Research Article - Journal of Pregnancy and Neonatal Medicine (2024) Volume 8, Issue 1
RISK FACTORS AND NEONATAL OUTCOMES ASSOCIATED WITH PRETERM BIRTH AT ERASMO MEOZ UNIVERSITY HOSPITAL (HUEM) â?? CÃ?CUTA, COLOMBIA.
Galvis. P1*, Rojas. E2, Hernandez. N2, Gonzalez. S3, Cortez. M31Obstetrician-gynecologist, Perinatologist. Scientific Director, Maternal-Fetal Medicine Unit, Norfetus. Perinatologist, Erasmo Meoz University Hospital. President, Santander Association of Maternal-Fetal Medicine,
Cucuta, Colombia
2Medical Students, University of Pamplona. Research Group SISPE. Research Group KIDO, Cucuta, Colombia.
3Medical Students, University of Pamplona, Cucuta, Colombia
- *Corresponding Author:
- Pablo Galvis
Students, University of Pamplona
Research Group SISPE
Research Group KIDO, Colombia
E-mail: pgcenturi@gmail.com
Received: 6-Feb-2024, Manuscript No. AAPNM-24-127012; Editor assigned: 10-Feb-2024, PreQC No. AAPNM-24-127012(PQ); Reviewed: 24-Feb-2024, QC No. AAPNM-24-127012; Revised: 29-Feb-2024, Manuscript No. AAPNM-24-127012(R); Published: 8-Mar-2024, DOI: 10.35841/aapnm-8.1.190
Citation: Galvis P. Risk factors and neonatal outcomes associated with preterm birth at erasmo meoz university hospital (EMUH)-Cucuta, Colombia. J Preg Neonatal Med. 2023;8(1):190
Keywords
preterm birth, risk factors, maternal-fetal morbidity, pregnancy, preterm birth.
Introduction
Preterm birth, according to the World Health Organization WHO), is defined as delivery occurring between the 22nd and 37th weeks of gestation. Additionally, it is categorized based on gestational age into extreme preterm less than 28 weeks), very preterm 28 to 32 weeks), and moderate to late preterm 32 to 37 weeks) [1]. Children born prematurely face an increased risk of complications throughout their lives, impacting their physical and emotional well-being and resulting in higher healthcare costs. Premature birth is considered the leading cause of perinatal morbidity and mortality worldwide [2].
Pre-term childbirth is one of the main problems in obstetrics; it has an incidence of approximately 10-11%, although this varies between different populations and depending on the risk factors that are present; for the population of U.S.A ranges between 8.1 and 9.6%; for European countries the data place Spain between 5 and 8% and Germany with 3.6%; for African countries the figures are around 18% [2,3]; in general in Latin America there are no reliable statistics on preterm birth , but is estimated to exceed 10% of total births [3]; some small studies in South America mention premature figures of 5.1% for Ecuador [4], 8.5% for Peru [5] and for Colombia there are not many studies related to prematurity, but in 2019 the figure of 10.4% is reported in a pregnant population of Bogotá [5]. Beck and collaborators identified data from 92 countries worldwide and estimated an overall prevalence of 9.6% for 2005 and Benclowe and collaborators of 11.1% for 2010 [6].
Various risk factors associated with preterm birth include low socioeconomic status, maternal age at the extremes of life), infections such as urinary tract infection or vaginosis, premature rupture of membranes, chorioamnionitis, preeclampsia, multiple pregnancies, and other fetal risk factors like oligohydramnios and intrauterine growth restriction IUGR) [5,7]. Early identification of these risk factors in both pregnant women and children born prematurely allows for effective prenatal and postnatal interventions aimed at reducing morbidity and mortality [7].
Materials and Methods
The present investigation adopts a descriptive framework, focusing on a sample derived from the entirety of gravid patients attending the Gynecology and Obstetrics service at Erasmo Meoz University Hospital HUEM). This study encompasses all deliveries occurring between the 24th and 36.6th weeks of gestation, spanning from January 2020 to December 2021. The total sample comprises 1023 instances of preterm births over this biennial timeframe, with exclusions applied to cases lacking comprehensive information.
A meticulously crafted technical form was employed for systematic data collection, leveraging a thorough examination of individual medical records. Subsequently, the accrued data were meticulously transcribed into a Microsoft Excel database, facilitating their subsequent in-depth analysis and nuanced interpretation. This methodological approach ensures a rigorous examination of pertinent clinical factors, fostering a comprehensive understanding of preterm birth dynamics within our cohort.
