Research Article - Biomedical Research (2017) Volume 28, Issue 22
Screening research for proper heparin concentration in patients with hypertension during continuous renal replacement therapy
Ming-chen Liu, Hui-ping Yao and Xiao-min Chen*
Department of Nursing, ICU, Zhejiang Provincial People's Hospital, People's Hospital of Hangzhou Medical College, Hangzhou, PR China
- *Corresponding Author:
- Xiao-min Chen
Department of Nursing, ICU
Zhejiang Provincial People's Hospital
People's Hospital of Hangzhou Medical College
PR China
Accepted date: October 03, 2017
Abstract
Heparin is the commonly anticoagulant used in Continuous Renal Replacement Therapy (CRRT). Thrombosis could reduce the efficacy of CRRT. Patients with hypertension who undertake CRRT increase the risk of thrombosis. The current study was to explore the proper concentration of heparin for patients with hypertension during CRRT. In our study, 225 patients without hypertension were control subjects (A group) and 225 patients with hypertension were enrolled (B group). According to Activated Partial Thromboplastin Time (APTT) before CRRT, the patients of A and B groups were divided into low risk-hemorrhage population (APTT<55 s) and high risk- hemorrhage population (APTT ≥ 55 s), respectively. After CRRT, the patients in low risk-hemorrhage population from A and B groups were subjected to 1000 IU/ml and 500 IU/ml heparin saline, respectively; while patients in high risk-hemorrhage population from A and B groups were given 500 IU/ml and 250 IU/ml, respectively. The double-lumen of dialysis catheters was used to carry out blood purification treatment and monitor the coagulation parameters including APTT, Prothrombin Time (PT) and International Normalized Ratio (INR). It was showed that 250 IU/ml of heparin was an appropriate concentration for sealing tube in all patients with APTT ≥ 55 s; 500 IU/ml heparin was an appropriate concentration for sealing tube in patients with hypertension (APTT<55 s).
Keywords
Heparin, Hypertension, Continuous renal replacement therapy (CRRT)
Introduction
In recent years, Continuous Renal Replacement Therapy (CRRT) has been applied extensively in multiple organ dysfunction syndrome [1]. Obstruction of vascular may seriously decline the efficacy of CRRT [2,3]. Therefore, blood purification treatment is crucial for maintaining the patency of vascular access [4]. Thrombosis is the most common complication of double-lumen catheters in hemodialysis [5]. The incidence rate of thrombosis caused by different concentration of sealing-up fluid was 2.6-35.5% [6]. Heparin saline is the most frequently used sealing-up fluid during CRRT. Heparin saline, as anticoagulant, is the useful agent to prevent thrombosis in catheter. But excessive concentration of heparin would lead to bleeding and coagulopathy; while inadequate concentration of heparin may result in thrombosis [7,8]. There is not yet a unitary standard for the concentration of heparin in China. 1000 IU/ml of heparin is considered a standard concentration, but it ignores the impact of coagulation factors on the patency of vascular access [9,10]. There are coagulation dysfunction and thrombopenia in critical patients under APTT above 55 s [11-13]. Obviously, single concentration of heparin cannot be applied uniformly to the patients with different physiological and pathological conditions.
About 10-49% patients received maintenance hemodialysis suffer from hypertension [14,15]. Patients with hypertension frequently are associated with the dysfunction of endogenous fibrinolysis and sympathetic hyperfunction, which increases the release of catecholamine and promotes platelet aggregation. This finally enhances the risk of thrombosis [16]. Therefore, reasonable selection of the heparin concentration is important for patients with hypertension after CRRT. In this study, we selected 225 cases of patients with normal blood pressure and 225 cases of patients with hypertension, which were further divided into low risk-hemorrhage population (APTT<55 s) and high risk- hemorrhage population (APTT ≥ 55 s), respectively. Different heparin concentration was used for closing the tube in each group after CRRT to formulate the proper concentration for patients with different coagulation function.
Patients and Methods
Patients
We enrolled 1015 cases of patients with CRRT and figured out 450 cases of patients who meet our research standard from May 2015 to May 2016 in Hospital. The patients’ age ranged between 20 and 96 y, with the mean ± SD age of 53.11 ± 18.96 y. All patients had signed a consent form and had not used any anticoagulant during the study period. 225 cases of patients with normal blood pressure were classified as control group (A group) and 225 cases of patients with hypertension as experimental group (B group). APTT<55 s was considered as the condition of low risk-hemorrhage and APTT ≥ 55 s was considered as the condition of high risk-hemorrhage. After CRRT, patients with APTT<55 s received 1000 IU/ml of heparin saline and patients with APTT ≥ 55 sec received 500 IU/ml of heparin saline to close catheter in A group, patients with APTT<55 s received 500 IU/ml of heparin saline and patients with APTT ≥ 55 s received 250 IU/ml of heparin saline to close catheter in B group.
