Case Report - Ophthalmology Case Reports (2019) Volume 3, Issue 1
Scleromalacia perforans secondary to a pemphigus.
Sqalli Houssaini A*, Mansouri S, El Anzi O, Benzekri L, Senouci K, Hassam B
Department of Dermatology and Venereology, Hospital IBN SINA, Mohammed V University, Rabat, Morocco
- Corresponding Author:
- Sqalli Houssaini Asmaa
Dermatology and Venerology Department
University Hospital Center Ibn Sina Rabat, Morocco
Tel: +212661311366
E-mail: sqalli_asmae@hotmail.com
Accepted date: May 22, 2019
Citation: Sqalli Houssaini A, Mansouri S, El Anzi O, Benzekri L, Senouci K, et al. Scleromalacia perforans secondary to a pemphigus. Ophthalmol Case Rep. 2019;3(1):5-8.
DOI: 10.35841/ophthalmology.3.1.5-7
Visit for more related articles at Ophthalmology Case ReportsAbstract
Scleromalacia perforans is a rare form of anterior scleritis represented by progressive thinning of the sclera. It is most often associated with rheumatoid arthritis, and sometimes seen in inflammatory systemic disease. Rarely scleromalacia has been described in porphyria and herpes zoster. We are reporting the case of a 62-year-old man who was followed for Pemphigus vulgaris and who developed Scleromalacia perforans of the eye. the association between pemphigus and SP has never been described before. So this report suggests adding SP to rare but possible complications of pemphigus and highlights the importance of multi-disciplinary care.
Keywords
Scleromalacia perforans, Pemphigus, Ocular complications.
Introduction
Scleromalacia perforans (SP) is a rare form of anterior scleritis which readily presents as a blackish blue hue visible through a thin sclera [1]. No significant redness or pain is present but it is represented by progressive thinning of the sclera; It is a rare form of necrotizing anterior scleritis. It is often associated with systemic disease and involvement of multiple organs. We are reporting the case of a 62-year-old man who was followed for pemphigus vulgaris and who developed scleromalacia perforans of the eye.
This case is original because it is the first report of pemphigus patient who developed an SP.
Case Report
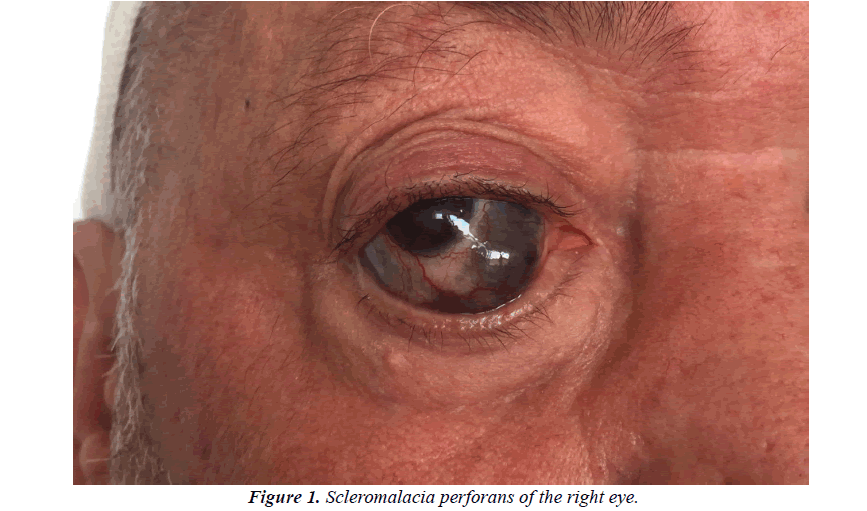
A 62-year-old hypertensive patient was followed in the dermatology department for a pemphigus vulgaris for 5 years treated with oral corticosteroid therapy with good initial development. The patient was lost from sight and then presented himself in a relapse chart of his pemphigus. On admission, the patient had diffuse cutaneous involvement with bullous lesions and post-bullous erosions. Otherwise, he reported a notion of eye pain with a decrease in the visual acuity of the right eye that had been evolving for 6 months. The examination objectified indeed a blue-blackish lesion of the right eye (Figure 1).
An ophthalmological examination was requested, showing the presence of a scleral thinning revealing the underlying uveal tissue, a protrusion of the eyeball and decreased visual acuity (6/10). A perforating scleromalacia was diagnosed. Therapy with prednisone at 1 mg/Kg/day and azathioprine 150 mg/J was started. The evolution was marked with the improvement of cutaneous lesions and persistence of SP.
Discussion
Pemphigus is an autoimmune disease affecting the skin and mucous membranes characterized by the presence of antibodies against intercellular substance, which leads to suprabasal acantholysis and therefore blisters formation.
Ocular involvement can rarely be seen. It may be unilateral or bilateral and usually presents as chronic and refractory blepharitis and conjunctivitis [2,3]. Conjunctival bullas are unusual, [4,5] and sometimes, erosions and blisters over the lid margin and mucous discharge may be observed [6,7].
