Research Article - Biomedical Research (2017) Volume 28, Issue 5
Research and analysis of mechanical ventilation in the treatment of pleural effusion caused by multiple rib fractures
Hui Zhang1#, Tingting Sun2#, Mingchen Feng1*1Department of Critical Care Medicine, Jining No.1 People’s Hospital, Jining, PR China
2Department of Surgery, Jining No.1 People’s Hospital, Jining, PR China
#These authors contributed equally for this work
- *Corresponding Author:
- Mingchen Feng
Department of Critical Care Medicine
Jining No.1 People’s Hospital, PR China
Accepted date: October 26, 2016
Abstract
Aim: This study is to investigate the effects of mechanical ventilation in the treatment of pleural effusion caused by multiple rib fractures.
Methods: A total of 44 patients with pleural effusion caused by multiple rib fractures admitted to our hospital from January 2013 to 2015 January were randomly divided into two groups, Com group (routine medical treatment group) and Mon group (mechanical ventilation group), with 22 cases in each group. Patients in Com group were given conventional medical treatment and those in Mon group were given conventional medical therapy combined with mechanical ventilation. Chest computed tomography (CT) and chest three-dimensional reconstruction (VRT) were performed at admission, the second day, the fourth day and the sixth day after admission. The activity of lactate dehydrogenase was detected by colorimetric method.
Results: Over time, the general clinical manifestations such as expiratory dyspnea of Mon group were less severe than those of Com group. Chest X-ray findings showed that over time, the lung texture of Mon group was clearer than that of Com group. Chest CT manifestations showed that over time, the amount of pleural effusion in Mon group was significantly lower than that of Com group (P<0.05).
Conclusion: Our results suggest that the treatment of pleural effusion caused by multiple rib fractures with conventional medical therapy combined with mechanical ventilation can promote fracture healing.
Keywords
Multiple rib fracture, Mechanical ventilation, Pleural effusion.
Introduction
Chest trauma is the most common injury in the emergency trauma and rib fractures is the most common trauma in chest trauma [1,2]. Rib fractures can also cause abdominal injury. Multiple fractures in multiple ribs are very severe chest injury, which are often associated with pulmonary contusion, pneumothorax, and hemorrhagic shock [3]. Severe rib fractures can cause paradoxical respiration and mediastinal swing, which has large effects on respiratory and circulatory system, result in acute respiratory distress syndrome (ARDS), and cause the death of patients [4]. Almost all the flail chest patients have lung contusion. In patients with chest trauma, there are respiratory secretions increase and intra alveolar hemorrhage. Chest pain caused by rib fracture makes the patients afraid to take a deep breath and cough, instead rapid shallow breathing [5,6]. If it is not treated timely, it is easy to cause ARDS or different degree of pulmonary atelectasis, pulmonary infection, and pleural effusion. It is reported that 64% of patients with multiple rib fractures without anatomical reset have long-term persistent chest pain and other sequel [7].
Materials and Methods
Patients
A total of 44 pleural effusion patients caused by multiple rib fractures admitted in hospital from January 2013 to January 2015 were enrolled in this study. Pleural effusion occurred in 44 cases, accounting for 68.7% of the total number of cases. In the 44 cases, 24 cases were males and 20 cases were females. The oldest age was 70 years old, the youngest age was 20 years old, and the average age is 45 years old. Two cases died from ARDS, accounting for 4.58% of numbers of pleural effusion cases. Prior written and informed consent were obtained from every patient and the study was approved by the ethics review board of Laiwu Hospital Affiliated to Taishan Medical University.
Clinical imaging
According to the principle of random voluntary choice for treatment, patients were divided into Com group (conventional medical treatment group) and Mon group (mechanical ventilation group), with 22 cases in each group. There were no significant differences in clinical data between the two groups (P>0.05). Patients in Com group were given conventional medical treatment and those in Mon group were given conventional medical therapy combined with mechanical ventilation. Chest CT and chest three-dimensional reconstruction (VRT) was performed at day 0, day 2, day 4 and day 6 of hospitalization. Scanning parameters: 120 kV, 220 mA, thickness 5 mm, pitch 1. CT value was used to show the performance of fracture healing. CT value=α × (μm-μw)/μw. Note: The factor μm stands for the absorption coefficient (m) of the material and the factor μw stands for the water absorption coefficient (W). The factor α is the indexing factor and its value is 1000.
