Research Paper - Archives of General Internal Medicine (2018) Volume 2, Issue 3
Role of Common Environmental Surfaces in the School in Transmission Enteric Bacterial Pathogens.
Abdulrahim M Alkhamis1* and Mohamed Noweir2
1Department of Public Health, Ministry of Health, Saudi Arabia
2Faculty of Medicine, Alexandria University, Egypt
- *Corresponding Author:
- Abdulrahim M Alkhamis
Department of Public health
Ministry of Health, Saudi Arabia
E-mail: rahim14moh@gmail.com
Accepted on June 11, 2018
Citation: Alkhamis AM, Noweir M. Role of common environmental surfaces in the school in transmission enteric bacterial pathogens. Arch Gen Intern Med. 2018;2(3):36-41. DOI: 10.4066/2591-7951.1000056
DOI: 10.4066/2591-7951.1000056
Visit for more related articles at Archives of General Internal MedicineAbstract
Inanimate surfaces play a role in the transmission of human pathogens, e.g. (fecal coliform) either direct or indirect. Toilets surfaces are a potential source of finding many bacterial due to different factors that help pathogens to grow and transmission. The related of transmission of enteric pathogenic microorganisms via the hands of the toilet visitors thus continues to be a problem in the community.
Aim: To assess the role of environmental surfaces at schools, to transmission enteric bacterial pathogens.
Methods: The exposure area microbiological cotton swabs were collected from 16 selected schools in Dammam town from government schools and rented schools, twice per week and transferred to the microbiology laboratory at the University of Dammam to process within 2 hours for fecal coliforms.
Results: Among 592 (100%) microbiology swab samples of the selected command from selected commonly touched environmental surfaces only 15 (2.5%) showed positive for fecal coliforms with the highest isolation frequency from toilet washer 11 (14.9%) of the 15 total positive samples followed by sink wall 3 (4%) and finally the class door handle 1 (1.4%) of the 15 total positive samples.
Conclusions: The highest positive results were in governmental school’s surface; lowest positive results were in rented schools surface. However, Hand-washing, a simple and effective way to cut down on cross-contamination is all too often forgotten.
Keywords
School, Pathogen, Transmission, Contact, Direct.
Introduction
The role of the environmental surface in the transmission of the disease has questioned. Recently, there are many reports of life-threatening due to community-acquired infections and that emphasize to be more investigation and identify community surface that potential career bacteria [1]. Inanimate surfaces have been shown to play a role in the transmission of human pathogens either directly, by surface-to-mouth contact, or indirectly, by contamination of fingers and subsequent hand-to- mouth contact [1]. Gastrointestinal diseases continue to be a significant health problem in school-age worldwide.
Diarrhea is the second leading cause of death among children under five globally. Nearly one in five child deaths- about 1.5 million each year is due to diarrhea [2]. In 2004, there were 36.4 million children of elementary school age (5-13 years) in the United States. Of these children, 31.1 million enrolled in elementary school [2]. Children in this age group are at risk of developing respiratory and gastrointestinal infections, most commonly caused by the exchange of secretions and inadequate hand hygiene [3]. School-aged children are often absent because of these common infectious diseases [3]. These absences also result in lost time from work for parents and substantial costs related to physician visits and antibiotic prescriptions [3].
Direct contact transmission requires physical contact between an infected person and a susceptible person and the physical transfer of microorganisms. Direct contact includes touching an infected individual [4].
There are many area highly potential source of infection and one of them toilets due to contaminated with microbes from the gut most of the time [5]. In this case, the organism was found under the flushing rim and in the scale on the porcelain surface of the toilet). The risks from the toilet assessed as follows: In general, the risk from the toilet bowl itself is not high, because flushing removes the bacteria.