Results
Initially, we will describe the characteristics of the studied population concerning maternal age, place of residence urban or rural), education, and socioeconomic stratum. Subsequently, we will record the obstetric characteristics of the evaluated pregnant individuals: gestational age at the time of preterm birth, obstetric formula, number of prenatal consultations, delivery method, and history of prematurity. Concluding the results, we will highlight the various risk factors assessed in our study and present the newborn data.
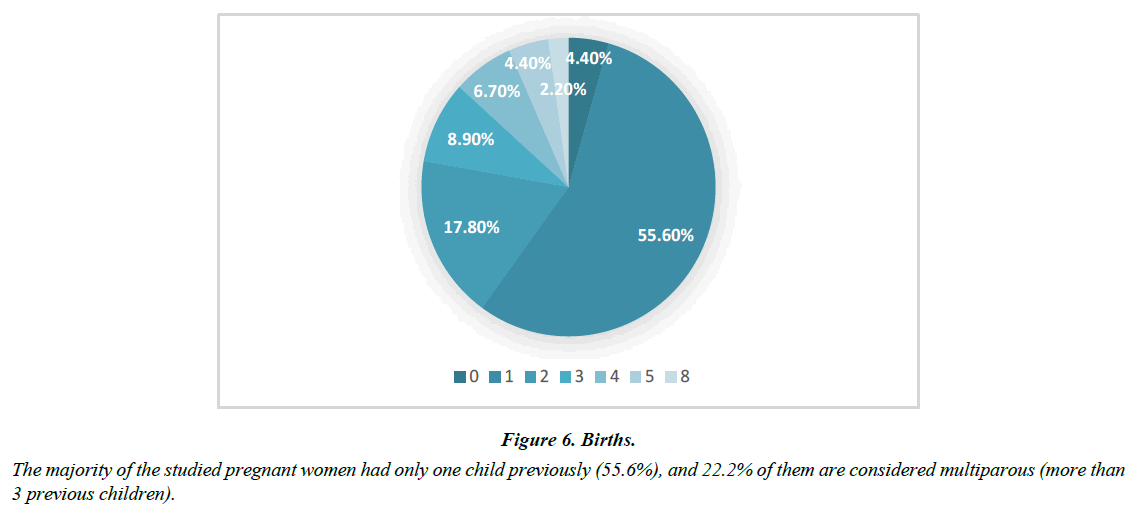
Characteristics of the Pregnant Population
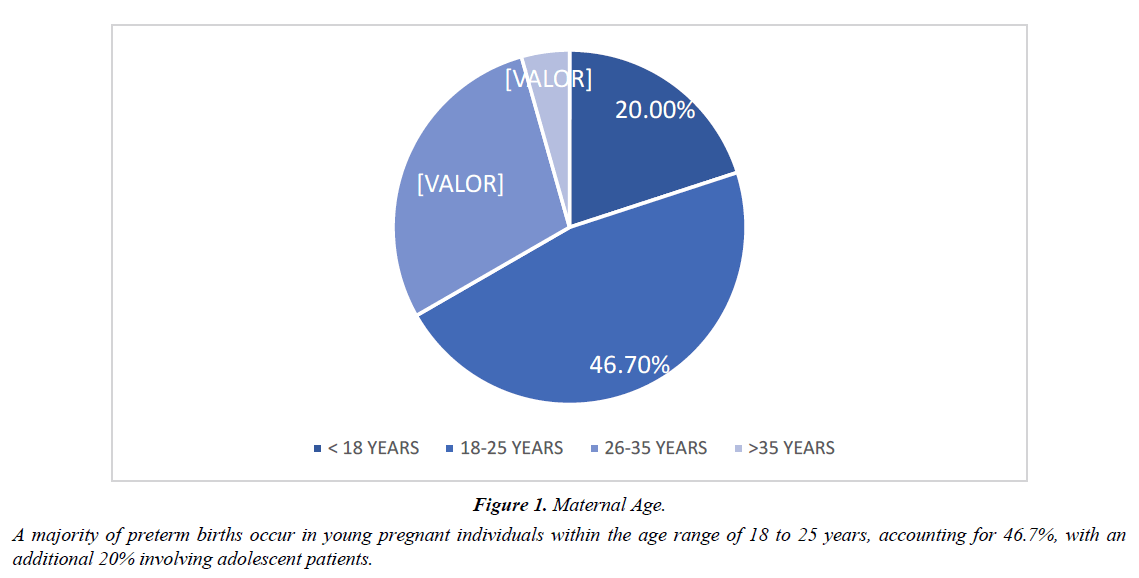
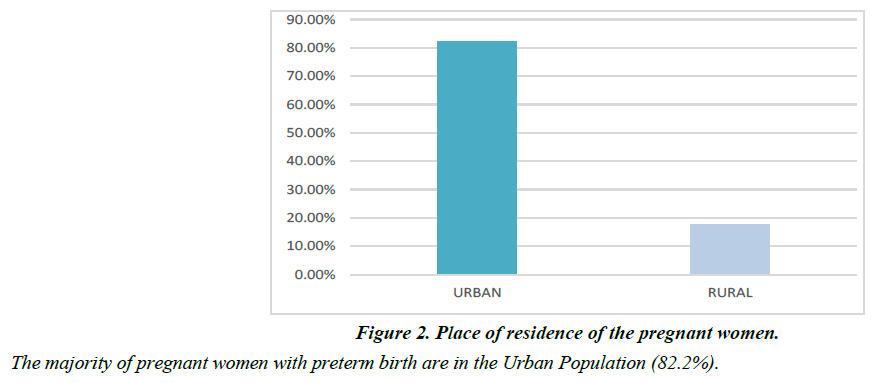
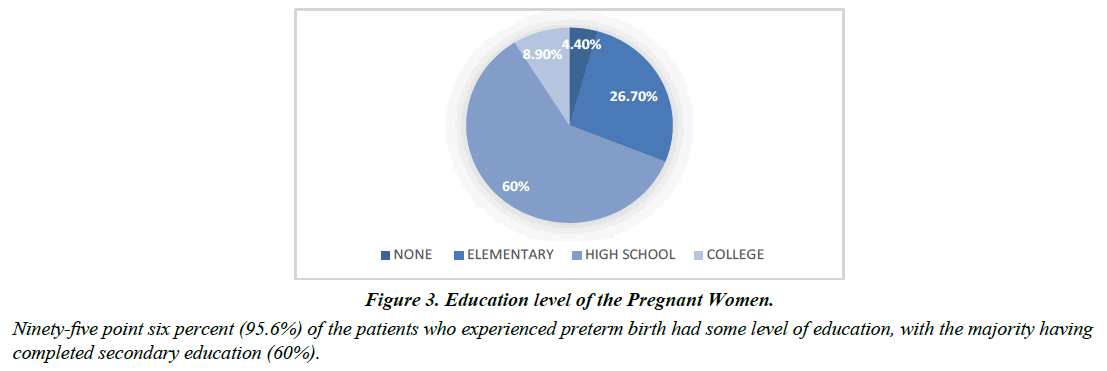
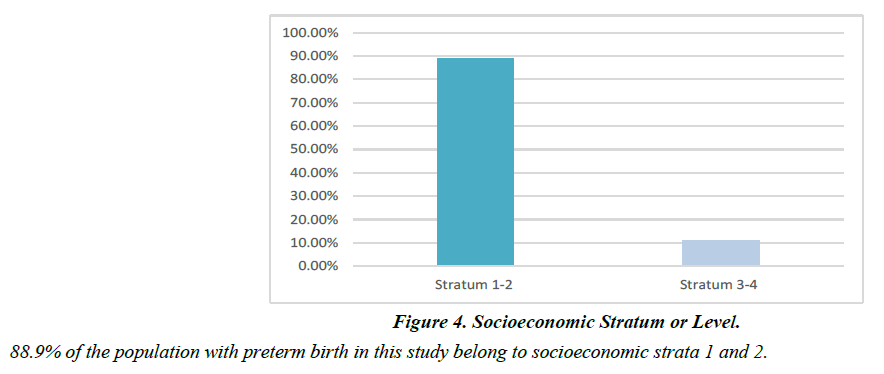
A majority of preterm births occur in young pregnant individuals within the age range of 18 to 25 years, accounting for 46.7%, with an additional 20% involving adolescent patients (Table 1, Figure 1). The majority of pregnant women with preterm birth are in the Urban Population 82.2%) (Figure 2). Ninety-five point six percent 95.6%) of the patients who experienced preterm birth had some level of education, with the majority having completed secondary education 60%) (Figure 3). 88.9% of the population with preterm birth in this study belong to socioeconomic strata 1 and 2 (Figure 4). The most predominant gestational age at the time of delivery was > 32 weeks, accounting for 89% (Figure 5). The majority of the studied pregnant women had only one child previously 55.6%), and 22.2% of them are considered multiparous more than 3 previous children) (Table 2, Figure 6). 32.6% of the patients had not had prenatal check-ups previously, and 38.3% of the pregnant women attended more than 4 prenatal consultations (Table 3, Figure 7). The majority of pregnant women had a high delivery method 90.8%), with only 9.2% having a vaginal delivery (Figure 8).
