Research Article - Journal of Clinical Ophthalmology (2022) Volume 6, Issue 3
Retinal lesion on optical coherence tomography angiography (octa) of hemodialysis patients with diabetes mellitus.
Vu Tuan Anh1*, Pham Trong Van2, Le Anh Tam2, Nhung Ta Thi Kim3, Xuan Le Thi Thanh3
1Department of Optholmology, Vietnam National Eye Hospital, Hanoi, Vietnam
2Department of Preventive Medicine, Hanoi Medical University, Hanoi, Vietnam
3Department of Preventive Medicine and Public Health, Hanoi Medical University, Hanoi, Vietnam
- Corresponding Author:
- Dr. Vu Tuan Anh
Department of Optholmology
Vietnam National Eye Hospital
Hanoi
Vietnam
E-mail: tathikimnhung@hmu.edu.vn
Received: 04-Apr-2022, AACOVS-22-59540; Editor assigned: 07-Apr-2022, AACOVS-22-59540; (PQ); Reviewed: 21-Apr-2022, AACOVS-22-59540; Revised: 03-June -2022, Manuscript No- AACOVS-22-59540 (R); Published: 10-June-2022; DOI: 10.35841/AACOVS.6.3.1-5.
Citation:Tuan Anh V, Van PT, Tam LA, et al. Retinal lesion on optical coherence tomography angiography (octa) of hemodialysis patients with diabetes mellitus. J Clin Ophthalmol. 2022;6(3):1-5.
Abstract
Purpose: To describe the retinal lesion features among patients with diabetes mellitus on hemodialysis at the central Bach Mai hospital. Materials and methods: An observational study was applied, 44 eyes of 23 diabetes patients with hemodialysis was recruited. Data was collected including personal information, routine eye examination, taking color fundus photography, OCT, OCTA to find out the retinal lesions. Results: The average age of study participants was 62.9 ± 8.9. 56.6% were male, the average duration of diabetes was 16.73 ± 8.32 years; the majority of eyes with vision impairment accounted for 68.2%; the prevalence of eyes with macular edema were 27.3%; central retinal thickness measured on average OCTA was 256.63 ± 125.83 µm; 9/44 eyes have anemia (ischemia) on OCTA image. Conclusion: The retinal damage of diabetic patients on hemodialysis was severe. It is important to take the retinal examination with OCTA routinely can help diagnose, detect the retina lesions and prevent severe eye complications.
Keywords
Diabetic retinopathy, Hemodialysis, OCTA
Introduction
The prevalence of Diabetes Mellitus (DM) has been increasing rapidly in Vietnam as well as in the world [1-2]. Additionally, Chronic Kidney Disease (CKD) is also increasing being recognized as a global public health problem [3]. In patients with diabetes mellitus on hemodialysis, the eye (retinal) lesions are more severe [4]. This is group of patients with many difficulties in following and treatment, especially contraindications in fluorescein of angiography. However, there were very few studies on the effects of hemodialysis on retinal complications, such as changes in retinal thickness, retinal ischemia and macular edema, and results were variable [5-7].
Diabetic hemodialysis patients have severe systemic conditions. Although the eye lesions are not life threatening, but it would reduce quality of life. However, the research on the retinal lesion among diabetic patients was largely lacking. The examination routinely can help diagnose, detect the retinal lesions and prevent severe eyes complications. Therefore, we conducted this research to describe the retinal lesion features on OCTA in patients with diabetes mellitus on hemodialysis at the central Bach Mai Hospital.
Materials and Methods
Study subjects
From September 2020 to September 2021, a cross-sectional study was conducted to collected data from 23 diabetic hemodialysis patients with 44 eyes. The patients were diagnosis as diabetic hemodialysis patients by physicians at Center of Nephrology Urology and Dialysis, Bach Mai Hospital, a central general facility. All study participants were asked to get agreement for participation. We excluded patients those were too old, weak (physical disabilities), difficult to participate for examination. To control confounders, we also excluded the opacity of transparent structures (corneal scarring, grade IV cataracts, vitreous hemorrhage 3+) and difficulty dilating pupils.
Study variables and data collection methods
Data was collected from patients including demographic characteristics and examination checklists. Demography variables were age, gender, type of diabetes, duration of diabetes and dialysis time.
All patients were examined to best corrected visual acuity with Snellen chart. Anterior segment examination was applied by slit-lamp for cornea, anterior chamber and iris, lens situation. In addition, (retina was checked by bio microscopy with Volk 90D) posterior segment examination was by slit-lamp and ophthalmoscopy with Volk 90D lenses to identify retinal lesions and (grading) stage of diabetic retinopathy. Colour fundus photography by OCT and OCTA were performed. General examinations for all patients were done, including blood pressure, blood glucose and HbA1C.