Colorimetric method
The pleural effusion was collected under guidance of color Doppler ultrasound. The activity of lactate dehydrogenase was detected by colorimetric method.
Statistical analysis
Data was analyzed by SPSS 13.0 software. Normality and homogeneity of variance test were firstly performed. If the data was in normal distribution and homogeneity of variance, single factor analysis of variance was used for comparing data among different groups at the same time point, and, the Q test was used for comparing data from the same group at different time points. Otherwise, Dunnett's T3 test was performed. P<0.05 were considered to be statistically significant.
Results
General clinical manifestations
The general clinical manifestations were observed. Before treatment, the patients of each group all had different degrees of chest pain, and the pain got intensified with cough, deep breathing or body rotation. After treatment, the symptoms of chest pain and dyspnea in Mon group were milder than that in Com group.
Manifestations on chest X-ray
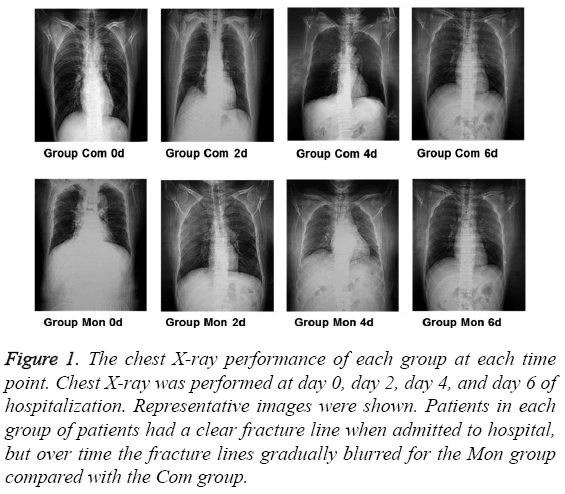
To observe the fracture line, chest X-ray was performed. As shown in Figure 1, patients of each group had a clear fracture line when admitted to hospital. However, after treatment, the fracture lines gradually blurred for the Mon group compared with the Com group.
Figure 1: The chest X-ray performance of each group at each time point. Chest X-ray was performed at day 0, day 2, day 4, and day 6 of hospitalization. Representative images were shown. Patients in each group of patients had a clear fracture line when admitted to hospital, but over time the fracture lines gradually blurred for the Mon group compared with the Com group.
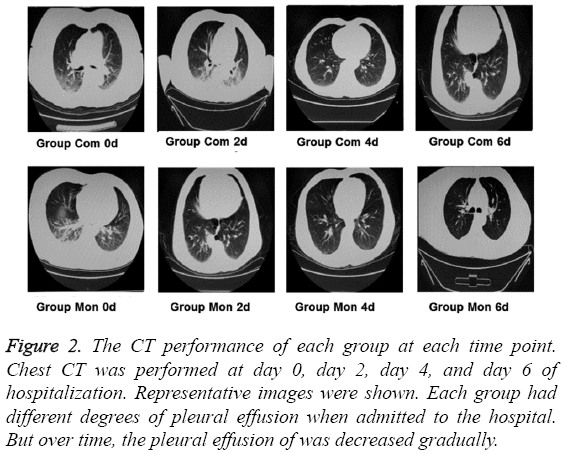
Manifestations on chest CT
To observe the pleural effusion, chest CT was carried out. CT value was calculated. As shown in Figure 2, patients in each group had different degrees of pleural effusion when admitted to the hospital. However, in the Mon group, the pleural effusion of was decreased gradually over time. Similarly, the CT value of the Mon group was similar to that of the Com group (Table 1). After treatment, the CT values of the Mon group and the Com group were significantly decreased at day 2, 4, and 6 of hospitalization than those at day 0 (P<0.05). Compared with the Com group, the CT values of the Mon group were significantly lower at day 2, 4, and 6 of hospitalization (P<0.05).
| Group | CT value | |||
|---|---|---|---|---|
| 0 d | 2 d | 4 d | 6 d | |
| Com | 24.0±2.1 | 22.0±2.2bc | 18.0±2.7bc | 18.0±1.6bc |
| Mon | 24.0±2.3 | 20.0±1.8ac | 17.0±2.0ac | 16.0±2.3ac |
Table 1: The comparison of CT value of pleural effusion in each group at each time point (Hu, mean ± SD, n=22).
