review of all medical records [10]. Depression severity was assessed according to the 21-item Hamilton Rating Scale for Depression (HRSD). Only subjects with a minimum HAMD score of 18 were enrolled in the study [11-13]. The Clinical Global Impression rating scales (CGI) are used to measures of symptom severity, treatment response and the efficacy of treatments in treatment studies of patients with MDD [14, 15].
Mirtazapine was taken once a day for 8 weeks. Mirtazapine was initiated at daily doses of 15 mg/day. After 1 week, the dose was flexibly altered by each doctor based on the patient’s systemic clinical conditions and side effects at each visit (weeks 1, 2, 4, 8). The doses of mirtazapine were gradually increased to maximums of 45 mg/day, depending on the patient’s condition. Of 58 patients, the number remaining in the study was 4 at week 1, 6 at week 2, and 18 at week 4; 30 patients completed 8 weeks of mirtazapine treatment.
Subjects with primary or comorbid diagnoses of schizophrenia, schizoaffective disorder, rapid cycling bipolar disorder, dementia, or alcohol or substance dependence, based on DSM-IV criteria, within the previous 6 months were excluded. We also excluded subjects who had a personal or family history of substance abuse/dependence or other major psychiatric disorders prior to the study. Patients taking medications were subjected to a 2-week washout period; patients taking psychotropic medications or other medications that might influence mirtazapine metabolism were subjected to an 8-week washout period. Demographic data were recorded, and patients with serious or unstable medical illnesses were excluded. All subjects were at least 18 years of age.
After written informed consent was obtained, venous blood was drawn from each subject. The trial was conducted in accordance with good clinical practices and the Helsinki Declaration. This study was approved by the ethics committees at Nanjing medical University.
Measurement of BDNF
Blood samples were collected before antidepressive treatment and after remission (decrease to 7 points or less on HRSD). They were kept at room temperature for 1 h followed by 1 h at 4 °C before serum was isolated. Samples were centrifuged at 4 °C (3000 rpm, for 15 min using a refrigerated centrifuge). Remove serum and assay immediately or aliquot and store samples at <= -20 °C. Avoid repeated freeze-thaw cycles. Serum BDNF levels were measured using enzyme-linked immunosorbent assay (ELISA) kits (Quantikine Human BDNF, R&D Systems, Minneapolis, MN, USA) according to the manufacturer's instructions. Each assay was performed in duplicate.
Statistical analysis
The Student’s t test was used to assess the significance of the change in psychopathology scores from baseline to endpoint in each treatment group. All tests were two tailed, and group differences were tested at the p < 0.05 level. All statistical analyses were performed using SPSS 18.0 (SPSS Inc., Chicago, IL, USA).
Results
The clinical efficacy of mirtazapine in geriatric patients with major depression
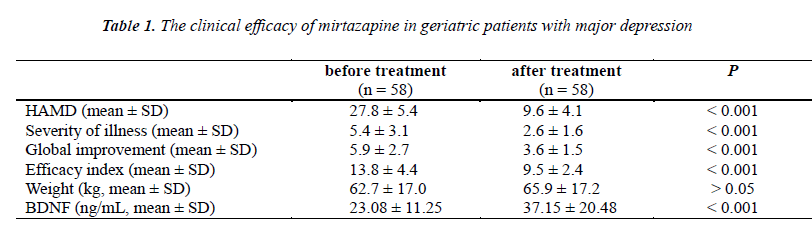
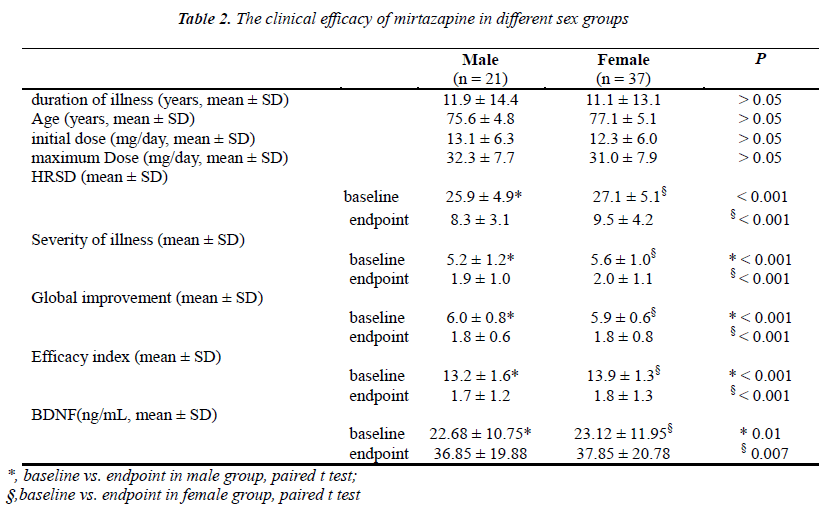
All patients were assessed with the Hamilton Rating Scale for Depression (HRSD) for depression severity after admission. Fifty-eight patients (age, from 60~88 years; Mean age: 76.8 ± 4.3 years) were recruited for inclusion in the trial. In the study, the mean HRSD score at the baseline before mirtazapine treatment was 27.8 ± 5.4, and the mean HRSD score after mirtazapine treatment was 9.6 ± 4.1 (Table 1). There were significant differences in the HRSD scores between the before and after mirtazapine treatment (p < 0.001). Meanwhile, we found that the decrease in HRSD scores were statistically significant in different sex groups from the baseline to the remission after 8 weeks treatment (male: p < 0.001; female: p < 0.001; respectively). Whatever male or female patients, mirtazapine significantly improved the HRSD scores from baseline (Table 2).