Indeed, concerning the pathogenic profile that could be expected to isolate due to fecal contamination of environmental surfaces, it is not possible to test collected samples for every pathogen, and detection techniques are often expensive as well as time-consuming. For this reason, indicator organisms are used to test for the potential contamination by enteric pathogens. Indicator organisms were chosen according to specific requirements, some of which are:
The indicator must be present when the pathogen is present. The indicator must be as resistant to the environmental conditions, water purification, and disinfection processes as the pathogen.
The indicator must be detectable by relatively simple, rapid laboratory techniques [6]. Fecal coliforms occur in large numbers in human feces and can presumptively identify on differential culture media. Each discrete colony represents a bacterial cell initially present on the surface that sampled. In principle, the number of fecal coliforms rather than the frequency of positive samples reported in previous school’s studies should more accurately reflect enteropathogenic characteristics of infectious dose and survival in the environment. Indeed, Limited studies concerning the pattern and epidemiology of diarrheal diseases among school-age children in Saudi Arabia are available.
Many studies in this field during last years have focused on hospitals, daycare facilities, and schools, but little attention paid to the home. Recent events, including widespread. Media coverage of foodborne outbreaks and increased marketing of a variety of antibacterial products for personal hygiene and hard surface disinfection have resulted in a resurgence of interest and public concern about hygiene and cleanliness in the home [1]. Hygiene refers to conditions or practices by which people maintain or promote health by keeping them and their surroundings clean. The question that persists is: How do household cleanliness and personal hygiene affect the risk of infectious disease transmission? [7].
There are suvere of study have proved that domestic toilets career and spread of Salmonella bacteria and causes salmonellosis [8]. Campylobacteriosis, like many gastrointestinal human diseases, has its ecology in which the propagation of human infection and disease depends on pathogen survival and finding new hosts to replicate and sustain the pathogen population. The pathogen survival trajectories that lead to human exposure include ecologic filters that limit population size, e.g., cooking food to kill Campylobacter. Environmental factors that influence the size of the pathogen reservoirs include temperature, nutrient availability, and moisture availability during the period the pathogen population is moving through the environment between infected and susceptible hosts [9].
Previously, it demonstrated that children in educational facilities commonly experience diarrhea due to rotavirus, Giardia, and bacterial pathogens. Multiple agents frequently coexist, and the environment heavily contaminated with enteric bacteria during outbreaks [10].
Bright et al. reported the presence of microorganisms on common classroom contact surfaces (e.g., fomites) was determined to identify the area’s most likely to become contaminated. Six elementary classrooms were divided into control and intervention groups (cleaned daily with a quaternary ammonium wipe) and tested for heterotrophic bacteria. Three classrooms were also tested for norovirus and influenza A virus. Frequently used fomites were the most contaminated; water fountain toggles, pencil sharpeners, keyboards, and faucet handles were the most bacterially contaminated; desktops, faucet handles, and paper towel dispensers were the most contaminated with viruses. Influenza A virus was detected in up to 50% and norovirus on up to 22% of surfaces throughout the day. Children in the control classrooms were 2.32 times more likely to report absenteeism due to illness than children in the intervention classrooms and were absent longer (on average).
Improved classroom hygiene reduced the incidence of infection and thus student absenteeism [11].
On the other’s hand, Ross-Degnan et al. reported that Good hand hygiene might reduce the spread of infections in families with children who are in out-of-home child care. Alcohol-based hand sanitizers rapidly kill viruses that commonly associated with respiratory and Gastrointestinal (GI) Infections [12].
The study showed clear evidence of 54% decrease in microbial flora after hand washing. Thus, it can conclude that hand washing is a cornerstone to prevent the diarrhoeal infection. Infectious diseases that are commonly spread through hand to hand contact include common cold and several gastrointestinal disorders, such as diarrhea. School going children exposed to higher risks of diarrhoeal disease by consuming contaminated water and food. If proper treatment not given, this can prove fatal, particularly to children. Many of these illnesses occur unnecessarily since the fecal-oral routes of disease transmission are easily prevented. The students in schools or colleges are more likely to take meal and water without washing hands and may pose the risk of infection. Hygiene has a measurable impact on reducing the burden of infections in the developing world. One of the best way and easier to stopping transmission of pathogens by hand hygiene [13].