Inclusion and exclusion criteria
Inclusion criteria for this study were as follows: patients with continuous blood purification therapy ≥ 2 in ICU; the temporary double-lumen of dialysis catheter was indwelt in patients; the sites of catheter were femoral vein; patients with hypertension did not have diabetes and pregnancy.
Exclusion criteria were as follows: patients were allergic to heparin; there were significant bleeding in patients; patients with APTT>120 s or blood platelet<30 × 109/l; patients with APTT<22 s; other complications in patients (in addition to hypertension).
Sealing method
The double-lumen of dialysis catheters (Bard International Ltd, USA) were used for carrying out blood purification treatment in all patients. The patients in A and B groups were divided into low risk-hemorrhage population (APTT<55 s) and high risk- hemorrhage population (APTT ≥ 55 s), respectively. Ten microliter of normal saline was used for washing residual blood in the end of artery and vein, the correspondent concentration of heparin was then used for positive pressure sealing by closing heparin cap. The catheter was proper fixation after sealing tube cavity and the covering catheter with sterile gauze.
Evaluation of specific indicators
Hemorrhage and catheter function were recorded after sealing for 1 and 4 h. Coagulation parameters including APTT, INR and PT were monitored before sealing tube and after sealing tube for 1 and 4 h. After eliminating the influence of catheter adherence and position, the blood velocity ≥ 200 ml was considered as catheter function well when the blood velocity ≥ 200 ml and heparin saline was withdrew into 20 ml of work drum in 6 s, the catheter function was considered to be normal; when the blood velocity<200 ml and heparin saline was painfully withdrew into 20 ml of work drum, the catheter function was considered to be obstructed partly; when heparin saline completely cannot withdrew into 20 ml of work drum, which was considered as catheter obstruction.
Statistical analyses
Data were analysed by SPSS version 21.0 (SPSS, Inc., Chicago, IL, USA). Descriptive data are presented as mean ± standard deviation. LSD t test or chi-square test was applied in intergroup comparison. Correlation analysis was analysed using person's method. P<0.05 was considered to be statistically significant.
Results
Comparison of gender, age and APTT in patients with or without hypertension
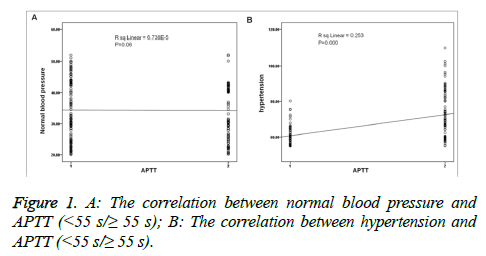
The age 450 patients varied from 20 to 96 y old. Patients without hypertension were A group; while patients with hypertension was B group. The average age of A group was 47.2 ± 19.3 and the average age of B group was 59.8 ± 20.5. There was no significant difference in sex between A and B groups (P>0.05; Table 1). The age had shown significant difference between A and B groups (P<0.05; Table 1). There were significant difference in APTT between A and B groups (P<0.05; Table 1). In addition, no significant differences were found between APTT and normal blood pressure in patients without hypertension (P>0.05; Figure 1A), however, there was significant difference in patients with hypertension (P<0.05; Figure 1B).
| A (225 cases) | B (225 cases) | p-value | ||
|---|---|---|---|---|
| Gender (male/female) | 110 /125 | 111/114 | >0.05 | |
| Age | 47.2 ± 19.3 | 59.8 ± 20.5 | <0.05 | |
| APTT | < 55 s | 152 | 125 | <0.05 |
| ≥ 55 s | 73 (32.4%) | 100 (44.4%) | ||
| Chi-square test, *P<0.05 | ||||
Table 1: The comparison of gender, age and APTT between A group and B group.