The clinical efficacy of mirtazapine was evaluated by the Clinical Global Impression Scale. The Severity of illness was decreased from 5.4 ± 3.1 at the baseline to 2.6 ± 1.6 after mirtazapine treatment (p < 0.001). The global improvement was decreased from 5.9 ± 2.7 at the baseline to 3.6 ± 1.5 after mirtazapine treatment (p < 0.001). The efficacy index was decreased from 13.8 ± 4.4 at the baseline to 9.5 ± 2.4 after mirtazapine treatment (p < 0.001). Meanwhile, we did not find any significant differences in weight gain between the before and after mirtazapine treatment (mean ± SD, 62.7 ± 17.0 kg and 65.9 ± 17.2 kg, respectively; p > 0.05). We also found that the decrease in CGI scores were statistically significant in different sex groups from the baseline to the remission after 8 weeks treatment (Table 2). Whatever male or female patients, mirtazapine significantly improved the CGI scores from baseline.
The effective of mirtazapine on serum BDNF level in geriatric patients with major depression
Blood samples were collected at the baseline and after 8 weeks of antidepressant treatment (during remission). The aim of the study was to evaluate BDNF serum levels in elderly depressed patients, before and after antidepressant treatment. In the study, we found that the mean serum BDNF level at the baseline before mirtazapine treatment was 23.08 ± 11.25 ng/ml, while the mean serum BDNF level after mirtazapine treatment was 37.15 ± 20.48 ng/ml (Table 1). After 8 weeks of treatment there was a statistically significant difference in the serum BDNF levels between the before and after mirtazapine treatment (p < 0.001). When we compared the serum BDNF level of the depressed patients from the baseline to the remission after 8 weeks treatment in different sex groups, there was no statistically significant difference (male: p = 0.01; female: p = 0.007; respectively). Whatever male or female, mirtazapine significantly improved the serum BDNF level from baseline in elderly Chinese patients with severe depression.
Discussion
Depression impacts older people differently than younger people. In the elderly, depression often occurs with other medical illnesses and disabilities and lasts longer. Mirtazapine is a commonly used antidepressant with a well-known ability to produce sedation [16]. Clarification of its efficacy as an augmentation therapy and in patients with refractory depression and its role in improving the efficacy and reducing the extrapyramidal effects of antipsychotic drugs would also help to establish its clinical value [4]. Low-dose mirtazapine as addon therapy has shown better efficacy, earlier onset of action and more number of responders and remitters as compared to conventional treatment in MDD in Indian patients [17]. Studies indicated that statistically significant and clinically relevant differences in favor of mirtazapine were evident on several outcome variables. Mirtazapine demonstrated an accelerated anxiolytic effect as shown by changes from baseline on the Hamilton Rating Scale for Anxiety [18].
In this study, the HRSD and CGI scores showed a significantly statistical difference between the before and after mirtazapine treatment both in male and female groups. Mirtazapine significantly improved the HRSD and CGI scores from baseline to the remission after 8 weeks mirtazapine treatment. The HRSD and CGI scores indicated that the patients showed a significant improvement of depressive symptoms, which is implied that mirtazapine was an effective treatment in elderly Chinese patients with severe depression.