Gastrointestinal diseases continue to be a significant health problem in primary schools in the UK. Kaltenthaler et al. in Their study, which took place in 20 primary schools in the Leeds area, investigated the presence of fecal indicator bacteria on children's hands and environmental surfaces. Fecal streptococci used as an indicator of fecal contamination. A handwashing knowledge score developed for each child. Those children with good hygiene knowledge had less fecal contamination on their hands (relative risk: 1.4, 95% CI=1.09-1.81, P=0.005). Those schools with higher hand counts were more likely to have had a reported outbreak of gastroenteritis in the past. Of the swabs taken from surfaces in the toilet areas and classrooms, the carpets in the classrooms were the most frequently contaminated surfaces [2].
In Saudi Arabia Al-Freihi et al. in 1993 conducted a prospective study of acute diarrheal diseases in the Eastern Province of Saudi Arabia over a 19-month period to determine etiology, risk factors, and other epidemiological characteristics. Of the 853 subjects studied, 344 were cases and 509 controls. More cases are seen in children than in adults. Enteric pathogens detected in 49% of the cases, but none in the controls. Of the pathogens, 68% were bacterial with Salmonella (34%) and Shigella species (14.7%) being the most common; Campylobacter jejuni emerged as an essential cause especially in adults. Contrary to most reports, rotaviruses were responsible for only 11.5% of the cases in children. Entamoeba histolytica (13.5%) and Giardia intestinalis (10.4%) were parasites commonly detected. Shigella organisms were the only pathogens that isolated in hospital cases without being isolated in cases from the community [8].
Materials and Methods
The study conducted in a randomly selected 16 primary schools in Dammam city- Eastern province Saudi Arabia and the sampling sites was commonly touched surfaces swabbed during the school visits including; toilet`s tap, toilets washer, washing sinks and door handle in the bathroom and Classrooms from inside). The frequency of samples was collected from each sampling site once.
Equipment used for testing the samples was; icebox, sterile disposable cotton swabs, sterile 10 ml screw capped centrifuge tubes containing 1 ml buffered peptone broth, standard count agar plates, centrifuge, sterile 10 ml screw capped centrifuge tubes containing single strength lauryl tryptose broth (LTB) and inverted Durham's tube, sterile 10 ml screw capped centrifuge tubes containing single strength Brilliant Green Lactose Bile broth (BGLBB) and inverted Durham's tube, flam source, humidity meter, and incubator.
On the first day was measured humidity and temperature by using digital parameter. Than samples were collection from each school's toilets tap, toilets lock, toilets washer, toilets siphon, sink tap, bath handle and class door handle from inside were swabbed using the cotton swabs. After that, the tubes were labeled and stored in the ice pox to be transferred to the microbiology laboratory at Imam Abdulrahman Bin Faisal university within 2 hours. In the Laboratory the sterile 10 ml screw capped centrifuge tubes containing single strength lauryl tryptose broth, and inverted Durham's tube was inoculated aseptically by the swabs then incubated at 37°C for 24 hours. The swabs were then returned to the tubes again, and then they centrifuged at 1000 rpm for 3 minutes. Then 1 ml of the homogenate was transferred to a Hetero Trophic standard agar Plate (HPC) to estimate the total viable count by pour plate method (Heterotrophic plate count (Standard plated method)) and plates incubated at 37°C for 24 hours. On the second day, was procedure each tube of lauryl tryptose broth observed for the presence of turbidity and gas production, negative tubes reintubated for another 24 h. Using a flame sterilized loop, transfer two loopful from each positive lauryl tryptose broth tube to a BGLBB tube in duplicate than tubes incubated at 35-37°C and for 44 ± 0.5°C 48 hrs. After 24 hours the tubes were checked for gas formation. The tubes incubated at 37°C: if showed turbidity and gas were considered positive for Total Coliforms, and if negative it was reintubated at 37°C for more 24 hours. Tubes incubated at 44 ± 0.5°C: if showed turbidity and gas were considered positive for fecal Coliforms, and if negative it was reintubated at 37°C for more 24 hours. HPC plate count: Using the Quebec colony counter, all plates showed growth were counted and scored as follow; 0-30 colonies considered Negative and 30-300 colonies considered contamination [14]. All data were submitted to statistical analysis using SPSS system.