The effect of different concentration of heparin on coagulation function in patients with or without hypertension
The different concentration of heparin adopted in this study was based on our clinical experiences and some previous reports. In low risk-hemorrhage population (APTT<55 s) in A group (patients without hypertension) and B group (patients with hypertension), PT, INR and APTT subjected with 1000 IU/ml and 500 IU/ml for 1 h were both significantly increased compared with before sealing tube (P<0.05; Table 2). By contrast, after sealing tube for 4 h, PT, INR and APTT showed no significant differences compared with before sealing tube.
| APTT heparin | APTT<55 s (277 cases) | APTT ≥ 55 s (173 cases) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1000 IU/ml | 500 IU/ml | 500 IU/ml | |||||||||||
| Before | 1 h | 4 h | Before | 1 h | 4 h | Before | 1 h | 4 h | Before | 1 h | 4 h | ||
| A | PT (S) | 10.63 | 15.78 | 11.39 | 11.04 | 14.09 | 10.98 | 15.65 | 16.33 | 15.89 | 16.66 | 17.35 | 16.61 |
| INR | 1.02 | 1.12 | 1.06 | 1.07 | 1.11 | 1.05 | 0.98 | 0.99 | 1.02 | 1.11 | 1.13 | 1.1 | |
| APTT (S) | 25.12 | 50.32 | 30.21 | 26.33 | 45.32 | 27.59 | 69. 12 | 107.02 | 70.31 | 67.35 | 96.29 | 65.45 | |
| PT (S) | 11.32 | 12.65 | 11.66 | 10.98 | 11.94 | 11.01 | 16.32 | 17.25 | 17.02 | 16.02 | 17.02 | 16.23 | |
| B | INR | 1.13 | 1.19 | 1.08 | 1.1 | 1.02 | 0.99 | 1.04 | 1.01 | 1.02 | 1.01 | 1.13 | 1.03 |
| APTT (S) | 27.35 | 54.12 | 28.71 | 28.01 | 50.01 | 26.31 | 72.15 | 110.23 | 71.22 | 72.69 | 110.58 | 73.99 | |
Table 2: The general condition of patients with CRRT.
In high risk-hemorrhage population (APTT>55 s) in A group and B group, PT, INR and APTT subjected with 500 IU/ml and 250 IU/ml for 1 h were both increased compared with before sealing tube (P<0.05; Table 2). By contrast, after sealing tube for 4 h, PT, INR and APTT decreased to the level that showed before sealing tube. It was indicated that, no matter with or without hypertension, APTT had no significant influence on the concentration of heparin used in patients.
The different concentration of heparin had significant effect on bleeding of patients
As shown in Table 3, plugging ratio in all the groups was zero. For patients without hypertension, there was no significant difference between 1000 IU/ml and 500 IU/ml of heparin in low risk-hemorrhage population; nevertheless, the bleeding rate in 250 IU/ml heparin was significantly lower than that of 500 IU/ml of heparin in high risk-hemorrhage population (P<0.05). For patients with hypertension, the bleeding rate in 500 IU/ml of heparin was significantly lower than that in 1000 IU/ml when APTT was below 55 s; while there was significant difference in the bleeding rate between 250 IU/ml and 500 IU/ml heparin, when APTT was above 55 s (P<0.05).
| A (225 cases) | B (225 cases) | ||||||
|---|---|---|---|---|---|---|---|
| Blockage (Yes/No) | Bleed (Yes/No) | P-value | Blockage (Yes/No) | Bleed (Yes/No) | P-value | ||
| APTT<55 s | 1000IU/ml | 76/0 | 8/68 | >0.05 | 62/0 | 11/52 | <0.05 |
| 500 IU/ml | 76/0 | 4/72 | 63/0 | 3/60 | |||
| APTT ≥ 55 s | 500 IU/ml | 36/0 | 6/30 | <0.05 | 50/0 | 11/50 | <0.05 |
| 250 IU/ml | 37/0 | 1/36 (%) | 50/0 | 2/48 | |||
| Chi-square test, *P<0.05 | |||||||
Table 3: Comparison of blockage and bleed between APTT<55 s and APTT ≥ 55 s.
Discussion
In patients with hypertension, the activity of renin-angiotensin-aldosterone system is increased, which will enhance the platelet aggregation effects of paranephrine. The function of vascular endothelial cells is impaired and hypertrophic, resulting in an imbalance of secretion of fibrinolytic activity regulation factors. In addition, sympathetic function is hyperactive to promote platelet aggregation [17,18]. Therefore, balance between coagulation system, and fibrinolytic system is broken, causing the abnormality of blood coagulation mechanism (hypercoagulability) in patients with hypertension [19]. Blood hypercoagulability can increase the risk of thrombosis and bleeding. APTT presents the state of hypercoagulability [20]. According to the data in our clinical experiences, APTT<55 s was considered as low-risk hemorrhage and APTT ≥ 55 s was considered as high-risk hemorrhage.