BDNF, the most abundant of the neurotrophins in the brain, has been implicated in both major depression and cognitive function. Genetic association studies of the BDNF Val66Met polymorphism (rs6265) in geriatric depression have produced inconsistent results. Serum BDNF levels and BDNF Val66Met polymorphism are related to the mirtazapineresponse in MDD [19- 23]. Increasing evidence in the literature suggests a link between the brain-derived neurotrophic factor (BDNF) system and adult depression, supporting a role in the pathophysiology of the disease and response to therapy [24]. Clinical studies have indicated that serum or plasma BDNF levels are decreased in patients with untreated major depressive disorder (MDD), and that antidepressant treatment can restore the decreased BDNF level to the normal value [7, 25].
A few studies have reported BDNF serum levels in elderly depressed subjects and their relationship with antidepressant therapy. And low serum levels of BDNF are a state abnormality that is evident during depression and normalizes during remission [26]. BDNF had been a candidate molecule for influencing the clinical response to antidepressant treatment.
Conclusions
In this study, we found that the increase in serum BDNF level was statistically significant after 8 weeks of mirtazapine treatment. The results supported previous findings of low BDNF levels in untreated depressive patients compared to that those levels increase after antidepressant treatment. This study showed that mirtazapine treatment of depression improves serum BDNF level which may be considered as a marker of geriatric depression. This makes mirtazapine an important option for the treatment of major depression in geriatric patients who require additional therapy. Serum BDNF levels may be considered as a marker of response to antidepressant treatment for depression in the elderly. Further research is required to define the comparative efficacy of mirtazapine in the elderly with severe depression.
Abbreviations
DSM, The Diagnostic and Statistical Manual of Mental Disorders; MDD, major depressive disorders; BDNF, brain-derived neurotrophic factor; CGI, Clinical Global Impression rating scales; HRSD, Hamilton Rating Scale for Depression.
Competing interests
The authors declare that they have no competing interests.
Acknowledgements
This research was supported by the Science and Technology Planning Project of Wuxi Municipality, China (No. CSE01N1118); and The Medical Technology Project of Wuxi Hospital management center (No.YGZX1116); Jiangsu Provincial Special Program of Medical Science (BL2013012); the Health Talents Project for Jiangsu, China (LJ201157; RC2011038).
References
- Collins PY, Patel V, Joestl SS, March D, Insel TR, Daar AS, Scientific Advisory B, the Executive Committee of the Grand Challenges on Global Mental H, Anderson W, Dhansay MA, Phillips A, Shurin S, Walport M, Ewart W, Savill SJ, Bordin IA, Costello EJ, Durkin M, Fairburn C, Glass RI, Hall W, Huang Y, Hyman SE, Jamison K, Kaaya S, Kapur S, Kleinman A, Ogunniyi A, Otero-Ojeda A, Poo MM, Ravindranath V, Sahakian BJ, Saxena S, Singer PA, Stein DJ. Grand challenges in global mental health. Nature 2011; 475: 27-30.
- Downing LJ, Caprio TV, Lyness JM. Geriatric psychiatry review: differential diagnosis and treatment of the 3 D's - delirium, dementia, and depression. Curr Psychiatry Rep 2013; 15: 365.
- Croom KF, Perry CM, Plosker GL. Mirtazapine: a review of its use in major depression and other psychiatric disorders. CNS Drugs 2009; 23: 427-452.
- Holm KJ, Markham A. Mirtazapine: a review of its use in major depression. Drugs 1999; 57: 607-631.
- Holland J, Bhogle M. Sertraline and mirtazapine as geriatric antidepressants. Psychiatr Danub 2013;25 Suppl 2: S286-290.
- D'Sa C, Duman RS. Antidepressants and neuroplasticity. Bipolar Disord 2002; 4: 183-194.
- Aydemir O, Deveci A, Taneli F. The effe ct of chronic antidepressant treatment on serum brain-derived neurotrophic factor levels in depressed patients: a preliminary study. Prog Neuropsychopharmacol Biol Psychiatry 2005; 29: 261-265.
- Gonul AS, Akdeniz F, Taneli F, Donat O, Eker C, Vahip S. Effect of treatment on serum brain-derived neurotrophic factor levels in depressed patients. Eur Arch Psychiatry Clin Neurosci 2005; 255: 381-386.
- Martocchia A, Curto M, Scaccianoce S, Comite F, Xenos D, Nasca C, Falaschi GM, Ferracuti S, Girardi P, Nicoletti F, Falaschi P. Effects of escitalopram on serum BDNF levels in elderly patients with depression: a preliminary report. Aging Clin Exp Res 2014; 26:461-464.