Data analysis
All data was cleaned then entered using SPSS software to analysis. Descriptive analysis was used to display frequency and percentage of main indicators regards to diabetic retinopathy.
Macular edema was diagnosed based on the criteria of ETDRS [8], including
- Retinal thickening within 500 mm from the central point.
- Hard exudate within 500 mm from the central point, associated with adjacent retinal edema (edema may be outside the 500 mm limit).
- The thick retina was ≥ 1 disc diameter, within 1 disc diameter from the centre.
Classification of diabetic macular edema was by ICO [9] to three levels as mild, moderate and severe (Table 2).
Ethical consideration
The study was approved by the Scientific Research Council at Hanoi Medical University and official agreement by Rector Board of Bach Mai Hospital in 2021. All patients were asked to sign a written inform consent. All data were confidential for research purpose only.
Results
Characteristics of study participants
Among 23 study participants, the majority of the patients were males (56.6%). More than half of them were over 60 years old, in which 43.6% aged from 61 to 70 years old. Average age of the patients was 62.9 ± 8.9 years, ranged from 48 to 83 years old.
In the study of visual acuity characteristics of the group of patients, 19 eyes (43.2%) were low vision, 11 eyes (25%) were blind, and only 6 eyes (13.6%) have normal vision (Figure 1).
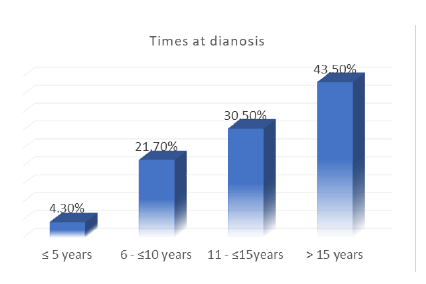
Of the 23 studied patients, most of the patients had diabetes for more than 15 years (10 people, 43.5%). There was one patient (4.3%) with diabetes under 5 years (Figure 2).
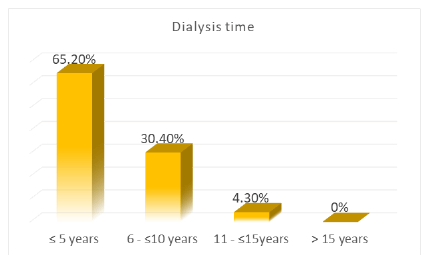
In our study, the number of patients with dialysis time of less than 5 years was 15 (65.2%). The group of patients with 6-10 years of dialysis time was 7 (30.4%). The group of patients with dialysis time of 11-15 years is the least, with 1 patient (4.3%). None of the patients had dialysis more than 15 years.
Features of retinal lesions on OCTA
Table 1 shows that the prevalence of diabetic retinopathy was high, accounted for 75% of study participants. Majority of diabetic retinopathy patients was mild (36.4%). The percentage of patients with proliferative Diabetic Retinopathy (DR) was low (6.8%). In addition, 9/44 eyes have anemia (ischemia) on OCTA image.
Table 1. Distribution of retinal lesions.
| Retinal lesions | Number of eyes | Rate (%) | |
|---|---|---|---|
| Non (apparent) DR | 8 | 18,2 | |
| Diabetic retinopathy | Mild | 16 | 36,4 |
| Moderate | 11 | 25,0 | |
| Severe | 6 | 13,6 | |
| Proliferative DR | 3 | 6,8 | |
| Total | 44 | 100 | |
The Table 2 shows that the prevalence of patients had eyes with macular edema were 27.3%. None of the patients had diabetic cystoid macular edema.
Table 2. Prevalence of diabetic macular edema (DME).
| Diabetic macular edema | Number of eyes | Rate (%) | ||
|---|---|---|---|---|
| No DME | 32 | 72,7 | ||
| Mild | 4 | 9,1 | ||
| DME | Moderate | 6 | 13,6 | 27,3 |
| Severe | 2 | 4,6 | ||
| Diabetic cystoid macular edema | 0 | 0,0 | ||
| Total | 44 | 100 | ||
The (Table 3) presents the central retinal thickness. The average level of central retinal thickness measured on OCTA was 265.63 ± 125.83 µm, of which the thickest was 929 µm and the thinnest was 181 µm.
Table 3.Central retinal thickness.
| Thickest | Thinnest | Mean ± SD | |
|---|---|---|---|
| Central retinal thickness | 929 | 181 | 265,63 ± 125,83 |
Table 4 displays characteristics of the central avascular zone. The surface area size of 44 eyes in the study was 0.6 ± 0.15 mm², and the circumference area was 3.4 ± 0.62. mm² while the central region measures 0.63 ± 0.064 mm² (Table 5).