Results
Table 1 showed that Among 592 (100%) microbiology swab samples of the selected command from selected commonly touched environmental surfaces only 15 (2.5%) showed positive for fecal coliforms with the highest isolation frequency from toilet washer 11 (14.9%) of the 15 total positive samples followed by sink wall 3 (4%) and finally the class door handle 1 (1.4%) of the 15 total positive samples.
| toilet tap | toilet lock | toilet washer | toilet siphon | sink wall | sink tap | bath handle | class door handle | Total | |
|---|---|---|---|---|---|---|---|---|---|
| positive | 0 0% |
0 0% |
11 14.9% |
0 0% |
3 4.1% |
0 0% |
0 0% |
1 1.4% |
15 2.5% |
| negative | 74 100% |
74 100% |
63 85.1% |
74 100% |
95.9 95.9% |
74 100% |
74 100% |
73 98.6% |
577 97.5% |
| Total | 74 | 74 | 74 | 74 | 74 | 74 | 74 | 74 | 592 |
Table 1. Comparison of the percentage of isolation frequency of fecal Coliforms from the school`s selected commonly touched environmental surfaces.
The result from the Table 2 showed that among the swabbed selected commonly touched different environmental surfaces the highest HPC results were obtained from toilet washer handle as the Mean ± SD was (21.43 ± 68.01) followed by sink wall samples HPC Mean ± SD was (1.43 ± 7.12) then class door handle HPC Mean ± SD (.26 ± 2.21) while the other surfaces showed negative result.
| toilet tap | toilet lock | toilet washer | toilet siphon | sink wall | sink tap | bath handle | class door handle | |
|---|---|---|---|---|---|---|---|---|
| Mean | .00 | .00 | 21.43 | .00 | 1.43 | .00 | .00 | .26 |
| Std. Deviation | .00 | .00 | 68.01 | .00 | 7.12 | .00 | .00 | 2.21 |
Table 2. Comparison Between the means of heterotrophic Plate Count results from the school`s selected commonly touched different environmental surfaces.
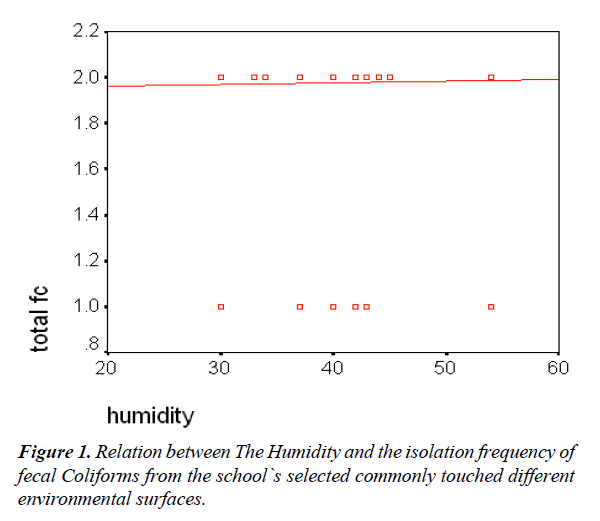
Table 3 and Figure 1 showed a weak positive correlation between Humidity and number of positive fecal Coliforms swabs among the swabbed commonly touched different environmental surfaces.
| Total FC | Humidity | Correlation | significance | |
|---|---|---|---|---|
| Mean ± SD | 1.97 ± 0.15 | 39.7 ± 5.99 | 0.026 | 0.52 |
Table 3. Relation between The Humidity and the isolation frequency of fecal Coliforms from the school`s selected commonly touched different environmental surfaces. Mean 2=negative; 1=positive.