| Prenatal consultions | Percentage |
|---|---|
| 0 | 32,60% |
| 1 to 3 | 29,10% |
| 4 to 6 | 30% |
| >7 | 8,30% |
| TOTAL | 100% |
Table 1. A majority of preterm births occur in young pregnant individuals within the age range of 18 to 25 years, accounting for 46.7%, with an additional 20% involving adolescent patients.
| Births | Percentage |
|---|---|
| 0 | 4.40% |
| 1 | 55.6% |
| 2 | 17.80% |
| 3 | 8.90% |
| 4 | 6.70% |
| 5 | 4.40% |
| 8 | 2.20% |
| TOTAL | 100% |
Table 2. Births
| Prenatal Consultations | Percentage |
|---|---|
| 0 | 32.60% |
| 01-Mar | 29.10% |
| 04-Jun | 30.00% |
| >7 | 8.30% |
| TOTAL | 100% |
Table 3. Number of Prenatal Consultations
History of Preterm Births.
Within the 95.6% of pregnant women studied, who had already had at least one child, 33.3% of them experienced premature birth in previous pregnancies.
Risk factors for preterm birth
Our study aims to describe a series of risk factors for Preterm Birth in our pregnant population. We will present each of them along with their respective outcomes. Urinary Tract Infection UTI) was observed in 51.1% of the evaluated pregnant women (Figure 9). The 22.2% of the study population presented vaginal infections (Figure 10).
Premature rupture of membranes
Premature Rupture of Membranes RPM) associated with preterm birth is reported at 35% in global literature, whereas in this study, it was observed in 40% of the analyzed cases.
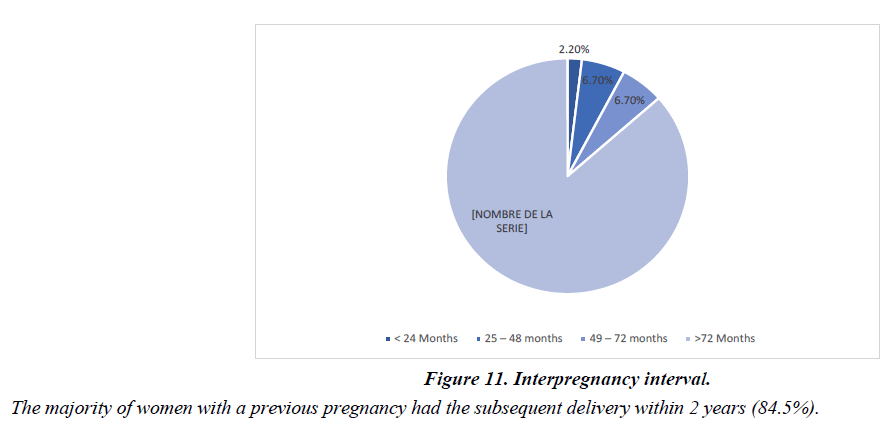
The majority of women with a previous pregnancy had the subsequent delivery within 2 years 84.5%) (Figure 11). Only 24.4% experienced obstetric hemorrhage, with no evidence of placenta previa or placental abruption 95.5% of patients did not have placenta previa or low-lying placenta, and there were no cases of premature placental detachment) (Figure 12). As a precedent to preterm birth, 29.6% of patients with preterm birth reported having experienced hypertensive disorder (Figure 13). 73.3% of the population did not have anemia, a fact correlated with good management of iron sulfate during pregnancy (Figure 14).