Figure 2: The CT performance of each group at each time point. Chest CT was performed at day 0, day 2, day 4, and day 6 of hospitalization. Representative images were shown. Each group had different degrees of pleural effusion when admitted to the hospital. But over time, the pleural effusion of was decreased gradually.
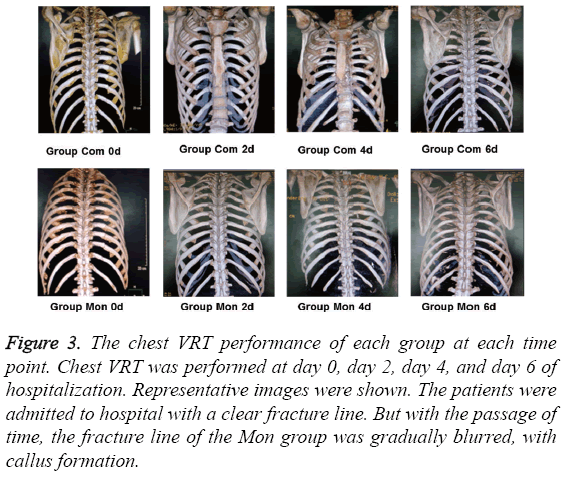
Manifestations on chest VRT
To further analyze fracture line, patients were examined with VRT. CT value was calculated. The patients of both groups were admitted to hospital with a clear fracture line (Figure 3). The CT value of the two groups was not statistically significant (P>0.05) (Table 2). But with the passage of time, the fracture line of the Mon group was gradually blurred, with callus formation. The CT value of the bone tissue gradually increased (P<0.05) and was more direct than the chest X-ray. There were significant differences between different groups and different time points (P<0.05).
| Group | CT value | |||
|---|---|---|---|---|
| 0d | 2d | 4d | 6d | |
| Com | 382.0±2.8 | 421.3±2.7bc | 453.6±2.7bc | 493.0±2.8bc |
| Mon | 382.1±3.6 | 443.5±1.4ac | 463.7±2.0ac | 512.1±3.7ac |
Table 2: The comparison of CT value in each group at each time point (Hu, mean ± SD, n=22).
Figure 3: The chest VRT performance of each group at each time point. Chest VRT was performed at day 0, day 2, day 4, and day 6 of hospitalization. Representative images were shown. The patients were admitted to hospital with a clear fracture line. But with the passage of time, the fracture line of the Mon group was gradually blurred, with callus formation.
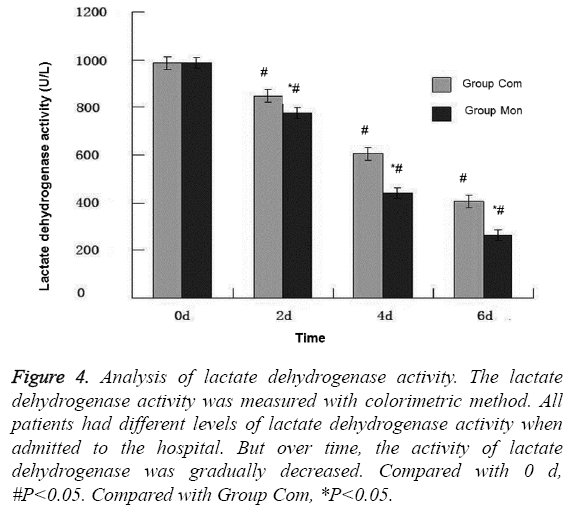
Lactate dehydrogenase activity examination
The lactate dehydrogenase activity was measured with colorimetric method. As shown in Figure 4, all patients had similar levels of lactate dehydrogenase activity when admitted to the hospital (P>0.05). But over time, the activity of lactate dehydrogenase was gradually decreased. The activity of lactate dehydrogenase in Mon group was significantly lower than that in Com group (P<0.05).
Figure 4: Analysis of lactate dehydrogenase activity. The lactate dehydrogenase activity was measured with colorimetric method. All patients had different levels of lactate dehydrogenase activity when admitted to the hospital. But over time, the activity of lactate dehydrogenase was gradually decreased. Compared with 0 d, #P<0.05. Compared with Group Com, *P<0.05.