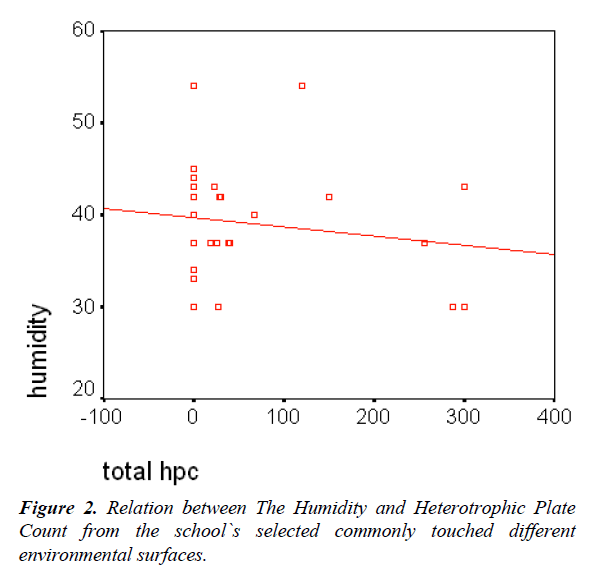
Table 4 and Figure 2 showed a negative correlation between Humidity and Heterotrophic Plate Count among the swabbed commonly touched different environmental surfaces in the selected schools.
| Total HPC | Humidity | Correlation | significance | |
|---|---|---|---|---|
| Mean ± SD | 2.89 ± 25.05 | 39.7 ± 5.99 | -0.041 | 0.308 |
Table 4. Relation between The Humidity and Heterotrophic Plate Count from the school`s selected commonly touched different environmental surfaces.
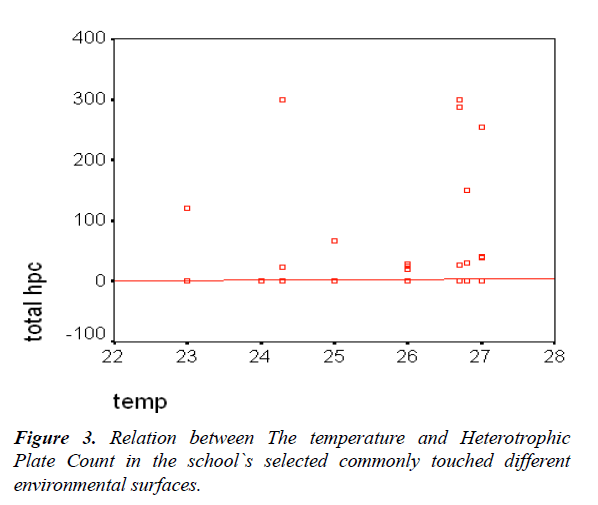
Table 5 and Figure 3 showed a weak positive correlation between temperature and Heterotrophic Plate Count among the swabbed commonly touched different environmental surfaces.
| Total HPC | Temperature | Correlation | significance | |
|---|---|---|---|---|
| Mean ± SD | 2.89 ± 25.05 | 25.77 ± 1.19 | 0.017 | 0.662 |
Table 5. Relation between the temperature and Heterotrophic Plate Count in the school`s selected commonly touched different environmental surfaces.
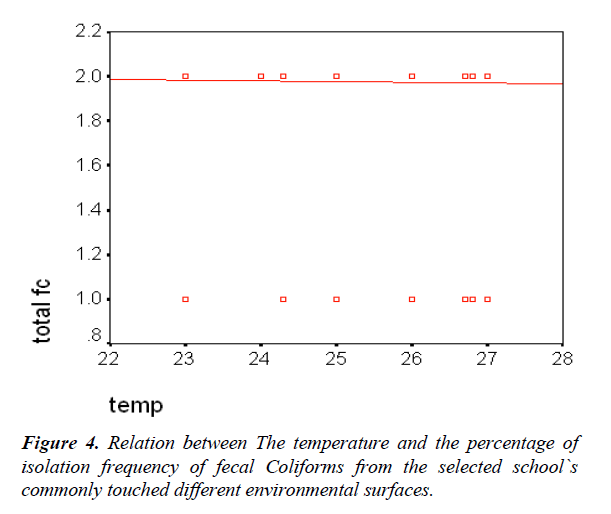
Table 6 and Figure 4 showed a negative correlation between temperature and percentage of isolation frequency fecal Coliforms among the swabbed commonly touched different environmental surfaces.