Persistent inflammation and erosion of the eyelids may affect the anatomy of the lid margin and the quality of the tear film and cause severe dryness, leading to poor vision quality. Atypical features are also reported, including cicatricial changes on both bulbar and tarsal conjunctivae [8], cobblestone-like conjunctival papillae [9], and trichiasis resembling mucous membrane pemphigoid [10]. No case of Scleromalacia perforans has been reported. Scleromalacia perforans is a rare severe disorder of the globe. It is a necrotizing scleritis without inflammation. Thinning and atrophy of the episclera are progressive without inflammatory signs, with the development of localized areas of scleral infarction. It is characterized by insidious and slow progression until changes of color sclera appear which corresponds to the choroid that appears through transparency through thin conjunctiva.
SP usually occurs in rheumatoid arthritis and more rarely during some vasculitis, systemic lupus erythematosus, Behçet disease, Wegener’s granulomatosis, it is also described in Crohn disease, porphyria, ankylosing spondylitis, and herpes zoster.
Young and Watson suggest three main causes leading to scleral destruction: prolonged local vasoconstriction, activation of scleral fibrocytes with resorption of the extracellular matrix, and infiltration of the scleral stroma by inflammatory cells, which explains the frequent occurrence of SP during inflammatory diseases [11]. The main complications are cataracts, anterior uveitis, glaucoma, and visual loss. Our patient had decreased visual acuity (6/10).
There is no therapeutic consensus. Treatment relies on corticosteroids and immunosuppressive drugs for severe necrotizing scleritis [12]. Surgical treatment is indicated in necrotizing scleritis with perforation of the globe. Surgery of SP is also needed when the uvea is exposed to preserve the integrity of the globe [11,13].
It is also necessary to treat or control the underlying pathology that led to SP to prevent recurrences [14]. For our case, the treatment of pemphigus allowed a stabilization of the ocular lesions.
There are Some reports describing the effectiveness of infliximab in the treatment of scleritis in case of failure of immunosuppression [15,16]. Otherwise, Lola E et al. reported the successful treatment of two cases of refractory necrotizing scleritis with adalimumab [17].
As it is the first report of pemphigus patient who developed an SP, this report suggests adding SP to rare but possible complications of pemphigus.
Conclusion
In conclusion, despite the rarity of ocular involvement during pemphigus, it must always be sought in order to provide adequate care early and avoid complications. SP should be added to possible manifestations of pemphigus vulgaris.
Finally, autoimmune bullous diseases, especially pemphigus vulgaris, are serious pathologies with various complications and often require multidisciplinary management with the collaboration of dermatologists, ophthalmologists, and internists to provide optimal patient care.
References
- Tong L, Thumboo J, Tan YK, et al. The eye: A window of opportunity in rheumatoid arthritis? Nat Rev Rheumatol. 2014;10(9):552-60.
- Daoud YJ, Cervantes R, Foster CS, et al. Ocular pemphigus. J Am Acad Dermatol. 2005;53(4):585-90.
- Hodak E, Kremer I, David M, et al. Conjunctival involvement in pemphigus vulgaris: A clinical, histopathological and immunofluorescence study. Br J Dermatol. 1990;123(5):615-20.
- Palleschi GM, Giomi B, Fabbri P. Ocular involvement in pemphigus. Am J Ophthalmol. 2007;144(1):149-52.
- Fiore JM, Perry HD, Donnenfeld ED, et al. Pemphigus vulgaris: Bilateral plica semilunaris involvement. Cornea. 2011;30(3):357-59.
- Camisa C, Meisler DM. Immunobullous diseases with ocular involvement. Dermatol Clin. 1992;10(3):555-70.
- Lifshitz T, Levy J, Cagnano E, et al. Severe conjunctival and eyelid involvement in pemphigus vulgaris. Int Ophthalmol. 2004;25(2):73-4.
- Baykal HE, Pleyer U, Sonnichsen K, et al. Severe eye involvement in pemphigus vulgaris (in German). Ophthalmologe. 1995;92(6):854-57.
- Chirinos-Saldana P, Zuniga-Gonzalez I, Hernandez-Camarena JC, et al. Cicatricial changes in ocular pemphigus. Eye (Lond). 2014;28(4):459-65.
- Namba H, Narumi M, Sugano A, et al. Pathological findings of pemphigus vulgaris showing giant cobblestone-like conjunctival papillae. Case Rep Ophthalmol. 2013;4(3):114-21.
- Murphy CC, Ayliffe WE, Booth A, et al. Tumor necrosis factor blockade with infliximab for refractory uveitis and scleritis. Ophthalmology. 2004;111(2):352-56
- Suami M, Kato M, Koide K, et al. Keratolysis in a patient with pemphigus vulgaris. Br J Ophthalmol. 2001;85(10):1263-64.
- Kopacz D, Maciejewicz P, Kopacz M. Scleromalacia perforans-what we know and what we can do. J Clinic Experiment Ophthalmol. 2013;S2:009.
- Pavesio CE, Meier FM. Systemic disorders associated with episcleritis and scleritis. Curr Opin Ophthalmol. 2001;12(6):471-78.
- O?Day DM, Horn JD. The eye and rheumatic disease. In: Ruddy S, Harris ED, Sledge CB, eds. Kelley?s Textbook of rheumatology. Philadelphia: Saunders, 2001:393-400.
- Nguyen QD. Scleral patch graft in the management of necrotizing scleritis. Int Ophthalmol Clin. 1999;39(1):109-31.
- Lola E, Lawuyi, Gurbaxani A. Refractory necrotizing scleritis succesfully treated with adalimumab. J Ophthalmic Inflamm Infect.2016;6:37