Table 4.Characteristics of the central avascular zone.
| Characteristics of the central avascular zone | Average area |
|---|---|
| Surface Area | 0,6 ± 0,15 (mm²) |
| Circumference | 3,4 ± 0,62 (mm²) |
| Center area | 0,63 ± 0,064 (mm²) |
Table 5. Density of blood vessels in the surface of the retina.
| Mean ± SD (mm/mm2) | Minimum – maximum | |
|---|---|---|
| Central | 4,41 ± 2,1 | 0,3-11,6 |
| Peri central | 12,59 ± 2,96 | 2,9-18,6 |
| Total | 12,44 ± 2,25 | 6,6-17,3 |
In our study, the average density of blood vessels in the central area was 4.41 ± 2.1 (mm/mm²), the average density of the peri-central area was 12.59 ± 2.96 (mm/mm²) and the combined mean vascular density was 12.44 ± 2.25 (mm/mm²).
Discussion
Of the 23 studied patients, most of the patients had diabetes for more than 15 years (43,5%). The average time of diabetic diagnosis was 16,73 ± 8,32 years, similar to the study by Kameda (2020) at 17,4 ± 8,8 years [10] and Takamura (2020) at 16,18 ± 9,03 years [11]. However, the average time of diagnosis was higher than that in some national studies such as the author Nguyen Thi Lan Anh (8,98 ± 6,76 years) [12], Nguyen Thi Ngoc Han (5,8 ± 4,9 years) [13]. This difference can be explained by our study subjects were diabetic patients with end-stage renal failure one of the complications of diabetes. These complications only occur after has had diabetes for a relatively long time. So, it is appropriate to have the highest rate of patients with diabetes with chronic kidney failure in our study with the longest duration of diabetes.
In our study, the number of patients with dialysis time of less than 5 years was 15 (65.2%). Diabetic patients with late-stage renal failure requiring dialysis are most common in the early years of the combination of the two diseases. Over time, the number of patient’s decreases, end-stage renal disease as well as diabetes is incurable diseases, and the number of patients decreases over time with both diseases that may be related to life expectancy of the patient.
The prevalence of diabetic retinopathy in our study was high at 75%. It is higher than previous studies such as Micheal, et al. 71% [14], Tomic, et al. 64% [15], much higher than that in review of 35 studies by the study by Yau J.W.Y et al. in (34.6%) [16], El-Menyar, et al. in (45%) [17]. According to reports of domestic and international studies, the prevalence of diabetic retinopathy is very different. The rate of diabetic retinopathy encountered in our study was higher than previous studies because our study participants were diabetic patients with end stage chronic renal failure [18], having higher the average time of diagnosis of the disease. The percentage of patients with proliferative diabetic retinopathy in our study was lower than that in the study by Lee et al. in 2014 (6.8% vs. 21, 6%) [19]. In sum, the high percentage of patients having diabetic retinopathy at the end-stage chronic renal failure in our study indicates a common pathological change in the renal vasculature as well as the patient’s retina [20]. Our finding implies that to reduce the risk of blindness in patients with diabetes, patients need to be examined early, closely monitored, regularly and promptly treated for the retina’s damage.
Diabetic macular edema
Macular edema is a major cause of vision loss for diabetic patients and can occur at any stage of the disease [21]. The prevalence of patients had eyes with macular edema in our study was 27.3%. This rate is higher than that of the research results of Nguyen Thi Lan Anh of 7.4% [12], Nguyen The Vinh of 8% [22], Nguyen Thi Ngoc Han of 8,1% [13] and Varma et al. of 10,4% [23] A review study by Yau J.W.Y et al. in 2012 from 35 studies among 22.896 diabetic patients period 1980-2008 found that the prevalence of macular edema was 6.81% [16]. It can be explained by the longer duration of diabetes in the patients in our study. For example, in our study, the average time of diagnosis as diabetes was 16,73 ± 8,32 years, meanwhile in the study by Nguyen Thi Lan Anh, the time was 8,98 ± 6,76 years, by Nguyen Thi Ngoc Han it was 5,8 ± 4,9 years.
However, Azem et al reported the macular edema among diabetic patients with chronic renal failure on dialysis was 47,5% [24], that is higher than the prevalence in our study. It can be different of study participants. In Azem’s study, 100% patients had diabetic retinopathy, while the patients having eye with retinal lesions was 81.8% in our study.