Newborn data
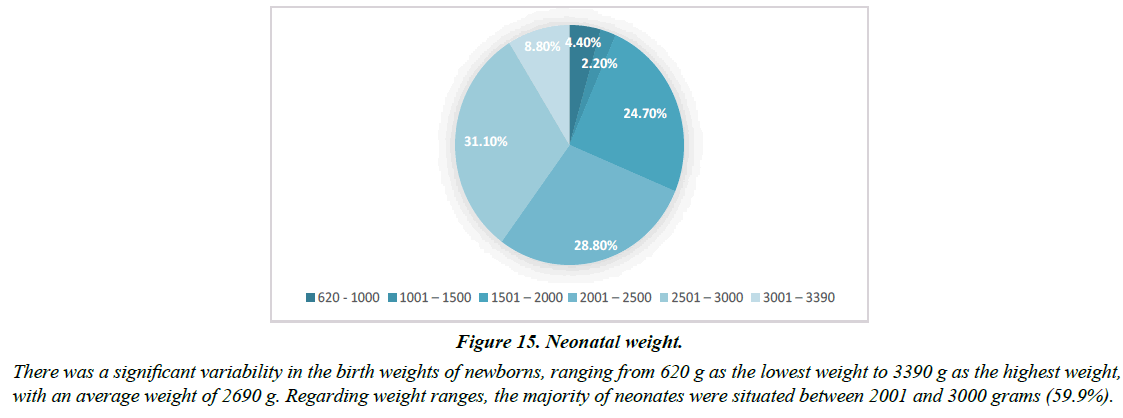
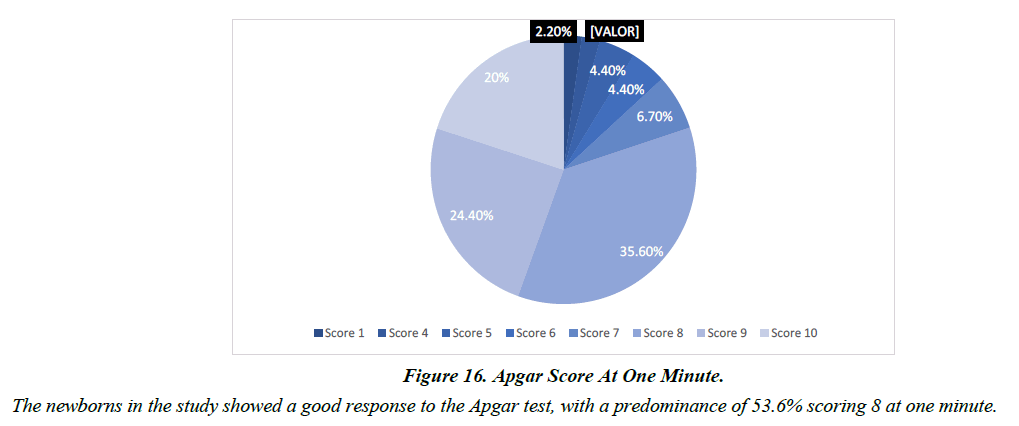
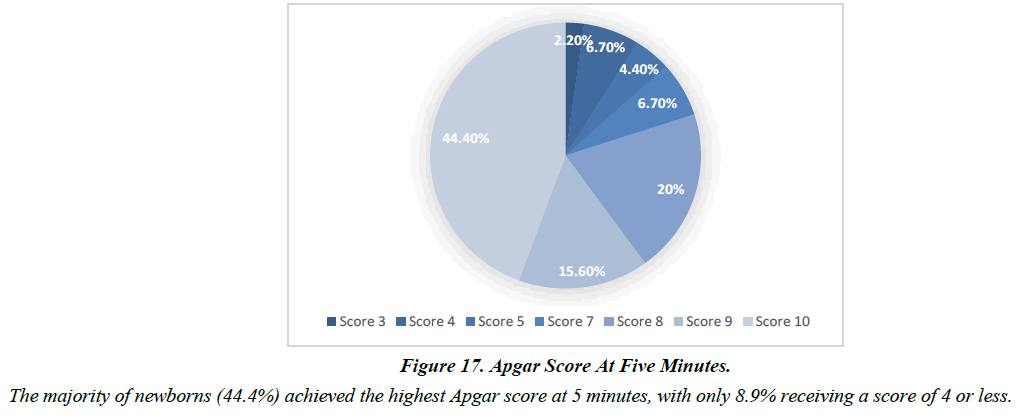
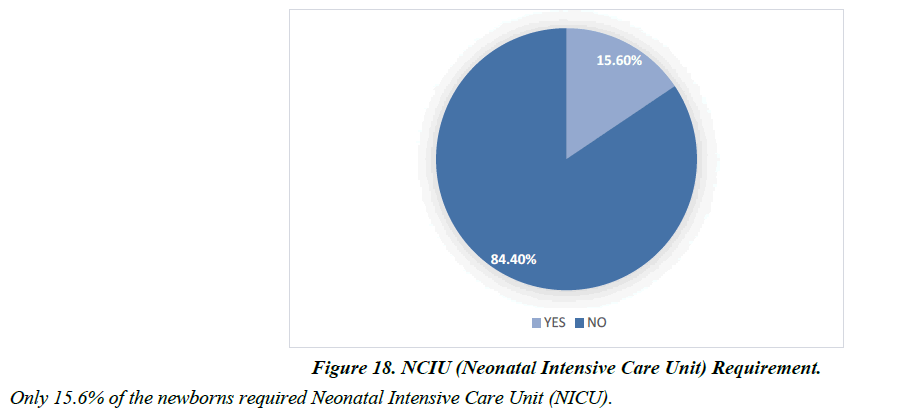
There was a significant variability in the birth weights of newborns, ranging from 620 g as the lowest weight to 3390 g as the highest weight, with an average weight of 2690 g. Regarding weight ranges, the majority of neonates were situated between 2001 and 3000 grams 59.9%) (Table 4, Figure 15). The newborns in the study showed a good response to the Apgar test, with a predominance of 53.6% scoring 8 at one minute (Figure 16). The majority of newborns 44.4%) achieved the highest Apgar score at 5 minutes, with only 8.9% receiving a score of 4 or less (Figure 17). Only 15.6% of the newborns required Neonatal Intensive Care Unit NICU) (Figure 18).