Heparin, a highly sulfated proteoglycan, is widely used blood-thinner and has complex blood anticoagulant mechanism that affects multiple parts in coagulation process [21,22]. The effect of heparin is apparent within a short time, but eliminate quickly. The excessive concentration of heparin can result in bleeding [23,24]. By contrast, lower concentration of heparin can result in thrombosis [25]. In CRRT, 1000 IU/ml heparin was used as the standard concentration for tube-sealing to maintain the smooth of vascular access and prevent thrombosis. However, it was considered to effect bleeding rate of patients during CRRT. Therefore, it is not suitable to use the uniform standard heparin concentration to different patients.
In our study, there was no significant difference in gender and significant difference in age between patients without hypertension and patients with hypertension. It was showed that the elder patients were susceptible to hypertension. Significant differences were observed in APTT between A group and B group. In addition, the proportion of patients with APTT ≥ 55 s in B group was higher than that of A group. No significant statistical relationship was found between patient with normal blood pressure and APTT. However, hypertension had a significant positive correlation with APTT. These results showed that patients with hypertension were more likely to bleed than patients without hypertension.
Moreover, the results showed that APTT, INR and PT in A group and B group after sealing tube with 1000, 500 and 250 IU/ml heparin for 1 h, were significantly higher than that of before sealing tube; and after sealing tube for 4 h, APTT, INR and PT were reduced to the levels before sealing tube. It was showed that the concentration of heparin as tube-sealing solution had no effect on coagulation function over time. It might be associated with heparinization in blood purification treatment. In addition, without affecting catheter function, there was no significant difference in bleeding rate between 1000 IU/ml and 500 IU/ml heparin in A group under APTT below 55 s; however, 250 IU/ml of heparin in A group could significantly reduce bleeding rate compared to 500 IU/ml of heparin in A group under APTT above 55 s. For patients with hypertension, 500 IU/ml heparin could significantly reduce bleeding rate compared to 1000 IU/ml heparin (APTT<55 s); while 250 IU/ml heparin could significantly reduce bleeding rate compared to 500 IU/ml heparin (APTT>55 s). Based on the investigations, the risk of bleeding in patients with normal blood pressure was increased, when APTT ≥ 55 s. The risk of bleeding in patients with hypertension was higher than that with normal blood pressure. In addition, when APTT of patients with hypertension exceeded 55 s, the risk of bleeding was far more than of patients without hypertension and of the hypertension patients with APTT<55 s.
The major limitation of this study was the sample number was small. Another weakness was that the observation was local. Thus it may be interesting to undertake in-depth exploration from large sample trials.
Conclusion
In conclusion, the appropriate concentration of heparin tube-sealing solution is essential to improving the effect of CRRT, based on different patients: 250 IU/ml of heparin was an appropriate concentration for sealing tube in all patients with APTT ≥ 55 s; 500 IU/ml heparin was an appropriate concentration for sealing tube in patients with hypertension (APTT<55 s).
Acknowledgements
Supported by Medical Science and Technology Project A of Zhejiang Province at No. 2015KYA027, and also funded by scientific research item of Nursing Department of Zhejiang Provincial People's Hospital at No.2014-HLB-003.
References
- Walcher A, Faubel S, Keniston A, Dennen P. In critically ill patients requiring CRRT, AKI is associated with increased respiratory failure and death versus ESRD. Ren Fail 2011; 33: 935-942.
- Brain M, Winson E, Roodenburg O, McNeil J. Non anti-coagulant factors associated with filter life in continuous renal replacement therapy (CRRT): a systematic review and meta-analysis. BMC Nephrol 2017; 18: 69.
- Pistolesi V, Zeppilli L, Polistena F, Sacco MI, Pierucci A, Tritapepe L, Morabito S. Preventing continuous renal replacement therapy-induced hypophosphatemia: an extended clinical experience with a phosphate-containing solution in the setting of regional citrate anticoagulation. Blood Purif 2017; 44: 8-15.
- Villa G, Neri M, Bellomo R, Cerda J, De Gaudio AR, De Rosa S, Ronco C. Nomenclature for renal replacement therapy and blood purification techniques in critically ill patients: practical applications. Crit Care 2016; 20: 283.
- Ben AS, Hadj-Abdelkader M, Benezit M, Deteix P, Heng AE, Rosset E. Predictors of autogenous arteriovenous hemodialysis access thrombosis after renal transplantation. Ann Vasc Surg 2017.
- Dumantepe M, Uyar I. The effect of angiojet rheolytic thrombectomy in the endovascular treatment of lower extremity deep venous thrombosis. Phlebology 2017.
- Fernandez A, Nair V, McKeone A, Ho J. Pharmacological management of cerebral venous sinus thrombosis with full-dose IV heparin infusion and its clinical outcomes. Am J Emerg Med 2017.