Discussion
The incidence rate of rib fracture in closed thoracic trauma was 85%, and the common cause of injury was road traffic injury, falling injury, indirect crush injury, direct violence injury, etc. In clinical, there are types of single or multiple fractures of ribs and a plurality of multiple rib fractures. Flail chest is one special type, namely continuous 3 or more than 3 root ribs with multiple fractures [8]. According to statistics, the incidence of flail chest blunt trauma in the chest wall is in about 10%-15% and the total mortality rate is as high as 16%-20% [9]. Rib fracture is the main reason of the combined lung contusion and laceration, and liquid pneumothorax. If the treatment is not timely performed, it could cause chest pain, deformity and other complications [10].
There are mainly 3 conventional treatment methods for rib fracture. Firstly, the chest wall external fixation. Chest wall external fixation after rib fracture can reduce the chest injury and is an important part of subsequent treatment [11]. Chest wall external fixation is used for multiple rib fractures or flail chest and can reduce pain and correct abnormal breathing. After external fixation, there is significantly improvement for the respiratory function in patients and the chest deformity is not obvious. Therefore, it is very important to diagnose rib fractures. Chest X-ray is not good due to the poor location of ribs, often leading to the misdiagnosis or missed diagnosis of occult fractures [12]. Multi slice spiral CT has the advantages of larger range, thinner layer, higher resolution scanning and three-dimensional reconstruction, which can effectively solve the problem of rib fracture in X-ray diagnosis of rib [13]. This study shows that each group had different degree of fracture line when the patients just admitted. With the passage of time, the fracture line gradually blurred. The healing of multiple rib fracture is also associated with the site of trauma, age and other factors. Duane et al. [14] found that the first and second rib fractures often had severe chest trauma and could lead to fatal vascular injury or tracheal injury. The risk of multiple rib fractures in the elderly is 2~2.5 times to that of young people [15-17]. There is a need to pay special attention to children's rib fractures. Due to the low content of calcium, children's chest has a greater flexibility and more prone to deformation [18,19].
The second method is analgesia. Rib fracture causes severe pain, increases pulmonary infection probability in patients, and affects respiratory function and fracture recovery, especially for flail chest patients. The analgesia to fracture of the rib should be given, and full analgesia can obviously reduce the complications and improve the prognosis. Commonly used analgesic methods include oral analgesics, intercostal nerve block, intravenous analgesia, epidural analgesia etc. There are also pleural and epidural analgesia to treat multiple rib fracture [20]. The effect of continuous thoracic spinal anesthesia is reported to be similar to that of continuous epidural analgesia by Davies et al. [21].
The third conventional treatment method is mechanical ventilation. Mechanical ventilation can significantly improve the hypoxemia of the patients, correct paradoxical respiration, and treat the pulmonary atelectasis. The indication for mechanical ventilation is that the number of rib fracture is more than or equal to 8, severe pulmonary contusion, traumatic brain injury, and poor ventilation and oxygenation by humidification oxygen. The specific indicators: tidal volume<5 ml/kg, respiratory frequency>35 times/min, PCO2 > 55 mmHg, and arterial oxygen saturation level< 90%. Mechanical ventilation is divided into conventional mechanical ventilation, no plane mask ventilation, continuous airway positive pressure (CPAP), and intermittent airway positive pressure ventilation (IPAP), etc. There are reports about [22] the application of noninvasive external persistent negative pressure ventilation (CNEP) in treatment of flail chest. Our study mainly used CNEP treatment. The results showed that with the passage of time, the symptoms of chest pain and dyspnea in Mon group were lower than that in Com group. The X-ray performance of Mon group was more obscure than that in Com group. The pleural effusion in Mon group was decreased gradually compared with Com group, and the chest CT value was decreased. The chest VRT showed that compared with the Com group, fracture lines in Mon group blurred gradually, and the chest CT value increased gradually, and more intuitive compared with the chest X-ray. The biochemical lactate dehydrogenase activity of pleural effusion in Mon group decreased gradually (P< 0.05) compared with that of Com group.
In summary, our findings suggest that mechanical ventilation can promote the healing of the rib fracture and reduce the complications.