| Total FC | Temperature | Correlation | significance | |
|---|---|---|---|---|
| Mean ± SD | 1.97 ± 0.15 | 25.77 ± 1.19 | -0.024 | 0.556 |
Table 6. Relation between the temperature and the percentage of isolation frequency of fecal Coliforms from the selected school`s commonly touched different environmental surfaces. Mean 2=negative; 1=positive.
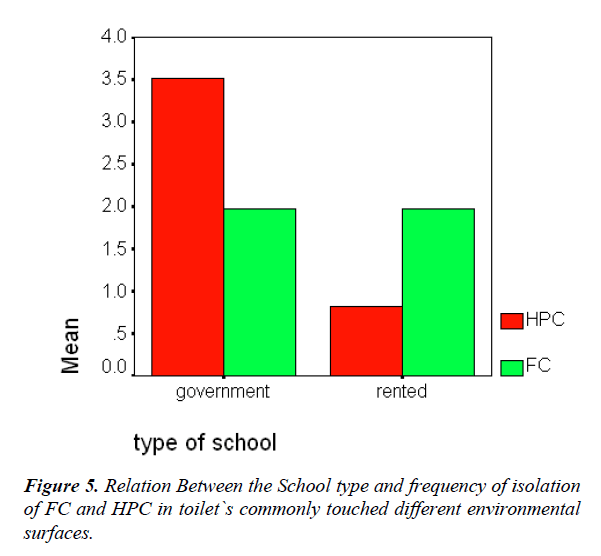
Figure 5 showed that no difference regarding isolation frequency of the FC while for HPC the governmental schools showed higher bacterial colony count than the rented schools from the whole swabbed commonly touched different environmental surfaces.
Discussion
Studies have shown that potential pathogens found in the school environment, particularly in the daycare and primary schools. These bacteria transmitted through a variety of means including direct person to person spread or contact with body fluids, contact with droplets or airborne spread by droplet nuclei, and indirect transmission through hand contact with a contaminated intermediate object. School attendance is a recognized risk factor for infectious diseases among children. Of particular concern is the increased possibility of the development of antimicrobial- resistant bacteria among these children. Daycare attending children have an increased relative risk for respiratory and gastrointestinal infections and double the risk of otitis media than non-day care-attending children. Increased contact between day care-attending children causes this increased risk and subsequently increased exposure to infectious organisms [13].