| WEIGHT (mg) | Percentage |
|---|---|
| 620 - 1000 | 4.40% |
| 1001 – 1500 | 2.20% |
| 1501 – 2000 | 24.40% |
| 2001 – 2500 | 28.80% |
| 2501 – 3000 | 31.10% |
| 3001 – 3390 | 8.88% |
| TOTAL | 100% |
Table 4. Neonatal Weight
Figure 15: Neonatal weight.
There was a significant variability in the birth weights of newborns, ranging from 620 g as the lowest weight to 3390 g as the highest weight, with an average weight of 2690 g. Regarding weight ranges, the majority of neonates were situated between 2001 and 3000 grams (59.9%).
Discussion
During the study period spanning from January 2020 to December 2021, a total of 12,902 deliveries were documented at Erasmo Meoz University Hospital. Among these, 1,023 were identified as preterm births, constituting 7.9% of the total. This proportion aligns closely with figures reported in studies conducted in the United States and Andean countries in South America but exceeds those reported in European contexts. Nonetheless, when compared to Colombia specifically, this rate falls below that reported in a study conducted in Bogotá, where the prevalence of prematurity was documented at 10.4%.
Within our cohort of pregnant individuals, the age group most prominently represented was between 18 and 25 years, accounting for 48.2% of cases. This finding mirrors observations made in analogous studies conducted in Latin American nations such as the Dominican Republic in 2018 and Peru between 2011 and 2013. [16] Notably, there is a notable predilection for pregnancies in younger individuals and those residing in urban locales. [1] The findings of the 2018 Vogel study corroborate this trend, demonstrating a significantly elevated risk of preterm birth among younger women, particularly those under 20 years of age, in contrast to their counterparts aged 25 to 29 [8].
Regarding sociodemographic determinants such as maternal age predominantly between 18 and 25 years), residential location primarily urban), educational attainment 60% possessing intermediate educational levels), and low socioeconomic status as per the catchment population of Erasmo Meoz University Hospital), no statistically significant disparities were observed in comparison to antecedent investigations.
A wealth of evidence has illustrated a direct correlation between low socioeconomic status and heightened incidence of low birth weight. Consequently, it is imperative to account for these variances when formulating preventative and prenatal care strategies aimed at effectively mitigating the risk of preterm birth across diverse maternal age cohorts [9,10]. Extant literature underscores the protective role of receiving prenatal care, with 38.3% of our study's pregnant cohort attending four or more prenatal consultations. Furthermore, there exists a demonstrable association between delayed initiation of prenatal care, particularly in the third trimester, and increased risk of preterm birth [11].
Prenatal visits wield considerable influence over pregnancy outcomes; notably, 36% of patients in our cohort did not specify the frequency of their prenatal visits, thereby heightening the likelihood of preterm birth. [8] Among those who did engage in prenatal care, nearly half sought services outside the hospital setting, which may attenuate the degree of oversight afforded by obstetric providers during labor. Notably, a study conducted by Dr. Javier Alexander Rivera Salas in 2015-2016 identified lack of prenatal care as the most prevalent cause of preterm birth, accounting for 64.1% of cases [12].
Regarding the mode of delivery, the majority of the study population at Erasmo Meoz Hospital underwent cesarean section, with a percentage of 90.8%. This largely depends on the individualization of cases, where, according to the clinical presentation and specifically the gestational age and associated morbidity, it would ultimately result in scheduled cesarean section. According to the conclusions of the 2013 Cochrane Review, there is no support for the superiority of the vaginal route in premature births [13].