- Spitzer RL, Wakefield JC. DSM-IV diagnostic criterion for clinical significance: does it help solve the false positives problem? Am J Psychiatry 1999; 156: 1856-1864.
- Leung CM, Wing YK, Kwong PK, Lo A, Shum K. Validation of the Chinese-Cantonese version of the hospital anxiety and depression scale and comparison with the Hamilton Rating Scale of Depression. Acta Psychiatr Scand 1999; 100: 456-461.
- Williams JB. A structured interview guide for the Hamilton Depression Rating Scale. Arch Gen Psychiatry 1988; 45: 742-747.
- Baca-Garcia E, Perez-Rodriguez MM, Basurte-Villamor I, Fernandez del Moral AL, Jimenez-Arriero MA, Gonzalez de Rivera JL, Saiz-Ruiz J, Oquendo MA. Diagnostic stability of psychiatric disorders in clinical practice. Br J Psychiatry 2007; 190: 210-216.
- Spearing MK, Post RM, Leverich GS, Brandt D, Nolen W. Modification of the Clinical Global Impressions (CGI) Scale for use in bipolar illness (BP): the CGI-BP.Psychiatry Res 1997;73:159-71.
- Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice.Psychiatry (Edgmont) 2007; 4: 28-37.
- Dolder CR, Nelson MH, Iler CA. The effects of mirtazapine on sleep in patients with major depressive disorder. Ann Clin Psychiatry 2012;24:215-24.
- Matreja PS, Badyal DK, Deswal RS, Sharma A. Efficacy and safety of add on low-dose mirtazapine in depression. Indian J Pharmacol 2012; 44: 173-177.
- Thompson C. Mirtazapine versus selective serotonin reuptake inhibitors. J Clin Psychiatry 1999;60 Suppl 17: 18-22; discussion 46-48.
- Hwang JP, Tsai SJ, Hong CJ, Yang CH, Lirng JF, Yang YM. The Val66Met polymorphism of the brain-derived neurotrophic-factor gene is associated with geriatric depression. Neurobiol Aging 2006; 27: 1834-1837.
- Katsuki A, Yoshimura R, Kishi T, Hori H, Umene-Nakano W, Ikenouchi-Sugita A, Hayashi K, Atake K, Iwata N, Nakamura J. Serum levels of brain-derived neurotrophic factor (BDNF), BDNF gene Val66Met polymorphism, or plasma catecholamine metabolites, and response to mirtazapine in Japanese patients with major depressive disorder (MDD). CNS Spectr 2012; 17: 155-163.
- Pei Y, Smith AK, Wang Y, Pan Y, Yang J, Chen Q, Pan W, Bao F, Zhao L, Tie C, Wang Y, Wang J, Zhen W, Zhou J, Ma X. The brain-derived neurotrophic-factor (BDNF) val66met polymorphism is associated with geriatric depression: a meta-analysis. Am J Med Genet B Neuropsychiatr Genet 2012;159B: 560-566.
- Erickson KI, Miller DL, Roecklein KA. The aging hippocampus: interactions between exercise,depression, and BDNF. Neuroscientist 2012; 18: 82-97.
- Kang RH, Chang HS, Wong ML, Choi MJ, Park JY, Lee HY, Jung IK, Joe SH, Kim L, Kim SH, Kim YK, Han CS, Ham BJ, Lee HJ, Ko YH, Lee MS, Lee MS. Brain-derived neurotrophic factor gene polymorphisms and mirtazapine responses in Koreans with major depression. J Psychopharmacol 2010; 24: 1755-1763.
- Ristevska-Dimitrovska G, Shishkov R, Gerazova VP, Vujovik V, Stefanovski B, Novotni A, Marinov P, Filov Different serum BDNF levels in depression: results from BDNF studies in FYR Macedonia and Bulgaria. Psychiatr Danub 2013; 25: 123-127.
- Lee BH, Kim YK. The roles of BDNF in the pathophysiology of major depression and in antidepressant treatment. Psychiatry Investig 2010; 7: 231-235.
- Chu CL, Liang CK, Chou MY, Lin YT, Pan CC, Lu T, Chen LK, Chow PC. Decreased plasma brain-derived neurotrophic factor levels in institutionalized elderly with depressive disorder. J Am Med Dir Assoc 2012; 13: 434-437.