In the present study Among 592 (100%) microbiology swab samples of the selected command from selected commonly touched environmental surfaces only 15 (2.5%) showed positive for fecal coliforms with the highest isolation frequency from toilet washer 11 (14.9%) of the 15 total positive samples followed by sink wall 3 (4%) and finally the class door handle 1 (1.4%) of the 15 total positive samples. As shown in Table 1. While in relation to bacterial counts from the same surfaces among the swabbed selected commonly touched different environmental surfaces the highest HPC results were obtained from toilet washer handle as the Mean ± SD was (21.43 ± 68.01) followed by sink wall samples HPC Mean ± SD was (1.43 ± 7.12) then class door handle HPC Mean ± SD (.26 ± 2.21) while the other surfaces showed negative result as shown in Table 2. WENIGER et al. in 1983 how reported that among 298 surfaces samples in the primary schools only 17 (4.3%) showed positive results for Fecal Coliform Positive specimens mainly obtained from toilets, floors, furniture, and a refrigerator handle [15]. Currin et al. reported the same, in 1999 as his study revealed that the number of samples with fecal contamination bacteria taken from flush handles in schools was much higher (Group D streptococcus in 71%, E. coli in 57%). Also goes for the total number of smears. That the level of general and personal hygiene in schools is shallow [16]. On the other hand, there were weak positive correlation between Humidity and number of positive fecal Coliforms swabs as shown in Table 3 and Figure 1. Meanwhile it showed negative correlation between Humidity and Heterotrophic Plate Count among the swabbed commonly touched different environmental surfaces in the selected schools as shown in Table 4 and Figure 2. However in relation to temperature the reverse was noticed as Table 5 and Figure 3 there were weak positive correlation between temperature and Heterotrophic Plate Count while in Table 5 and Figure 4 there was negative correlation between temperature and percentage of isolation frequency fecal Coliforms among the swabbed commonly touched different environmental surfaces which were compatible with the results of KALTENTHALERl, et al. Whom reported that there did not appear to be a correlation with either hand or swab counts and relative humidity or temperature [2]. WILKINSON found that the influence of various humidities (10, 65, and 100% RH) on the survival of some gram-negative bacteria on metal surfaces held at 25°C at an initial concentration of 107 cells per surface, they reported that a 4-log drop in viability was evident after 14.5 days at 10% RH, after 2.5 days at 65%, after 1.5 days at 100% RH. (7) Furthermore, Robin et al. reported that bacterial survival is reduced in humid environments as the bacteria can be considered hygroscopic bodies whose desiccation rate changes according to the relative humidity of the environment, When fixed on the supports and placed in a humid environment, they rapidly recharge themselves with water. That rehydration leads to a conformational change in the cell structures, the result of which is to reduce their activity significantly. In addition, depending on the type of micro-organism, whether it is a Gram-negative bacillus or a Gram-positive coccus, the osmotic shock from rehydration has more or less lethal consequences, they reported that the surface itself may be a contributing factor as the highest mortality measured on the PVC surface, and then decreasingly on glass and steel, they found that a surface of steel, seems inert in relation to germs. On a dry steel surface in a dry environment, bacterial cells can remain in a quiescent condition for several weeks, awaiting conditions more favorable to their development. They found that polypropylene (PP) support, as a polymer, which used because it is much more stable than PVC, only becomes active at high temperatures. When they contaminated PVC and PP supports using a calibrated Enterococcus faecalis aerosol in order to evaluate the survival rate of the bacteria incubated on these different surfaces, they found that PVC had a significant effect on survival of the bacteria, with inactivation of around 90% of the initial population after 96 h at an RH close to 0% at 25°C. On the other hand, no significant mortality noticed on the PP support. This result confirmed their hypothesis on the lethality caused by the reactive polymeric structure of PVC. They concluded that the immediate environment of the micro-organisms is also essential, as humid environments favor airborne cell adhesion, and inversely humidity has a lethal action on those cells if the supports are nutrient-free. On the other hand, immobilized cell survival under the same conditions is increased up to several weeks by dehydration or, more generally, dry environments. Later provision of nutrients, even in minimal quantities, and increased relative humidity are sufficient to ensure the revival of these quiescent micro-organisms [13,15,16]. An agreed point that could not deny is that no single positive sampled item reported positive again, a finding that has been pointed to by Robin et al., bacterial survival reduced in humid environments. In the present study, there was no difference between the governmental and rented school buildings regarding isolation frequency of the FC while for HPC the governmental schools showed higher bacterial colony count than the rented schools from the whole swabbed commonly touched different environmental surfaces. However, the limited numbers of examined rented schools might be the affecting factor due to the limitation of data.
Conclusion
The survival and transfer of potentially pathogenic bacteria via environmental surfaces are possible.
Single hand contact with contaminated surface results in a variable degree of enteric pathogen transfer.
Relative humidity positively associated with more prolonged persistence for bacteria on hard surfaces.
The school’s environmental surfaces mainly in toilets could serve as a potential transmission route for gastrointestinal pathogens in the community.
The epidemiological evidence to date shows that raising awareness about the importance of critical procedures, such as through hand-washing and surface hygiene (particularly hand and food contact surfaces) will have a considerable impact in the control and prevention of infectious organisms.
Recommendations
Proper hand washing promotion for the children in all school toilets.
All schools should supply with soap containers that frequently changed and a proper drying tissue rolls for reduction of pathogens transmission.
A strategy must create for cleaning and Disinfection of environmental surfaces including toilet washer handle in school’s toilets to reduce the risk of transmission of enteric pathogens from inanimate surfaces to susceptible patients.
Identified all people are experiencing nausea, vomiting, and diarrhea by doing a roll call and asking for symptoms weekly.
Cleaning of all potentially contaminated areas in the school on regular bases is necessary.
References
- Rutala WW, Weber DJD. Healthcare Infection Control Practices Advisory Committee (HICPAC). Guideline for disinfection and sterilization in healthcare facilities. 2008;1-158.
- Kaltenthaler EC, Elsworth AM, Schweiger MS, et al. Faecal contamination on children’s hands and environmental surfaces in primary schools in Leeds. Epidemiol Infect. 1995;115:527-34.
- Sandora TJ, Shih MC, Goldmann DA. Reducing Absenteeism from Gastrointestinal and Respiratory Illness in Elementary School Students: A Randomized, Controlled Trial of an Infection-Control Intervention. Pediatrics. 2008;121:e1555-62.
- https://eportal.mountsinai.ca/Microbiology//faq/transmission.shtml
- Döring G, Bareth H, Gairing A, et al. Genotyping of Pseudomonas aeruginosa sputum and stool isolates from cystic fibrosis patients: Evidence for intestinal colonization and spreading into toilets. Epidemiol Infect. 1989;103:555-64.
- Grabow WOK, Grabow WOK. Waterborne diseases Update on water quality assessment and control. Water SA. 1996;pp:193-202.
- Kagan LJ, Aiello AE, Larson E. The role of the home environment in the transmission of infectious diseases. J Community Health. 2002;27:247-67.
- Barker J, Bloomfield SF. Survival of Salmonella in bathrooms and toilets in domestic homes following salmonellosis. J Appl Microbiol. 2000;89:137-44.
- Skelly C, Weinstein P. Pathogen survival trajectories: an eco-environmental approach to the modeling of human campylobacteriosis ecology. Environ Health Perspect. 2003;111:19-28.
- Keswick BH, Pickering LK, DuPont HL, et al. Survival and detection of rotaviruses on environmental surfaces in day care centers. Appl Environ Microbiol. 1983;46:813-6.
- Bright KR, Boone SA, Gerba CP. Occurrence of Bacteria and Viruses on Elementary Classroom Surfaces and the Potential Role of Classroom Hygiene in the Spread of Infectious Diseases. J Sch Nurs. 2010;26:33-41.
- Sandora TJ. A Randomized, Controlled Trial of a Multifaceted Intervention Including Alcohol-Based Hand Sanitizer and Hand-Hygiene Education to Reduce Illness Transmission in the Home. Pediatrics. 2005;116:587-94.
- Tambekar DH, Shirsat SD. Hand Washing: A Cornerstone to Prevent the Transmission of Diarrhoeal Infection. Asian J Med Sci. 2009;1:100-3.
- Harley JP, LMP. Laboratory Exercises in Microbiology, Fifth Edition. McGraw−Hill Companies, Inc, New York. 2002;1:1-5.
- Weniger BG, Ruttenber AJ, Goodman RA, et al. Fecal coliforms on environmental surfaces in two day care centers. Appl Environ Microbiol. 1983;45:733-5.
- Curin K, Pavic S. Hygienic conditions in elementary and secondary schools in the county of Split-Dalmatia. Arh Hig Rada Toksikol. 1999;50:273-81.