Now, concerning obstetric complications during pregnancy, while they are relatively uncommon, they remain significant risk factors for preterm birth. In this study, several risk factors associated with preterm birth were identified, including urinary tract infection, premature rupture of membranes, obstetric hemorrhage, genital tract infection, hypertensive disorder such as pre-eclampsia, and maternal anemia; these findings are consistent with existing literature documenting the association of all these factors with preterm birth.
In relation to other studies, known predominant risk factors include Urinary Tract Infection [14], which in our study showed higher figures compared to those reported in Latin American literature 48.9%). Second most frequent was the presence of Premature Rupture of Membranes 40%), which due to its physiological behavior ends up being similar in the majority of premature birth investigative studies worldwide, with reported figures around 35%, but lower than other studies such as Escobar-Padilla and Gordillo-Lara in 2015 [15]. The next Risk Factor associated with Prematurity is a history of previous Preterm Birth 33.3%), representing one-third of the population, yet globally, figures of 49-50% are recorded, highlighting the importance of early evaluation and follow-up for those with a history of Preterm Birth.
Additionally, there was the presence of Hypertensive Disorder, specifically Pre-eclampsia, with a statistical association of 29.6% of cases linked to preterm birth at Erasmo Meoz Hospital. A study conducted in Bogotá, Colombia in 2018-2019, highlighted preeclampsia as one of the most significant risk factors, demonstrating that a diagnosis during the current gestation increases the risk of preterm birth fivefold compared to the absence of such diagnosis. Likewise, it was observed that the diagnosis of severe preeclampsia was of greater relevance, aligning with various studies worldwide.
Obstetric Hemorrhage associated with Prematurity was present in 24.4% of cases, where it is not necessarily related to second-half pregnancy bleeding grades Placenta Previa and Placental Abruption).
Cervicovaginal infections represent a risk of Preterm Birth in pregnant women, and in our study, they were associated with 22.2%, similar to a study from Ecuador published in 2018 23%), but lower than the study by Coiscou, Clarck, and Charitable in 2013, where vaginal infections were highlighted at 44.5% [7]. Previous research has established links between specific infections and prematurity. For example, a meta-analysis conducted by Olson et al. Shows a relationship between specific Chlamydia trachomatis infection and preterm birth, and a Mexican study also demonstrated a statistically significant association between concurrent urinary and cervicovaginal infections and the outcome of preterm birth.
Anemia was associated with a low risk of preterm birth, contrasting with a study conducted at Nuestra Señora de Altagracia University Hospital in the Dominican Republic published in 2022, where it is associated with prematurity in 31.6% [16].
On the other hand, if the aforementioned risk factors are not detected and treated early, there is a significant risk of complications in the newborn, such as respiratory, neurological, cardiovascular, gastrointestinal, and immunological pathologies that may persist and affect their quality of life into adulthood. Moreover, these complications can increase the likelihood of mortality. In a 2023 review, it is mentioned that the most common complications are respiratory, including Respiratory Distress Syndrome caused by a deficiency in pulmonary surfactant due to either lung immaturity or genetic alterations. However, the main causes of mortality in neonates are neurological complications such as intraventricular hemorrhage, which occurs within the first 10 days of life. [14] Premature newborns who experienced complications primarily had Respiratory Distress Syndrome, a considerably high figure at 69%, followed by other causes accounting for 20%, and a group of preterm newborns without complications, barely at 11% [17].
In our study, there is wide variability in the measures of weight average 2,690 grams) and length average 46 cm) of newborns, which corresponds to similar figures within the population of preterm neonates in Latin America. Additionally, it is noteworthy that the majority of newborns obtained favorable Apgar scores, with 53.6% scoring 8 at one minute of life and 44.4% achieving the maximum score at 5 minutes. Only 15.6% of newborns required neonatal intensive care. The case-control study by Jiang complements these findings by demonstrating that newborns in cases of preterm birth had adverse perinatal outcomes with lower birth weight and lower Apgar scores compared to the control group. These results are consistent with previous reports suggesting that male babies have a significantly higher risk of being born prematurely than females and confirm that preterm birth is often associated with unfavorable [5] perinatal outcomes, primarily at gestational ages far from term, which does not apply to our study because 88.9% of the patients were over 35 weeks gestation [18].
The combination of these findings highlights the importance of neonatal care and attention in cases of preterm birth, as premature newborns tend to face additional health challenges, such as lower birth weight and lower Apgar scores. These results underscore the need for specialized care strategies for preterm newborns and support for mothers at risk of preterm birth, a situation that is well recognized in our hospital. Implementation of strategies to reduce the morbidity of these neonates, such as the Kangaroo Care Plan, has been in place for several years [19].