- van Rein N, Biedermann JS, van der Meer FJM, Cannegieter SC, Wiersma N, Vermaas HW, Lijfering WM. Major bleeding risks of different low-molecular-meight-heparin agents: a cohort study in 12 934 patients treated for acute venous thrombosis. J Thromb Haemost 2017.
- Hughes SD, Bishop PD, Garcia R, Zhang T, Alexander WA. Topical recombinant thrombin at a concentration of 1000 IU/mL reliably shortens in vivo TTH and delivers durable hemostasis in the presence of heparin anticoagulation and clopidogrel platelet inhibition in a rabbit model of vascular bleeding. Ann Surg Innov Res 2009; 3: 14.
- Moran JE, Ash SR. Locking solutions for hemodialysis catheters; heparin and citrate-a position paper by ASDIN. Semin Dial 2008; 21: 490-492.
- Oudemans-van Straaten HM, Wester JP, de Pont AC, Schetz MR. Anticoagulation strategies in continuous renal replacement therapy: can the choice be evidence based? Intensive Care Med 2006; 32: 188-202.
- Tan HK, Baldwin I, Bellomo R. Continuous veno-venous hemofiltration without anticoagulation in high-risk patients. Intensive Care Med 2000; 26: 1652-1657.
- Tsuyama N, Ichiba T, Naito H. Unusual initial manifestation of acquired hemophilia a: a normal activated partial thromboplastin time, intramuscular hematoma and cerebral hemorrhage. Intern Med 2016; 55: 3347-3349.
- Hayati F, Beladi Mousavi SS, Mousavi Movahed SM, Mofrad Bushehri M. Pulmonary hypertension among patients undergoing hemodialysis. J Renal Inj Prev 2017; 6: 122-126.
- Zadeh SN, Hami M, Boostani R, Mojahedi MJ. Restless leg syndrome in chronic hemodialysis patients in Mashhad hemodialysis centers. J Renal Inj Prev 2017; 6: 137-141.
- Erlinger TP, Conlin PR, Macko RF, Bohannon AD, Miller ER, Moore TJ, Appel LJ. The impact of angiotensin II receptor blockade and the DASH diet on markers of endogenous fibrinolysis. J Hum Hypertens 2002; 16: 391-397.
- Dusing R. Pharmacological interventions into the renin-angiotensin system with ACE inhibitors and angiotensin II receptor antagonists: effects beyond blood pressure lowering. Ther Adv Cardiovasc Dis 2016; 10: 151-161.
- Lechin F, van der Dijs B, Hernandez G, Orozco B, Rodriguez S, Baez S. Acute effects of tianeptine on circulating neurotransmitters and cardiovascular parameters. Prog Neuropsychopharmacol Biol Psychiatry 2006; 30: 214-222.
- Kato F, Tanabe N, Ishida K, Suda R, Sekine A, Nishimura R, Tatsumi K. Coagulation-fibrinolysis system and postoperative outcomes of patients with chronic thromboembolic pulmonary hypertension. Circ J 2016; 80: 970-979.
- Du Z, Shi F, Liu D, Ye H, Surhio MM, Li J, Ye M. Anticoagulant activity of a sulfated Lachnum polysaccharide in mice with a state of hypercoagulability. Bioorg Med Chem Lett 2016; 26: 5550-5556.
- Maitz MF, Zitzmann J, Hanke J, Renneberg C, Tsurkan MV, Sperling C, Werner C. Adaptive release of heparin from anticoagulant hydrogels triggered by different blood coagulation factors. Biomaterials 2017; 135: 53-61.
- Zeng XJ, Peng H. Prevention of thromboembolic complications after spine surgery by the use of low-molecular-weight heparin. World Neurosurg 2017.
- Adatya S, Uriel N, Yarmohammadi H, Holley CT, Feng A, Roy SS, Zantek ND. Anti-factor Xa and activated partial thromboplastin time measurements for heparin monitoring in mechanical circulatory support. JACC Heart Fail 2015; 3: 314-322.
- Thomas CM, Zhang J, Lim TH, Scott-Douglas N, Hons RB, Hemmelgarn BR. Concentration of heparin-locking solution and risk of central venous hemodialysis catheter malfunction. Asaio J 2007; 53: 485-488.
- Li M, Wu H, Wang Y, Yin T, Gregersen H, Zhang X, Wang G. Immobilization of heparin/poly-l-lysine microspheres on medical grade high nitrogen nickel-free austenitic stainless steel surface to improve the biocompatibility and suppress thrombosis. Mater Sci Eng C Mater Biol Appl 2017; 73: 198-205.