References
- Morimoto Y, Sugimoto T, Sakahira H, Matsuoka H, Yoshioka Y, Arase H. Successful management of threatened aortic rupture late after rib fracture caused by blunt chest trauma. Ann Vascular Surg 2014; 28: 1035. e1011-1035. e1013.
- Boyles AD, Taylor BC, Ferrel JR. Posterior rib fractures as a cause of delayed aortic injury: a case series and literature review. Injury Extra 2013; 44: 43-45.
- Hwang EG, Lee Y. Effectiveness of intercostal nerve block for management of pain in rib fracture patients. J Exerc Rehabil 2014; 10: 241-244.
- Ren Y, Zhang C. Treatment and care for traumatic flail chest. J Med Theory Practice 2011; 24: 842-843.
- Wang H, Zhang M, Liu H, Yang Z, He G, Zeng Y. Minimally invasive treatment for plurality multiple rib fractures and flail chest. Chinese J Clin Thoracic Cardiovascular Surg 2014; 16: 449-450.
- Jiao X, Yin X, Li Y. Effects of surgery and conservative treatment on pulmonary function of patients with multiple rib fractures. J Chinese Physician 2014; 16: 418-520.
- Helzel I, Long W, Fitzpatrick D, Madey S, Bottlang M. Evaluation of intramedullary rib splints for less-invasive stabilisation of rib fractures. Injury 2009; 40: 1104-1110.
- Al-Koudmani I, Darwish B, Al-Kateb K, Taifour Y. Chest trauma experience over eleven-year period at al-mouassat university teaching hospital-Damascus: a retrospective review of 888 cases. J Cardiothorac Surg 2012; 7: 35.
- Borrelly J, Aazami MH. New insights into the pathophysiology of flail segment: the implications of anterior serratus muscle in parietal failure. Euro J Cardiothoracic Surg 2005; 28: 742-749.
- Gordy S, Fabricant L, Ham B, Mullins R, Mayberry J. The contribution of rib fractures to chronic pain and disability. Am J Surg 2014; 207: 659-662.
- Mayberry JC, Ham LB, Schipper PH, Ellis TJ, Mullins RJ. Surveyed opinion of American trauma, orthopedic, and thoracic surgeons on rib and sternal fracture repair. J Trauma Acute Care Surg 2009; 66: 875-879.
- Hu J. Causes of misdiagnosis for multiple rib fractures. J Practical Radiol 2003; 19: 765-767.
- Pretorius ES, Fishman EK. Helical (spiral) CT of the musculoskeletal system. Radiol Clin North Am 1995; 33: 949-979.
- Duane TM, O'Connor JV, Scalea TM. Thoracic outlet syndrome resulting from first rib fracture. J Trauma 2007; 62: 231-233.
- Rauchwerger JJ, Candido KD, Deer TR, Frogel JK, Iadevaio R. Thoracic epidural steroid injection for rib fracture pain. Pain Pract 2013; 13: 416-421.
- Maxwell CA, Mion LC, Dietrich MS. Hospitalized injured older adults: clinical utility of a rib fracture scoring system. J Trauma Nurs 2012; 19: 168-174.
- Li A. Treatment of elderly chest trauma and prevention of pulmonary complications. China J Clin Med 2009; 37: 61-62.
- Holmes JF, Sokolove PE, Brant WE, Kuppermann N. A clinical decision rule for identifying children with thoracic injuries after blunt torso trauma. Ann Emerg Med 2002; 39: 492-499.
- Williams RL, Connolly PT. In children undergoing chest radiography what is the specificity of rib fractures for non-accidental injury? Arch Dis Child 2004; 89: 490-492.
- Shinohara K, Iwama H, Akama Y, Tase C. Interpleural block for patients with multiple rib fractures: comparison with epidural block. J Emerg Med 1994; 12: 441-446.
- Davies R, Myles P, Graham J. A comparison of the analgesic efficacy and side-effects of paravertebral vs epidural blockade for thoracotomy-a systematic review and meta-analysis of randomized trials. Br J Anaesth 2006; 96: 418-426.
- Linton DM, Sviri S. Conservative management of flail chest after cardiopulmonary resuscitation by continuous negative extrathoracic pressure. Crit Care Resusc 2006; 8: 339-340.