Conclusion
In conclusion, the population that showed a higher frequency of preterm birth was the age group of 18-25 years, urban area residents, with basic secondary education, socio-economic strata 1 and 2, and subsidized health insurance, commonly in a free union marital status, gestational age over 32 weeks, and without any method of contraception. Regarding the factors associated with preterm birth, it was determined that urinary infections are the most frequent, followed by premature rupture of membranes and anemia.
Ultimately, newborn data, gestational age, and weight serve as predictive factors for neonatal morbidity and mortality in adulthood. Based on this, these parameters were considered in our population, revealing a lower incidence of adequate weight for gestational age compared to data in newborns with low birth weight for gestational age and very low birth weight. This allows for establishing the existence and intensity of the relationship between the preterm birth entity and the condition of the children born to mothers with preterm pregnancies. Furthermore, while there are studies on very low birth weight infants from developed countries, few have analyzed morbidity and mortality in Latin America. One strategy to address this situation is for neonatal care centers to join specialized collaborative thematic networks, which, among other benefits, enable standardizing criteria, optimizing resources, comparing centers, and identifying the most beneficial medical practices.
References
- Organización Mundial de la Salud. Preterm birth. 2023.
- Blencowe H, Cousens S, Chou D, et al. Born too soon: the global epidemiology of 15 million preterm births. Reprod Health. 2013;10:1-4.
- Schaaf JM, Liem SM, Mol BW, et al. Ethnic and racial disparities in the risk of preterm birth: a systematic review and meta-analysis. Am J Perinatol. 2012:433-50.
- Leal MD, Esteves-Pereira AP, Nakamura-Pereira M, et al. Prevalence and risk factors related to preterm birth in Brazil. Reprod Health. 2016;13:163-74.
- Zerna-Bravo C, Rocío Fonseca-Tumbaco, Ana María Viteri-Rojas, et al. Identification of risk factors for preterm birth. Case study of Enrique C. Sotomayor Hospital. Revista Ciencia Unemi. 2018;1126):134–42.
- Ahumada JS, Barrera AM, Canosa D, et al. Risk factors for preterm birth in Bogota DC, Colombia. Rev. Fac. Med. 2020;684):556-63.
- Vogel JP, Chawanpaiboon S, Moller AB, et al. The global epidemiology of preterm birth. Best Pract Res Clin Obstet Gynaecol. 2018;52:3-12.
- Rene D, Morales V, Randy Escudero Farro, et al. Maternal risk factors associated with preterm birth: a multicenter study. Metropolitan Trujillo. 2014;62):143–7.
- Rivera Salas JA. Maternal and Fetal Factors Associated with Preterm Birth in Patients Treated at San Vicente de Paúl Hospital in the city of Pasaje. 2016.
- Sosa JLC, Flores JLS. Risk factors for preterm birth in pregnant women at belén de lambayeque provincial teaching hospital.2015;22):7–18.
- Martínez-Cancino GA, Díaz-Zagoya JC, Romero-Vázquez A. Risk factors associated with preterm birth in adolescents. Salud en Tabasco. 2017;231-2):13-18.
- Leventhal S. A gap between ideals and reality: the right to health and the inaccessibility of healthcare for Haitian migrant workers in the Dominican Republic. Emory Int'l L. Rev. 2013;27:1249.
- Alfirevic Z, Milan SJ, Livio S. Caesarean section versus vaginal delivery for preterm birth in singletons. Cochrane Database Syst Rev. 2012;6).
- Huertas Tacchino E. Preterm birth, causes and preventive measures.
- Escobar-Padilla B, Gordillo-Lara LD, Martínez-Puon H. Risk factors associated with preterm birth in a second level hospital. Rev Med Inst Mex Seguro Soc. 2017;554):424.
- Risk factors associated with preterm labor in pregnant women at the Maternity Hospital Nuestra Señora de la Altagracia. 2018.
- Cherres Pacheco, J. I., Saltos Gutiérrez, et al. Causes of preterm birth and neonatal complications. RECIAMUC. 2023; 71):265-272.
- Jiang M, Mishu MM, Lu D, et al. A case control study of risk factors and neonatal outcomes of preterm birth. Taiwan J Obstet Gynecol. 2018;576):814-8.
- Rivera Galvis. A., Tamayo Cetina. W. Adherence to the kangaroo care program at the Erasmo Meoz University Hospital, a state social enterprise, by attendees during the year 2016. Cucuta: University of Santander. 2017.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref