Commentary - Journal of Clinical Ophthalmology (2021) Volume 5, Issue 3
Retinal sensitivity improves in the long term after internal limiting membrane peeling in vitro-macular surgery
Agnes Glacet-Bernard*Department of Ophthalmology, Intercommunal Hospital Center and Henri Mondor Hospital, Paris-Est Creteil University (UPEC, Paris XII University), Creteil, France
- Corresponding Author:
- Dr. Agnes Glacet-Bernard
Department of Ophthalmology
Intercommunal Hospital Center and Henri Mondor Hospital
Paris-Est Creteil University
Creteil
France
E-mail: agnes.glacet@chicreteil.fr
Accepted date: 20 May, 2021
Citation: Bernard AG. Retinal sensitivity improves in the long term after internal limiting membrane peeling in vitro-macular surgery. J Clin Ophthalmol 2021;5(3):422-423.
Introduction
The Creteil team followed up eleven patients who underwent epiretinal membrane (ERM) and internal limiting membrane (ILM) removal for 18 months using microperimetry (MP-3 Microperimeter®, Nidek, Japan), which allows very accurate measurement of retinal sensitivity in the macular region before and after surgery.
Methods
Patients with vitreomacular interface disease requiring vitrectomy underwent multimodal retinal imaging, including visual acuity assessment, fundus color photograph, infrared, autofluorescence, Spectral-Domain Optical Coherence Tomography, Optical Coherence Tomography-Angiography and microperimetry (MP-3 Microperimeter®, Nidek, Japan). They were examined at baseline (M0), 6 months (M6) and 18 months (M18) after surgery. Retinal sensitivity was subdivided into three concentric polygons: Large, Medium, Small [1,3].
Results and Discussion
Eleven eyes of 11 patients were analyzed, including 10 epiretinal membranes (ERMs) and 1 macular hole. Mean age was 68 years old. Best-corrected visual acuity (BCVA) improved in all patients from 0.51 logarithm of the minimal angle of resolution (logMAR) to 0.067 with a statistically significant difference (p=0.0074). Retinal sensitivity improved between M0 and M6 in all polygons and continued to improve between M6 and M18 for polygons Medium (M) and Small (S) with no statistical significance. At M18, BCVA and retinal sensitivity were similar in the operated eye compared with the fellow eye for all patients. Dissociated optic nerve fiber layer appearance was observed in 75% patients at M18. It was not correlated with either retinal sensitivity or BCVA or microscotomas. No recurrence of ERM or macular hole occurred during follow-up.
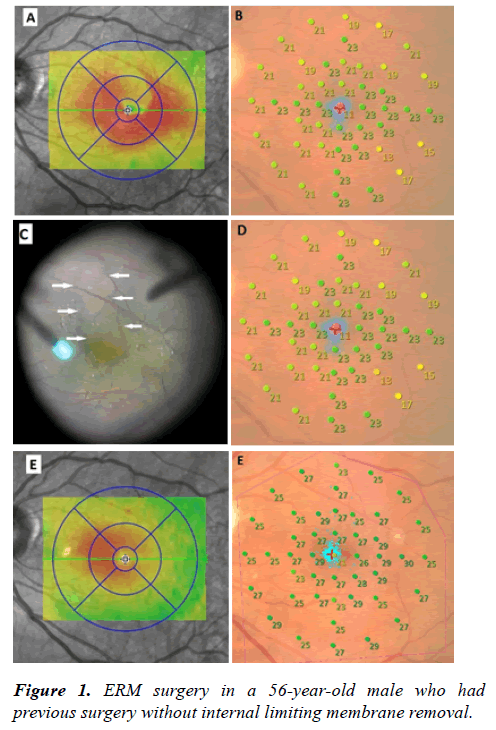
One year after the first surgery, BCVA was 20/63 with persistence of metamorphopsia.
SD-OCT showed a thickening of the macular region with a « double wings » shape. Initial mean retinal sensitivity was 21
dB. Peroperative findings showed the presence of ERM in front
of the persistent Brilliant Blue®-colored ILM; a small part of
the ILM had been spontaneously removed with the ERM
during the first surgical procedure in the supero-macular zone
(arrows), but ILM was still present at the fovea, responsible for
visual loss and decrease in retinal sensitivity. The area of the
spontaneous removal of the ILM corresponded to the area of normal retinal thickness on the preoperative SD-OCT. Six
months after the peeling of the ILM, both BCVA and retinal
sensitivity improved to 20/32 and 26.2. At M18, BCVA and
retinal sensitivity continued to improve respectively to 20/25
and 26.4 dB with no ERM recurrence (Figure 1).
This case is interesting because it shows that the presence of a pathological ILM following the first surgery is responsible for a decrease in vision and retinal sensitivity. Secondary peeling of the ILM results in normalization of retinal acuity and retinal sensitivity. Peeling of the ILM does not seem to have a deleterious effect in itself [3,6].
Conclusion
After surgery, the retinal sensitivity assessed by microperimetry gradually improved until the 18th month, and at the end was not different from the values of the fellow eye. These results seemed to confirm that ILM peeling can be an effective and safe technique to treat patients with vitreomacular interface disease.
References
- Blautain B, Glacet-Bernard A, Blanco-Garavito R, et al. Long-term follow-up of retinal sensitivity assessed by microperimetry in patients with internal limiting membrane peeling. Eur J Ophthalmol. 2021:1120672121997300.
- Kwok AKh, Lai TY, Yuen KS. Epiretinal membrane surgery with or without internal limiting membrane peeling. Clin Exp Ophthalmol. 2005;33:379-85.
- Feldman A, Zerbib J, Glacet-Bernard A, et al. Clinical Evaluation of the Use of Infracyanine Green Staining for Internal Limiting Membrane Peeling in Epimacular Membrane Surgery. Eur J Ophthalmol. 2008;18:972-9.
- Tadayoni R, Svorenova I, Erginay A, et al. Decreased retinal sensitivity after internal limiting membrane peeling for macular hole surgery. Br J Ophthalmol. 2012;96:1513-6.
- Park SH, Kim YJ, Lee SJ. Incidence of and risk factors for dissociated optic nerve fiber layer after epiretinal membrane surgery. Retina. 2016;36:1469-73.
- Kim YJ, Lee KS, Joe SG, et al. Incidence and quantitative analysis of dissociated optic nerve fiber layer appearance: real loss of retinal nerve fiber layer? Eur J Ophthalmol. 2018;28:317-323.