Central retinal thickness
The average level of central retinal thickness on OCTA in our study was 265.63 ± 125.83 µm. The finding was similar to the study by Emre et al. when they also found central retinal thickness at average level among diabetic patients was 255,48 ± 9,96 µm and the study by Auyanet, et al. was 245,28 ± 52,21 µm [25].
Our study had some limitation. Firstly, the sample size was not representative for all diabetic patients with retinopathy then we could not generalize for all population. Secondly, we cannot anticipate risk factors for diabetic retinopathy to recommend for appropriate measures. These limitations should be solved out when we conduct a larger sample size and analytical method.
Conclusion
The retinal damage in patients with diabetes mellitus on hemodialysis was very diverse. The rate of severe lesions was also much higher than that of diabetes patients in the community. The retinal examination with OCT, OCTA can help diagnose, quantify macular edema, macular thickness and are also the gold standard for diagnosing the stage (grading) of diabetic retinopathy with clinical examination by ophthalmoscopy. Therefore, follow-up and examination routinely can detect the retina lesions, prevent severe eye (ophthalmic) complications and improve the quality of life for this special group of patients.
Acknowledgements
We are also grateful to the physicians at Center of Nephrology Urology and Dialysis, Bach Mai Hospital for our strong support during the studies field work.
References
- Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843.
- Ngoc NB, Lin ZL, Ahmed W, et al. Diabetes: What Challenges Lie Ahead for Vietnam? Ann Glob Health. 2020;86:1.
- Levey AS. National kidney foundation kidney disease outcomes-quality initiative classification, prevalence and action plan for stages of chronic kidney disease. Ann Intern Med 2003;139:137 - 147.
- Lee R, Wong TY, Sabanayagam C, et al. Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye and vision (London, England). 2015;2:17.
- Matsuo T. Disappearance of diabetic macular hard exudates after hemodialysis introduction. Acta medica Okayama. 2006;60(3):201-205.
- Perkovich BT, Meyers SM. Systemic factors affecting diabetic macular edema. Am J Ophthalmol. 1988;105(2):211-212.
- Tokuyama T, Ikeda T, Sato K, et al. Effects of haemodialysis on diabetic macular leakage. Br J Ophthalmol. 2000;84(12):1397-1400.
- Kameda Y, Hanai K, Uchigata Y, et al. Vitreous hemorrhage in diabetes patients with proliferative diabetic retinopathy undergoing hemodialysis. Journal of diabetes investigation. 2020;11(3):688- 692.
- Takamura Y, Matsumura T, Ohkoshi K, et al. Functional and anatomical changes in diabetic macular edema after hemodialysis initiation: One-year follow-up multicenter study. Sci Rep. 2020;10:77-88.
- Müller M, Schönfeld C-L, Grammer T, et al. Risk factors for retinopathy in hemodialysis patients with type 2 diabetes mellitus. Scientific Reports. 2020;10:1-10.
- Tomi? M, Ljubi? S, Kastelan S, et al. The role of inflammation and endothelial dysfunction in the pathogenesis of diabetic retinopathy. Collegium antropologicum. 2013;37:51-57.
- Yau JW, Rogers SL, Kawasaki R, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes care. 2012;35(3):556-564.
- El-Menyar A, Al Thani H, Hussein A, et al. Diabetic retinopathy: a new predictor in patients on regular hemodialysis. Current medical research and opinion. 2012;28:999-1055.
- Olafsdottir E, Andersson DK, Dedorsson I, et al. The prevalence of retinopathy in subjects with and without type 2 diabetes mellitus. Acta ophthalmologica. 2014;92:133-137.
- Lee WJ, Sobrin L, Kang MH, et al. Ischemic diabetic retinopathy as a possible prognostic factor for chronic kidney disease progression. Eye (London, England). 2014;28:1119-1125.
- Kotlarsky P, Bolotin A, Dorfman K, et al. Link between retinopathy and nephropathy caused by complications of diabetes mellitus type 2. International ophthalmology. 2015;35:59-66.
- Lang GE. Diabetic macular edema. Ophthalmologica Journal international d'ophtalmologie International journal of ophthalmology Zeitschrift fur Augenheilkunde. 2012;227:21-29.
- Varma R, Torres M, Peña F, et al. Prevalence of diabetic retinopathy in adult Latinos: The Los Angeles Latino Eye Study. 2004;111:1298-1306.
- Azem N, Spierer O, Shaked M, et al. Effect of Hemodialysis on Retinal Thickness in Patients with Diabetic Retinopathy, with and without Macular Edema, Using Optical Coherence Tomography. J Ophthalmol. 2014;2014:709-862.
- Auyanet, I LJR, E Bosch, et al. Measurement of foveal thickness by optical coherence tomography in adult haemodialysis patients with diabetic nephropathy.2011;66-69.